Ewha Med J.
2024 Oct;47(4):e70. 10.12771/emj.2024.e70.
Prevalence and associated factors of ADHD-like symptoms among pharmacy students at Prince of Songkla University, Thailand in 2024: a crosssectional study
- Affiliations
-
- 1Department of Social and Administrative Pharmacy, Faculty of Pharmaceutical Sciences, Prince of Songkla University, Songkhla, Thailand
- KMID: 2561417
- DOI: http://doi.org/10.12771/emj.2024.e70
Abstract
Objectives
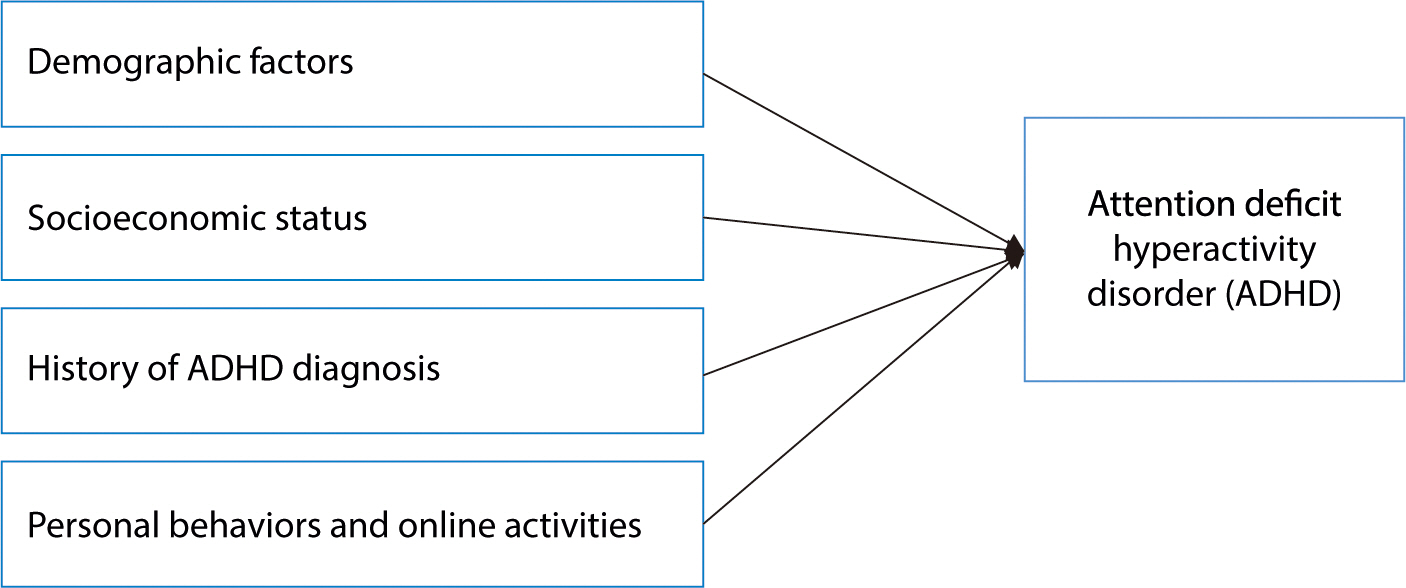
This study investigated the prevalence of attention-deficit hyperactivity disorder (ADHD) and its associated factors among pharmacy students at Prince of Songkla University in 2024. It was hypothesized that the prevalence of ADHD would be associated with various demographic, socioeconomic, historical, and behavioral factors.
Methods
This cross-sectional descriptive study involved pharmacy students from years 1–5 at Prince of Songkla University in Thailand. Data were gathered from 761 students using a self-administered questionnaire that included the Adult ADHD Self-Report Scale (ASRS Screener V1.1). Descriptive statistics, the chi-square test, the Fisher exact test, and multiple logistic regression were employed for data analysis.
Results
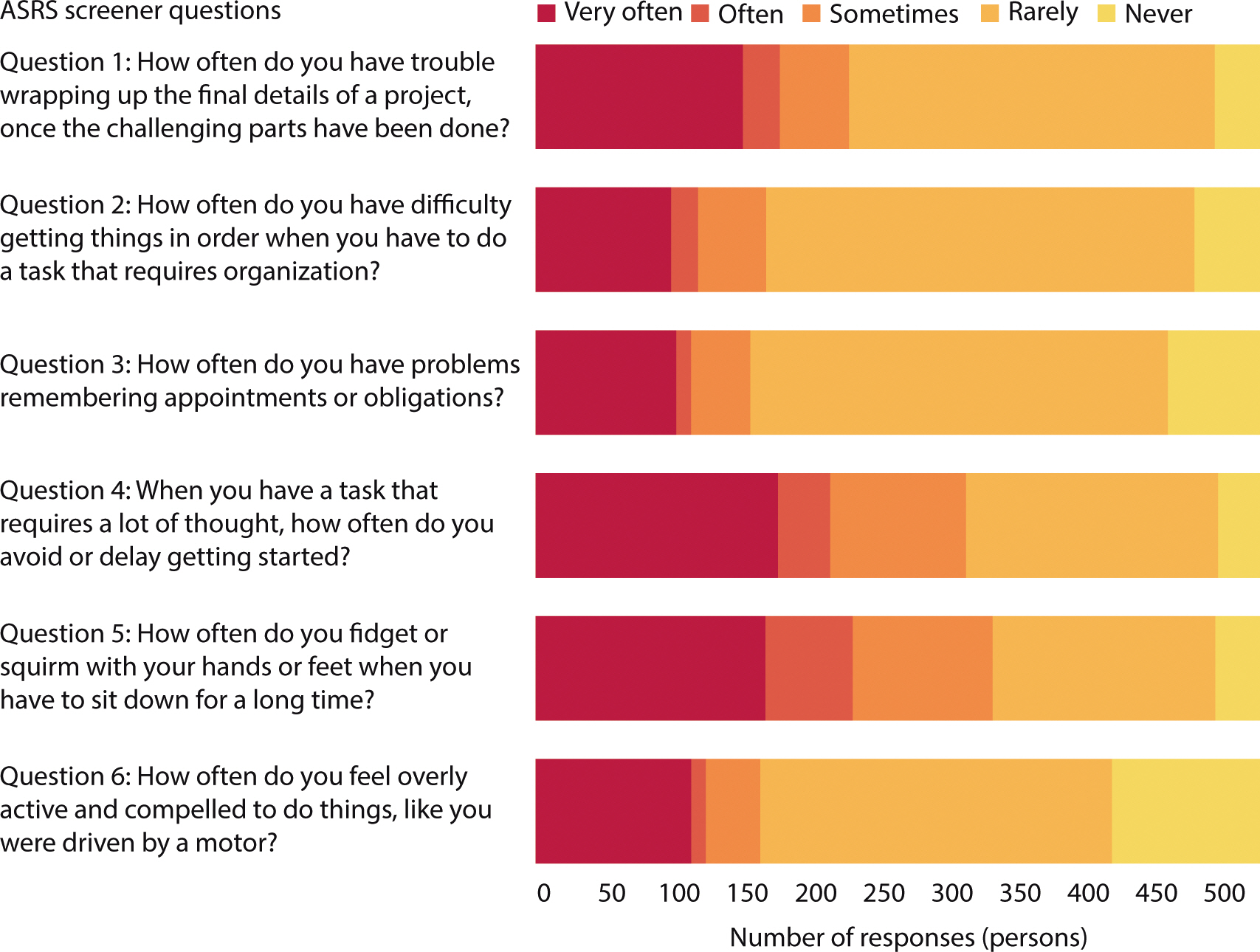
In total, 526 students participated in the study (participation rate: 69%), with an average age of 21±1.57 years. The risk of ADHD was prevalent in 14.4% of the respondents (76 students; 95% CI: 11.4%–17.5%). Significant factors associated with an increased risk of ADHD included identifying as not disclosed or preferring not to report gender (adjusted OR [OR adj ], 3.32; 95% CI, 1.04–10.57), having insufficient monthly income (OR adj , 2.02; 95% CI, 1.13–3.61), and recent traffic violations (OR adj , 2.02; 95% CI, 1.09–3.76). It was also found that difficulties with executive functioning, such as organization and procrastination, were highly prevalent among pharmacy students.
Conclusion
The study identified a substantial prevalence of ADHD risk among pharmacy students, with factors including gender, financial challenges, and behavioral patterns such as traffic violations significantly associated with this risk. These findings underscore the necessity for targeted mental health interventions in university settings.
Figure
Reference
-
References
1. Ayano G, Demelash S, Gizachew Y, Tsegay L, Alati R. The global prevalence of attention deficit hyperactivity disorder in children and adolescents: an umbrella review of meta-analyses. J Affect Disord. 2023; 339:860–866. DOI: 10.1016/j.jad.2023.07.071. PMID: 37495084.
Article2. Takeda T, Tsuji Y, Akatsu R, Nomura T. Initial impact of the COVID-19 outbreak on ADHD symptoms among university students in Japan. J Korean Acad Child Adolesc Psychiatry. 2023; 34(2):69–75. DOI: 10.5765/jkacap.220032. PMID: 37035788. PMCID: PMC10080255.
Article3. Charatcharoenwitthaya K. The impact of lockdown during COVID-19 pandemic on physical and mental health of adolescents. Siriraj Med J. 2022; 74(12):895–902. DOI: 10.33192/Smj.2022.105.
Article4. Thitamethee P, Likhitweerawong N, Louthrenoo O, Boonchooduang N. Chronic conditions and resilience: adolescent health behaviors in the midst of the COVID-19 pandemic in Thailand. Glob Pediatr Health. 2024; 11:2333794X241274732. DOI: 10.1177/2333794X241274732. PMID: 39246305. PMCID: PMC11378227.5. Wüstner A, Otto C, Schlack R, Hölling H, Klasen F, Ravens-Sieberer U. Risk and protective factors for the development of ADHD symptoms in children and adolescents: results of the longitudinal BELLA study. PLoS One. 2019; 14(3):0214412. DOI: 10.1371/journal.pone.0214412. PMID: 30908550. PMCID: PMC6433344.6. Ra CK, Cho J, Stone MD, De La Cerda J, Goldenson NI, Moroney E, et al. Association of digital media use with subsequent symptoms of attention-deficit/hyperactivity disorder among adolescents. JAMA. 2018; 320(3):255–263. DOI: 10.1001/jama.2018.8931. PMID: 30027248. PMCID: PMC6553065.
Article7. Shi M, Liu L, Sun X, Wang L. Associations between symptoms of attention-deficit/hyperactivity disorder and life satisfaction in medical students: the mediating effect of resilience. BMC Med Educ. 2018; 18(1):164. DOI: 10.1186/s12909-018-1261-8. PMID: 30005708. PMCID: PMC6043958.8. Kim DH, Lee HJ, Lin Y, Kang YJ. Changes in academic performance in the online, integrated system-based curriculum implemented due to the COVID-19 pandemic in a medical school in Korea. J Educ Eval Health Prof. 2021; 18:24. DOI: 10.3352/jeehp.2021.18.24. PMID: 34551511. PMCID: PMC8616727.
Article9. Bussaratid S, Atsariyasing W, Wannarit K, Pukrittayakami P, Hosiri T, Wiwatwararom N, et al. Reliability and validity study of adult ADHD Self-Report Scale (ASRS) screener v1. 1 Thai version. J Psychiatr Assoc Thailand. 2016; 61(2):145–154.10. Visanuyothin T, Wachiradilok P, Pavasuthiapaisit C. 597 – Prevalence of ADHD and ODD: a national survey in Thailand 2012. Eur Psychiatry. 2013; 28:Supplement 1. 1. DOI: 10.1016/S0924-9338(13)75869-3.11. Gimbach S, Vogel D, Fried R, Faraone SV, Banaschewski T, Buitelaar J, et al. ADHD medicine consumption in Europe after COVID-19: catch-up or trend change? BMC Psychiatry. 2024; 24(1):112. DOI: 10.1186/s12888-024-05505-9. PMID: 38336744. PMCID: PMC10854136.12. Rutherford L, Stark A, Ablona A, Klassen BJ, Higgins R, Jacobsen H, et al. Health and well-being of trans and non-binary participants in a community-based survey of gay, bisexual, and queer men, and non-binary and two-spirit people across Canada. PLoS One. 2021; 16(2):0246525. DOI: 10.1371/journal.pone.0246525. PMID: 33571252. PMCID: PMC7877578.13. Russell AE, Ford T, Russell G. Socioeconomic associations with ADHD: findings from a mediation analysis. PLoS One. 2015; 10(6):0128248. DOI: 10.1371/journal.pone.0128248. PMID: 26030626. PMCID: PMC4451079.14. Randell NJS, Charlton SG, Starkey NJ. Driving with ADHD: performance effects and environment demand in traffic. J Atten Disord. 2016; 24(11):1570–1580. DOI: 10.1177/1087054716658126. PMID: 27401237.
Article15. Paiboonsithiwong S, Kunanitthaworn N, Songtrijuck N, Wongpakaran N, Wongpakaran T. Learning styles, academic achievement, and mental health problems among medical students in Thailand. J Educ Eval Health Prof. 2016; 13:38. DOI: 10.3352/jeehp.2016.13.3. PMID: 26767720. PMCID: PMC4751292.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Venous air emboli during esophagoscopy confirmed by computed tomographic pulmonary angiography -a case report-
- Occupational Tasks Influencing Lung Function and Respiratory Symptoms Among Charcoal-Production Workers: A Time-Series Study
- ADHD and Its Comorbidities in College Students, with a Focus on Depression and Pathological Internet Use
- Response to: Management of Traumatic Spinal Fracture in the Coronavirus Disease 2019 Situation
- Response to: Management of Traumatic Spinal Fracture in the Coronavirus Disease 2019 Situation