J Korean Med Sci.
2024 Nov;39(44):e284. 10.3346/jkms.2024.39.e284.
Similar but Distinct Comorbidity Patterns Between Polycystic Ovary Syndrome and Endometriosis in Korean Women: A Nationwide Cohort Study
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Korea University College of Medicine, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea
- 3Computational Biology Department, Carnegie Mellon University, Pittsburgh, PA, USA
- 4Department of Statistics, Korea University, Seoul, Korea
- 5Department of Digital Health, Samsung Advanced Institute for Health Sciences & Technology (SAIHST), Samsung Medical Center, Sungkyunkwan University, Seoul, Korea
- KMID: 2561466
- DOI: http://doi.org/10.3346/jkms.2024.39.e284
Abstract
- Background
Polycystic ovary syndrome (PCOS) and endometriosis are widely recognized as significant risk factors affecting the reproductive health of women. The underlying mechanisms impacting fertility may vary, potentially leading to divergent outcomes. We aimed to examine and contrast the prevalence patterns of diseases coexisting with PCOS and endometriosis, using a large-scale nationwide insurance claims data from Asian women of reproductive age.
Methods
We analyzed health insurance and examination data of 157,662 Korean women aged 15–45 years, drawn from the Korea National Health Insurance Service-National Sample Cohort database. International Classification of Disease, Tenth Revision codes were mapped to phenome-wide association study codes (phecodes). Subsequently, multivariate logistic regression was performed to assess the comorbidity patterns among patients diagnosed with PCOS and endometriosis and healthy control groups.
Results
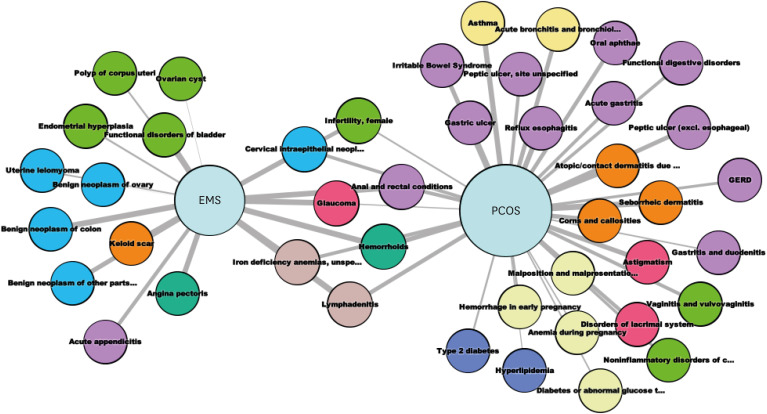
Our analysis revealed that PCOS was correlated with a wider range of metabolic disorders and symptoms, such as hyperlipidemia, type 2 diabetes, various gastrointestinal (GI) issues, and an array of pregnancy-related complications. Conversely, endometriosis was more prevalent among benign neoplasms of female reproductive and digestive organs, endometrial hyperplasia, and angina pectoris. Notably, infertility and glaucoma demonstrated significant associations with both conditions. Furthermore, a comparison of symptom-related codes in women with endometriosis revealed a predominance of painrelated symptoms, whereas those with PCOS exhibited a broader spectrum, encompassing pain, pruritus, GI problems, cough, fever, menstrual cycle disorders, edema, and dizziness.
Conclusion
PCOS and endometriosis, which are prevalent gynecological disorders affecting similar age groups of women, rarely co-occur and exhibit unique comorbidity profiles. Tailored healthcare strategies that take into account these distinct patterns have the potential to enhance long-term healthcare outcomes of affected patients. Further research is required to elucidate the underlying mechanisms and contrasting comorbidity profiles between PCOS and endometriosis.
Keyword
Figure
Reference
-
1. Ehrmann DA. Polycystic ovary syndrome. N Engl J Med. 2005; 352(12):1223–1236. PMID: 15788499.2. Horne AW, Missmer SA. Pathophysiology, diagnosis, and management of endometriosis. BMJ. 2022; 379:e070750. PMID: 36375827.3. Kim H, Lee M, Hwang H, Chung YJ, Cho HH, Yoon H, et al. The estimated prevalence and incidence of endometriosis with the Korean National Health Insurance Service-National Sample Cohort (NHIS-NSC): a national population-based study. J Epidemiol. 2021; 31(12):593–600. PMID: 32863371.4. Ryu KJ, Kim MS, Kim HK, Kim YJ, Yi KW, Shin JH, et al. Risk of type 2 diabetes is increased in nonobese women with polycystic ovary syndrome: the National Health Insurance Service-National Sample Cohort Study. Fertil Steril. 2021; 115(6):1569–1575. PMID: 33509630.5. Becker CM, Bokor A, Heikinheimo O, Horne A, Jansen F, Kiesel L, et al. ESHRE guideline: endometriosis. Hum Reprod Open. 2022; 2022(2):hoac009. PMID: 35350465.6. Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. 2018; 110(3):364–379. PMID: 30033227.7. Bonavina G, Taylor HS. Endometriosis-associated infertility: from pathophysiology to tailored treatment. Front Endocrinol (Lausanne). 2022; 13:1020827. PMID: 36387918.8. Kvaskoff M, Mu F, Terry KL, Harris HR, Poole EM, Farland L, et al. Endometriosis: a high-risk population for major chronic diseases? Hum Reprod Update. 2015; 21(4):500–516. PMID: 25765863.9. Dinsdale NL, Crespi BJ. Endometriosis and polycystic ovary syndrome are diametric disorders. Evol Appl. 2021; 14(7):1693–1715. PMID: 34295358.10. Denny JC, Ritchie MD, Basford MA, Pulley JM, Bastarache L, Brown-Gentry K, et al. PheWAS: demonstrating the feasibility of a phenome-wide scan to discover gene-disease associations. Bioinformatics. 2010; 26(9):1205–1210. PMID: 20335276.11. Bush WS, Oetjens MT, Crawford DC. Unravelling the human genome-phenome relationship using phenome-wide association studies. Nat Rev Genet. 2016; 17(3):129–145. PMID: 26875678.12. Hebbring SJ. The challenges, advantages and future of phenome-wide association studies. Immunology. 2014; 141(2):157–165. PMID: 24147732.13. Pendergrass SA, Brown-Gentry K, Dudek SM, Torstenson ES, Ambite JL, Avery CL, et al. The use of phenome-wide association studies (PheWAS) for exploration of novel genotype-phenotype relationships and pleiotropy discovery. Genet Epidemiol. 2011; 35(5):410–422. PMID: 21594894.14. Joo YY, Pacheco JA, Thompson WK, Rasmussen-Torvik LJ, Rasmussen LV, Lin FT, et al. Multi-ancestry genome- and phenome-wide association studies of diverticular disease in electronic health records with natural language processing enriched phenotyping algorithm. PLoS One. 2023; 18(5):e0283553. PMID: 37196047.15. Yu KH, Miron O, Palmer N, Lemos DR, Fox K, Kou SC, et al. Data-driven analyses revealed the comorbidity landscape of tuberous sclerosis complex. Neurology. 2018; 91(21):974–976. PMID: 30333165.16. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID: 26822938.17. Wekker V, van Dammen L, Koning A, Heida KY, Painter RC, Limpens J, et al. Long-term cardiometabolic disease risk in women with PCOS: a systematic review and meta-analysis. Hum Reprod Update. 2020; 26(6):942–960. PMID: 32995872.18. Poeta do Couto C, Policiano C, Pinto FJ, Brito D, Caldeira D. Endometriosis and cardiovascular disease: a systematic review and meta-analysis. Maturitas. 2023; 171:45–52. PMID: 37075537.19. Lin KY, Yang CY, Lam A, Chang CY, Lin WC. Uterine leiomyoma is associated with the risk of developing endometriosis: a nationwide cohort study involving 156,195 women. PLoS One. 2021; 16(8):e0256772. PMID: 34437644.20. Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. Erratum. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2019; 34(2):388. PMID: 30521039.21. Ye J, Peng H, Huang X, Qi X. The association between endometriosis and risk of endometrial cancer and breast cancer: a meta-analysis. BMC Womens Health. 2022; 22(1):455. PMID: 36401252.22. Kim H, Kim HJ, Ahn HS. Does endometriosis increase the risks of endometrial hyperplasia and endometrial cancer? Gynecol Oncol. 2023; 169:147–153. PMID: 36357191.23. Balıkçı AT, Ulutaş HG, Özgen GA. Evaluation of meibomian gland morphology and anterior segment parameters by Sirius topography systems in polycystic ovary syndrome. Indian J Ophthalmol. 2022; 70(8):2922–2928. PMID: 35918944.24. Vergroesen JE, Kaynak A, Aribas E, Kavousi M, van Meurs JB, Klaver CC, et al. Higher testosterone is associated with open-angle glaucoma in women: a genetic predisposition? Biol Sex Differ. 2023; 14(1):27. PMID: 37161452.25. Wang YE, Kakigi C, Barbosa D, Porco T, Chen R, Wang S, et al. Oral contraceptive use and prevalence of self-reported glaucoma or ocular hypertension in the United States. Ophthalmology. 2016; 123(4):729–736. PMID: 26948305.26. Pasquale LR, Kang JH. Female reproductive factors and primary open-angle glaucoma in the Nurses’ Health Study. Eye (Lond). 2011; 25(5):633–641. PMID: 21336255.27. Hogden K, Mikelberg F, Sodhi M, Khosrow-Khavar F, Mansournia MA, Kezouh A, et al. The association between hormonal contraceptive use and glaucoma in women of reproductive age. Br J Clin Pharmacol. 2021; 87(12):4780–4785. PMID: 34159623.28. Kałużna M, Kompf P, Wachowiak-Ochmańska K, Moczko J, Królczyk A, Janicki A, et al. Are patients with polycystic ovary syndrome more prone to irritable bowel syndrome? Endocr Connect. 2022; 11(4):e210309. PMID: 35275093.29. Kollmann M, Klaritsch P, Martins WP, Guenther F, Schneider V, Herzog SA, et al. Maternal and neonatal outcomes in pregnant women with PCOS: comparison of different diagnostic definitions. Hum Reprod. 2015; 30(10):2396–2403. PMID: 26223675.30. Crespi B. Variation among human populations in endometriosis and PCOS A test of the inverse comorbidity model. Evol Med Public Health. 2021; 9(1):295–310. PMID: 34659773.31. Dinsdale N, Nepomnaschy P, Crespi B. The evolutionary biology of endometriosis. Evol Med Public Health. 2021; 9(1):174–191. PMID: 33854783.32. Christakou CD, Diamanti-Kandarakis E. Role of androgen excess on metabolic aberrations and cardiovascular risk in women with polycystic ovary syndrome. Womens Health (Lond). 2008; 4(6):583–594. PMID: 19072461.33. Guan C, Zahid S, Minhas AS, Ouyang P, Vaught A, Baker VL, et al. Polycystic ovary syndrome: a “risk-enhancing” factor for cardiovascular disease. Fertil Steril. 2022; 117(5):924–935. PMID: 35512976.34. Crespi BJ, Evans SF. Prenatal origins of endometriosis pathology and pain: reviewing the evidence of a role for low testosterone. J Pain Res. 2023; 16:307–316. PMID: 36762368.35. Islam RM, Bell RJ, Handelsman DJ, McNeil JJ, Nelson MR, Reid CM, et al. Associations between blood sex steroid concentrations and risk of major adverse cardiovascular events in healthy older women in Australia: a prospective cohort substudy of the ASPREE trial. Lancet Healthy Longev. 2022; 3(2):e109–e118. PMID: 35252940.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Studies on Fibrinolytic System Behavior in Women with Polycystic Ovary Syndrome
- Analysis of LHbeta Exon 3 (Gly102Ser) Gene Mutation in Infertile Patients with Endometriosis and Polycystic Ovary Syndrome (PCOS)
- Inter-ovarian differences in ultrasound markers of ovarian size in women with polycystic ovary syndrome
- Medical diagnosis and treatment of polycystic ovary syndrome
- Polycystic Ovary Syndrome and Women Health