Ewha Med J.
2024 Oct;47(4):e63. 10.12771/emj.2024.e63.
Early detection of patients with narcotic use disorder using a modified morphine equivalent daily dose score based on an analysis of real-world prescription patterns: a retrospective cohort study
- Affiliations
-
- 1Department of Environment Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 2Graduate Program in System Health Science and Engineering, Ewha Womans University College of Medicine, Seoul, Korea
- 3Department of Information Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2561414
- DOI: http://doi.org/10.12771/emj.2024.e63
Abstract
Objectives
Addiction to prescription narcotics is a global issue, and detecting individuals with narcotic use disorder (NUD) at an early stage can help prevent narcotics misuse and abuse. We developed a novel index for the early detection of NUD based on an analysis of real-world prescription patterns in a large hospital.
Methods
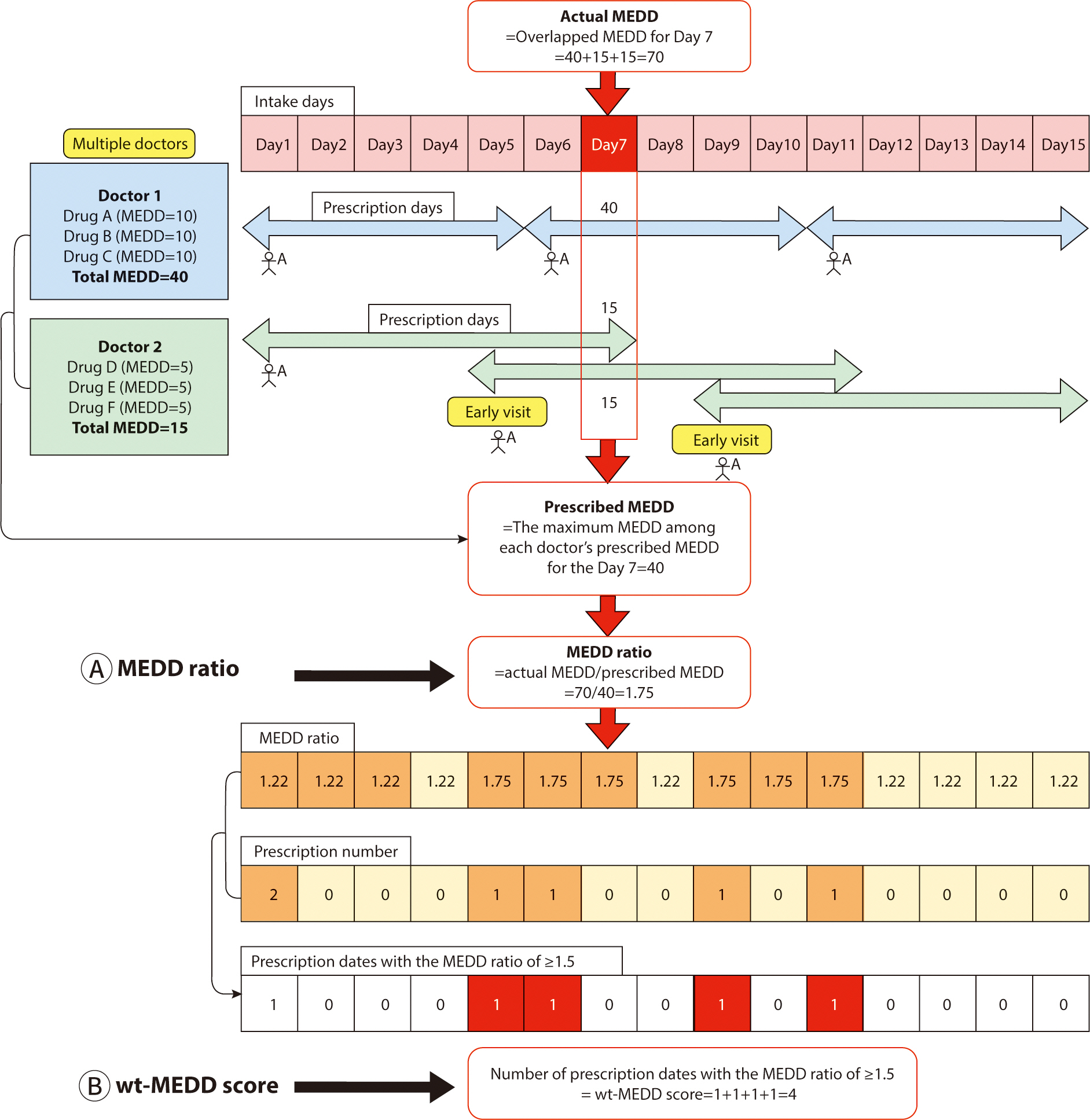
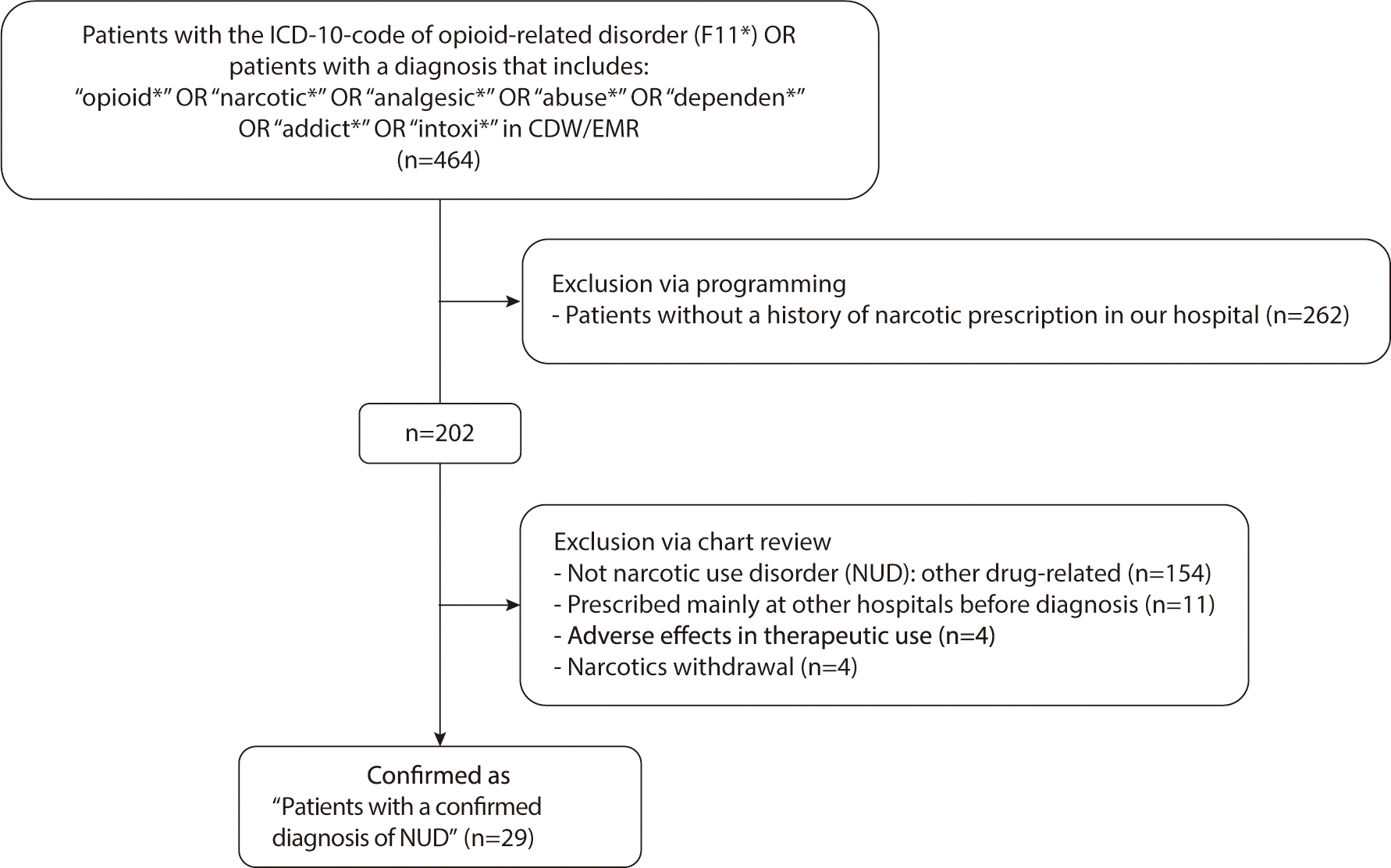
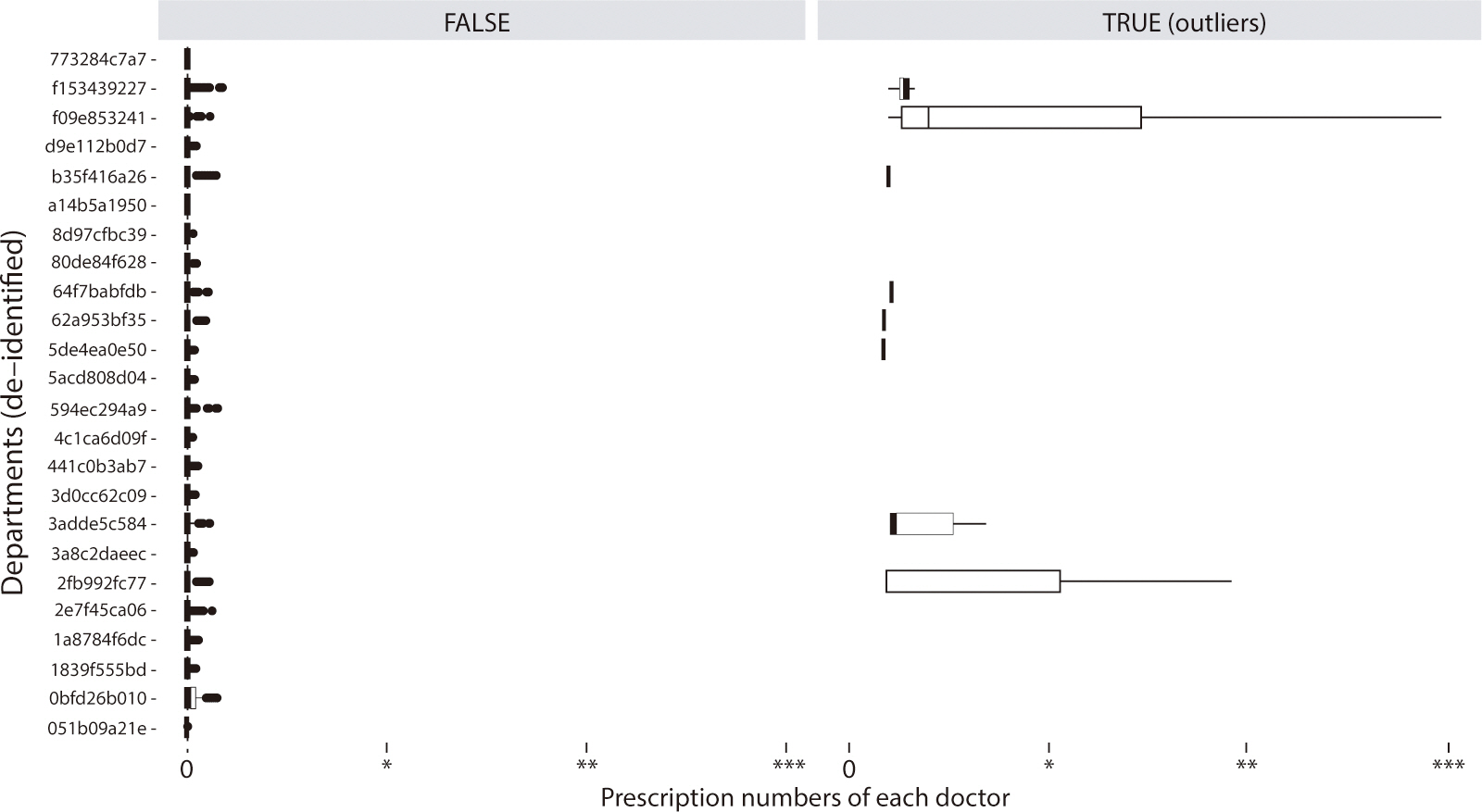
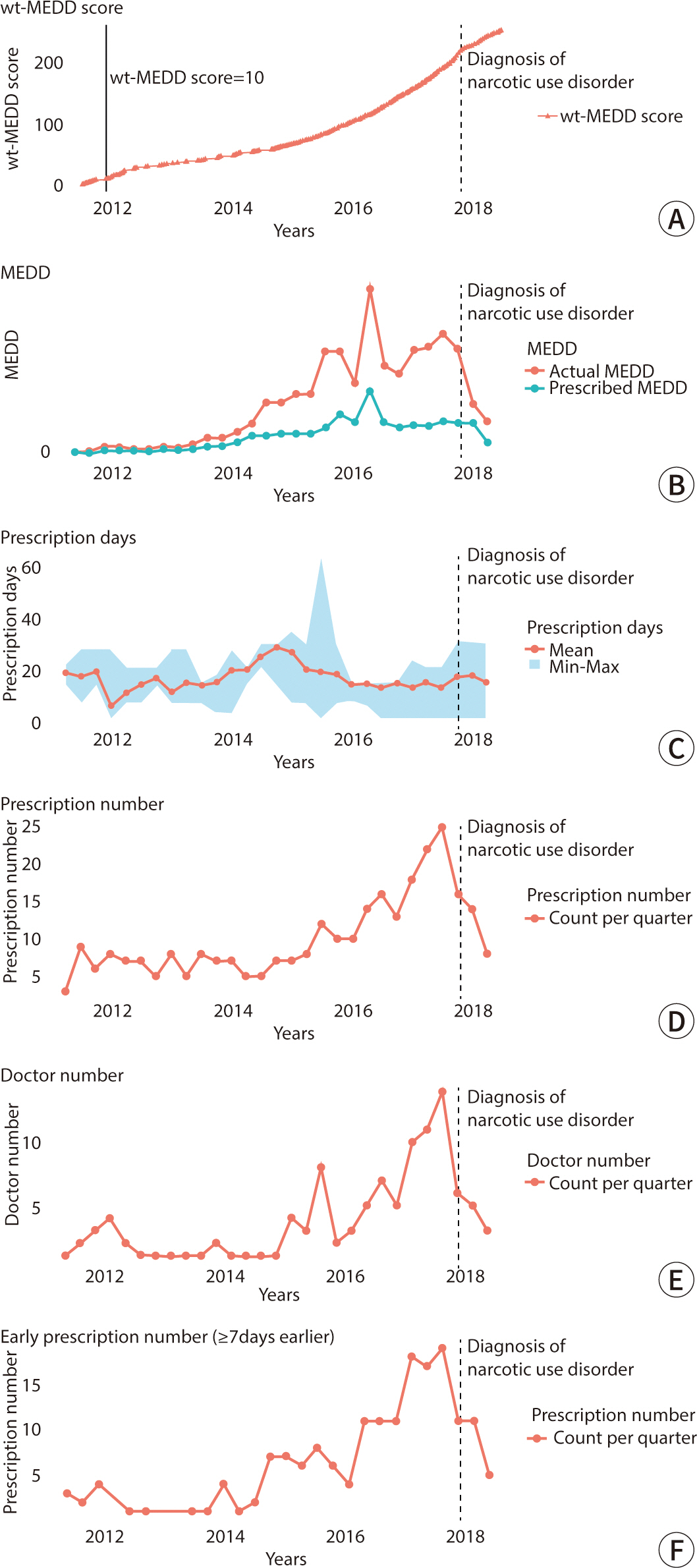
We analyzed the narcotic prescriptions of 221,887 patients, prescribed by 8,737 doctors from July 2000 to June 2018. To facilitate the early detection of patients at risk of developing NUD after a prolonged period of narcotic use, we developed a weighted morphine equivalent daily dose (wt-MEDD) score. This score was based on the number of prescription dates where the actual MEDD exceeded the intended MEDD. We compared the performance of the wt-MEDD scoring system in identifying patients diagnosed with NUD by doctors against other high-risk NUD indices. These indices included the MEDD scoring system, the number of days on prescribed narcotics, the frequency and duration of prescriptions, narcotics prescriptions from multiple doctors, and the number of early narcotic refills.
Results
A wt-MEDD score cut-off value of 10.5 successfully identified all outliers and diagnosed patients with NUD with 100% sensitivity and 99.6% specificity. This score demonstrated the highest sensitivity and specificity for detecting NUD compared to all other indexes. The predictive performance was further improved by combining the wt-MEDD score with other high-risk NUD indexes.
Conclusion
We developed a novel index, the wt-MEDD score, which showed excellent performance in the early detection of NUD.
Figure
Reference
-
References
1. United Nations Office on Drugs and Crime [UNODC]. Executive summary: conclusions and policy implications. New York: United Nations;2018.2. Sproule B, Brands B, Li S, Catz-Biro L. Changing patterns in opioid addiction: characterizing users of oxycodone and other opioids. Can Fam Physician. 2009; 55(1):68–69.e5.3. Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, van der Goes DN. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. PAIN. 2015; 156(4):569–576. DOI: 10.1097/01.j.pain.0000460357.01998.f1. PMID: 25785523.4. Califf RM, Woodcock J, Ostroff S. A proactive response to prescription opioid abuse. N Engl J Med. 2016; 374(15):1480–1485. DOI: 10.1056/NEJMsr1601307. PMID: 26845291.
Article5. Cochran G, Woo B, Lo-Ciganic WH, Gordon AJ, Donohue JM, Gellad WF. Defining nonmedical use of prescription opioids within health care claims: a systematic review. Subst Abuse. 2015; 36(2):192–202. DOI: 10.1080/08897077.2014.993491. PMID: 25671499. PMCID: PMC4736503.
Article6. Saunders JB. Substance use and addictive disorders in DSM-5 and ICD 10 and the draft ICD 11. Curr Opin Psychiatry. 2017; 30(4):227–237. DOI: 10.1097/YCO.0000000000000332. PMID: 28459730.
Article7. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain: United States, 2016. JAMA. 2016; 315(15):1624–1645. DOI: 10.1001/jama.2016.1464. PMID: 26977696. PMCID: PMC6390846.
Article8. Haffajee RL, Jena AB, Weiner SG. Mandatory use of prescription drug monitoring programs. JAMA. 2015; 313(9):891–892. DOI: 10.1001/jama.2014.18514. PMID: 25622279. PMCID: PMC4465450.
Article9. Delcher C, Wagenaar AC, Goldberger BA, Cook RL, Maldonado-Molina MM. Abrupt decline in oxycodone-caused mortality after implementation of Florida's Prescription Drug Monitoring Program. Drug Alcohol Depend. 2015; 150:63–68. DOI: 10.1016/j.drugalcdep.2015.02.010. PMID: 25746236.
Article10. Pardo B. Do more robust prescription drug monitoring programs reduce prescription opioid overdose? Addiction. 2017; 112(10):1773–1783. DOI: 10.1111/add.13741. PMID: 28009931.
Article11. Fink DS, Schleimer JP, Sarvet A, Grover KK, Delcher C, Castillo-Carniglia A, et al. Association between prescription drug monitoring programs and nonfatal and fatal drug overdoses: a systematic review. Ann Intern Med. 2018; 168(11):783–790. DOI: 10.7326/M17-3074. PMID: 29801093. PMCID: PMC6015770.
Article12. Häuser W, Schug S, Furlan AD. The opioid epidemic and national guidelines for opioid therapy for chronic noncancer pain: a perspective from different continents. PAIN Rep. 2017; 2(3):599. DOI: 10.1097/PR9.0000000000000599. PMID: 29392214. PMCID: PMC5741305.13. Kaye AD, Jones MR, Kaye AM, Ripoll JG, Galan V, Beakley BD, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse: part 1. Pain Physician. 2017; 20(2S):S93–S109. DOI: 10.36076/ppj.2017.s109.14. White AG, Birnbaum HG, Schiller M, Tang J, Katz NP. Analytic models to identify patients at risk for prescription opioid abuse. Am J Manag Care. 2009; 15(12):897–906.15. Centers for Disease Control and Prevention. Data resources: data files of select controlled substances including opioids with oral morphine milligram equivalent (MME) conversion factors, 2018 version [Internet]. Atlanta (GA): Centers for Disease Control and Prevention;c2018. [cited 2024 Aug 23]. Available from. https://www.hhs.gov/guidance/document/opioid-oral-morphine-milligram-equivalent-mme-conversion-factors-0.16. Reddy A, Vidal M, Stephen S, Baumgartner K, Dost S, Nguyen A, et al. The conversion ratio from intravenous hydromorphone to oral opioids in cancer patients. J Pain Symptom Manag. 2017; 54(3):280–288. DOI: 10.1016/j.jpainsymman.2017.07.001. PMID: 28711751.
Article17. Winstanley EL, Zhang Y, Mashni R, Schnee S, Penm J, Boone J, et al. Mandatory review of a prescription drug monitoring program and impact on opioid and benzodiazepine dispensing. Drug Alcohol Depend. 2018; 188:169–174. DOI: 10.1016/j.drugalcdep.2018.03.036. PMID: 29778769. PMCID: PMC6528173.
Article18. Hwang CS, Kang EM, Kornegay CJ, Staffa JA, Jones CM, McAninch JK. Trends in the concomitant prescribing of opioids and benzodiazepines, 2002–2014. Am J Prev Med. 2016; 51(2):151–160. DOI: 10.1016/j.amepre.2016.02.014. PMID: 27079639.
Article19. Yang Z, Wilsey B, Bohm M, Weyrich M, Roy K, Ritley D, et al. Defining risk of prescription opioid overdose: pharmacy shopping and overlapping prescriptions among long-term opioid users in medicaid. J Pain. 2015; 16(5):445–453. DOI: 10.1016/j.jpain.2015.01.475. PMID: 25681095.
Article20. Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the opioid risk tool. Pain Med. 2005; 6(6):432–442. DOI: 10.1111/j.1526-4637.2005.00072.x. PMID: 16336480.
Article21. Wen H, Schackman BR, Aden B, Bao Y. States with prescription drug monitoring mandates saw a reduction in opioids prescribed to Medicaid enrollees. Health Aff. 2017; 36(4):733–741. DOI: 10.1377/hlthaff.2016.1141. PMID: 28373340. PMCID: PMC5625882.
Article22. Helmerhorst GTT, Teunis T, Janssen SJ, Ring D. An epidemic of the use, misuse and overdose of opioids and deaths due to overdose, in the United States and Canada: is Europe next? Bone Joint J. 2017; 99(7):856–864. DOI: 10.1302/0301-620X.99B7.BJJ-2016-1350.R1. PMID: 28663389.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Increasing Very Low-Dose Edoxaban Prescription: Effectiveness and Safety Data of Korean AF Patients
- Analysis of Prescription Trends for Narcotic Appetite Suppressants: Utilizing the Narcotics Information Management System
- Prescription Patterns of Olanzapine among Manic Inpatients with Bipolar Disorder
- Postoperative Pain Control in Laminectomized Patients with Epidural Morphine
- Respiratory Effects of Reversal of Morphine Induced Respiratory Depression by Doxapram