Ewha Med J.
2024 Oct;47(4):e57. 10.12771/emj.2024.e57.
Septic cerebral embolism following lumbar spine surgery in a 69-year-old man with a lumbar epidural abscess in Korea: a case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kyung Hee University Hospital at Gangdong, Kyung Hee University College of Medicine, Seoul, Korea
- KMID: 2561420
- DOI: http://doi.org/10.12771/emj.2024.e57
Abstract
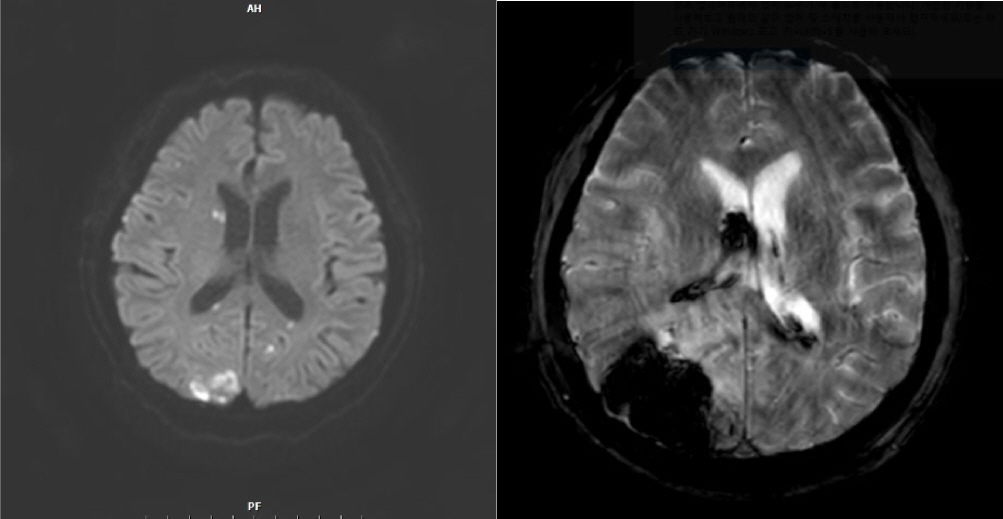
- Septic embolism and stroke are serious complications in patients with sepsis and often necessitate urgent surgical intervention to control the source of infection. A 69-year-old man presented with severe pain in his back and left thigh. MRI revealed extensive posterior epidural or subdural abscesses extending from the cervical to the lumbar level, as well as an abscess in the iliopsoas muscle. The patient underwent urgent drainage of the abscesses and decompression of the lumbar spine. Postoperatively, he developed sudden-onset atrial fibrillation and altered mental status. Brain CT showed multiple embolic infarctions. His condition deteriorated due to persistent infection, leading to disseminated intravascular coagulation, acute kidney injury, and septic shock. This case highlights the risk of cerebral embolism and hemorrhagic complications in patients with sepsis who undergo surgery. Early recognition of individuals at high risk and comprehensive perioperative management are critical to reducing the likelihood of such complications.
Figure
Reference
-
References
1. Yuki K, Murakami N. Sepsis pathophysiology and anesthetic consideration. Cardiovasc Hematol Disord Drug Targets. 2015; 15(1):57–69. DOI: 10.2174/1871529X15666150108114810. PMID: 25567335. PMCID: PMC4704087.
Article2. Scheggi V, Menale S, Tonietti B, Bigiarini C, Giovacchini J, Del Pace S, et al. Impact of septic cerebral embolism on prognosis and therapeutic strategies of infective endocarditis: a retrospective study in a surgical centre. BMC Infect Dis. 2022; 22(1):554. DOI: 10.1186/s12879-022-07533-w. PMID: 35715766. PMCID: PMC9206378.
Article3. Woida TR, Cornejo K, Lin A, Cipriano A, Nanda S, Amortegui JD, et al. Septic embolism: a potentially devastating complication of infective endocarditis. In. Firstenberg MS, editor. editor. Contemporary challenges in endocarditis. London: IntechOpen;2016. DOI: 10.5772/64931.
Article4. Allegrini D, Reposi S, Nocerino E, Pece A. Odontogenic orbital cellulitis associated with cavernous sinus thrombosis and pulmonary embolism: a case report. J Med Case Rep. 2017; 11(1):164. DOI: 10.1186/s13256-017-1309-0. PMID: 28629401. PMCID: PMC5477346.
Article5. Shao IY, Elkind MSV, Boehme AK. Risk factors for stroke in patients with sepsis and bloodstream infections. Stroke. 2019; 50(5):1046–1051. DOI: 10.1161/STROKEAHA.118.023443. PMID: 30896327. PMCID: PMC6476655.
Article6. Kaukonen KM, Bailey M, Pilcher D, Cooper DJ, Bellomo R. Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med. 2015; 372(17):1629–1638. DOI: 10.1056/NEJMoa1415236. PMID: 25776936.
Article7. Jones HR Jr, Siekert RG. Neurological manifestations of infective endocarditis: review of clinical and therapeutic challenges. Brain. 1989; 112(5):1295–1315. DOI: 10.1093/brain/112.5.1295. PMID: 2679968.8. Chan KL, Tam J, Dumesnil JG, Cujec B, Sanfilippo AJ, Jue J, et al. Effects of long-term aspirin use on embolic events in infective endocarditis. Clin Infect Dis. 2008; 46(1):37–41. DOI: 10.1086/524021. PMID: 18171211.
Article9. Hall MJ, Williams SN, DeFrances CJ, Golosinskiy A. Inpatient care for septicemia or sepsis: a challenge for patients and hospitals. NCHS Data Brief. 2011; (62):1–8.10. Voulgareli I, Chronaiou A, Tsoukalas D, Tsoukalas G. A rare case of lipoid pneumonia attributed to amiodarone. Pneumonia. 2018; 10:12. DOI: 10.1186/s41479-018-0056-3. PMID: 30534512. PMCID: PMC6280337.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Lumbar Epidural Abscess Combined with Cauda Equina Syndrome: Case Report
- Lumbar Spinal Epidural Abscess Combined with Cauda Equina Syndrome: A Case Report
- Rapidly Progressive Gas-containing Lumbar Spinal Epidural Abscess
- Tophaceous Gout of the Lumbar Spine Mimicking Infectious Spondylodiscitis and Epidural Abscess
- Intradural Lumbar Disc Herniations Associated with Epidural Adhesion : Report of Two Cases