Ewha Med J.
2024 Oct;47(4):e68. 10.12771/emj.2024.e68.
Exploration of the interaction between remote ischemic preconditioning and anesthetic-induced preconditioning using sevoflurane in isolated perfused rabbit heart
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2561413
- DOI: http://doi.org/10.12771/emj.2024.e68
Abstract
Objectives
Remote ischemic preconditioning (rIPC) is a novel technique in which brief episodes of ischemia and reperfusion in one organ confer protection against prolonged ischemia in a distant organ. In contrast, anesthetic-induced preconditioning (APC) utilizes volatile anesthetics to protect multiple organs from ischemia-reperfusion injury. Both methods are easily integrated into various clinical scenarios for cardioprotection. However, it remains unclear whether simultaneous application of these techniques could result in complementary, additive, synergistic, or adverse effects.
Methods
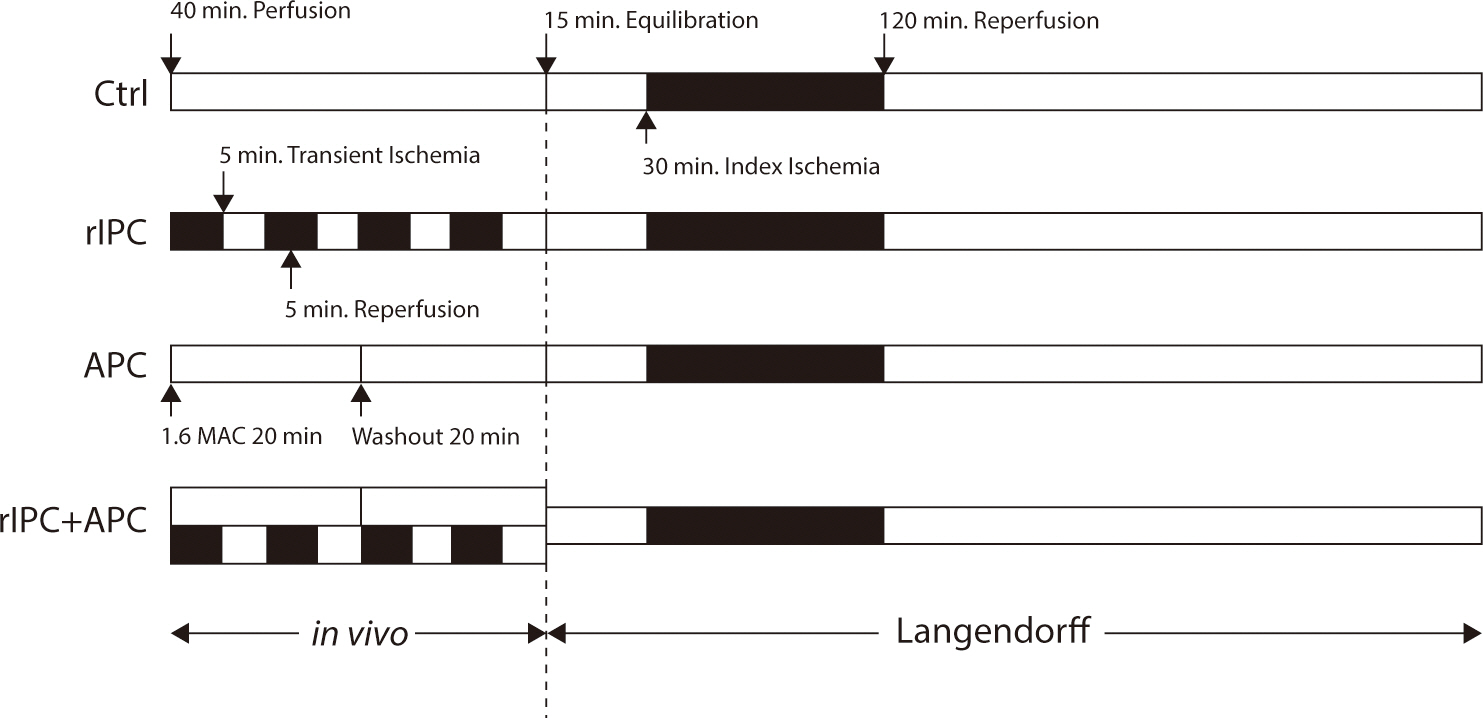
An adult rabbit heart Langendorff model of global ischemia/reperfusion injury was used to compare the cardioprotective effect of rIPC and APC alone and in combination relative to untreated (control) hearts. The rIPC group underwent four cycles of 5-minute ischemia on the hind limb, each followed by 5 minutes of reperfusion. The APC group received 2.5 vol% sevoflurane for 20 minutes via a face mask, followed by a 20-minute washout period.
Results
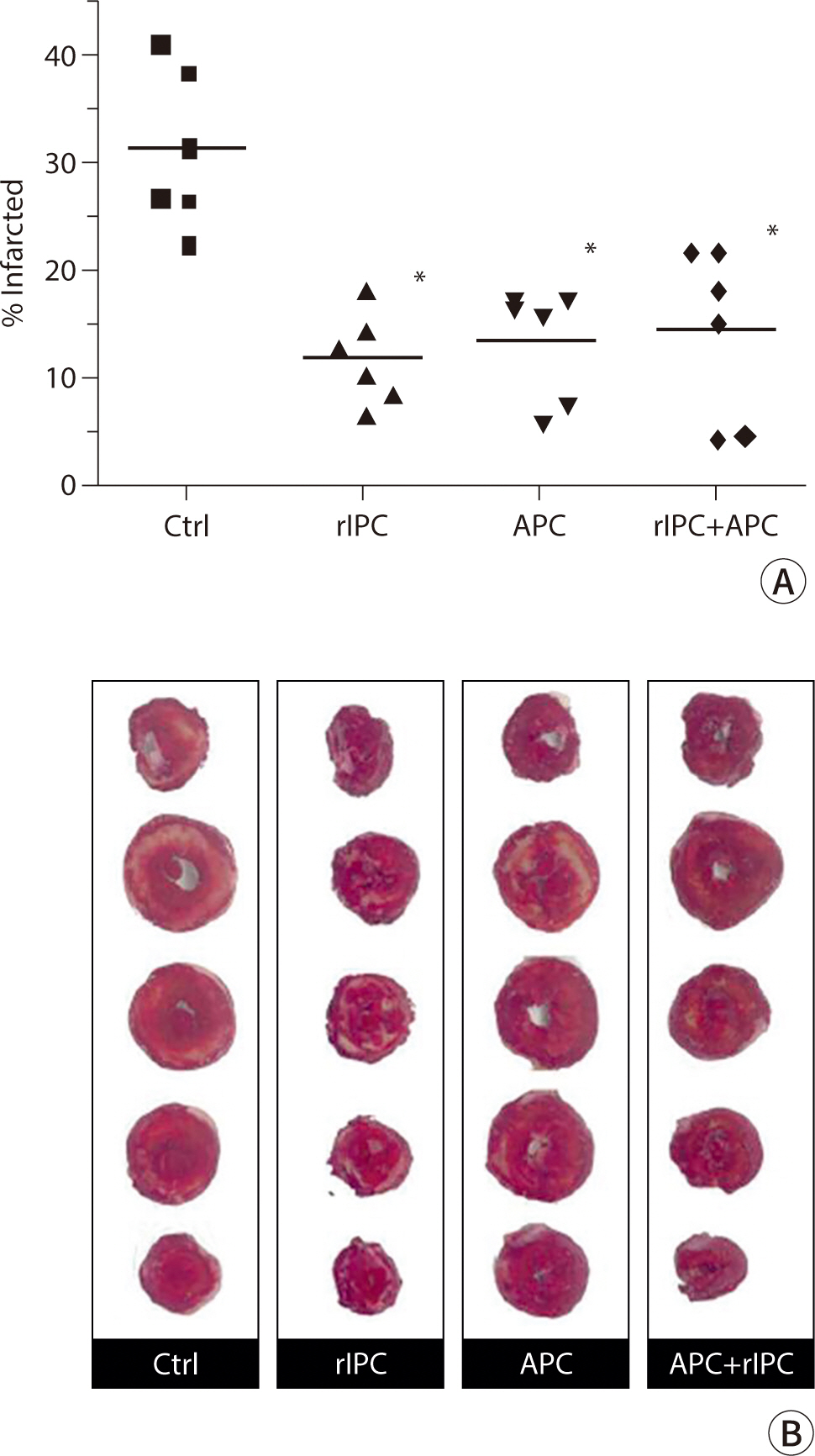
Both in vivo rIPC, induced by four 5-minute cycles of ischemia/reperfusion on the hind limb, and APC, administered as 2.5 vol% sevoflurane via a mask, significantly reduced the size of myocardial infarction following 30 minutes of global ischemia by >50% compared to the untreated control group (rIPC, 12.1±1.7%; APC, 13.5±2.1%; P<0.01 compared to control, 31.3±3.0%). However, no additional protective effect was observed when rIPC and APC were combined (rIPC+APC, 14.4±3.3%).
Conclusion
Although combining rIPC and APC did not provide additional protection, there was no inhibitory effect of one intervention on the other.
Keyword
Figure
Reference
-
References
1. Murry CE, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 1986; 74(5):1124–1136. DOI: 10.1161/01.CIR.74.5.1124. PMID: 3769170.
Article2. Liu Y, Downey JM. Ischemic preconditioning protects against infarction in rat heart. Am J Physiol. 1992; 263(4):H1107–H1112. DOI: 10.1152/ajpheart.1992.263.4.H1107. PMID: 1415759.
Article3. Przyklenk K, Bauer B, Ovize M, Kloner RA, Whittaker P. Regional ischemic 'preconditioning' protects remote virgin myocardium from subsequent sustained coronary occlusion. Circulation. 1993; 87(3):893–899. DOI: 10.1161/01.CIR.87.3.893. PMID: 7680290.
Article4. Konstantinov IE, Li J, Cheung MM, Shimizu M, Stokoe J, Kharbanda RK, et al. Remote ischemic preconditioning of the recipient reduces myocardial ischemia-reperfusion injury of the denervated donor heart via a KATP channel-dependent mechanism. Transplantation. 2005; 79(12):1691–1695. DOI: 10.1097/01.TP.0000159137.76400.5D. PMID: 15973170.
Article5. Cheung MMH, Kharbanda RK, Konstantinov IE, Shimizu M, Frndova Meng H, Li J, et al. Randomized controlled trial of the effects of remote ischemic preconditioning on children undergoing cardiac surgery: first clinical application in humans. J Am Coll Cardiol. 2006; 47(11):2277–2282. DOI: 10.1016/j.jacc.2006.01.066. PMID: 16750696.
Article6. Chiari PC, Bienengraeber MW, Pagel PS, Krolikowski JG, Kersten JR, Warltier DC. Isoflurane protects against myocardial infarction during early reperfusion by activation of phosphatidylinositol-3-kinase signal transduction: evidence for anesthetic-induced postconditioning in rabbits. Anesthesiology. 2005; 102(1):102–109. DOI: 10.1097/00000542-200501000-00018. PMID: 15618793.
Article7. Hausenloy DJ, Yellon DM. Remote ischaemic preconditioning: underlying mechanisms and clinical application. Cardiovasc Res. 2008; 79(3):377–386. DOI: 10.1093/cvr/cvn114. PMID: 18456674.
Article8. Pratt PF Jr, Wang C, Weihrauch D, Bienengraeber MW, Kersten JR, Pagel PS, et al. Cardioprotection by volatile anesthetics: new applications for old drugs? Curr Opin Anesthesiol. 2006; 19(4):397–403. DOI: 10.1097/01.aco.0000236139.31099.b5. PMID: 16829721.
Article9. Piriou V, Chiari P, Lhuillier F, Bastien O, Loufoua J, Raisky O, et al. Pharmacological preconditioning: comparison of desflurane, sevoflurane, isoflurane and halothane in rabbit myocardium. Br J Anaesth. 2002; 89(3):486–491. DOI: 10.1093/bja/89.3.486. PMID: 12402730.
Article10. Garcia C, Julier K, Bestmann L, Zollinger A, von Segesser LK, Pasch T, et al. Preconditioning with sevoflurane decreases PECAM-1 expression and improves one-year cardiovascular outcome in coronary artery bypass graft surgery. Br J Anaesth. 2005; 94(2):159–165. DOI: 10.1093/bja/aei026. PMID: 15556966.
Article11. De Hert SG, Turani F, Mathur S, Stowe DF. Cardioprotection with volatile anesthetics: mechanisms and clinical implications. Anesth Analg. 2005; 100(6):1584–1593. DOI: 10.1213/01.ANE.0000153483.61170.0C. PMID: 15920178.
Article12. Toller WG, Kersten JR, Pagel PS, Hettrick DA, Warltier DC. Sevoflurane reduces myocardial infarct size and decreases the time threshold for ischemic preconditioning in dogs. Anesthesiology. 1999; 91(5):1437–1446. DOI: 10.1097/00000542-199911000-00037. PMID: 10551596.
Article13. Piriou V, Mantz J, Goldfarb G, Kitakaze M, Chiari P, Paquin S, et al. Sevoflurane preconditioning at 1 MAC only provides limited protection in patients undergoing coronary artery bypass surgery: a randomized bi-centre trial. Br J Anaesth. 2007; 99(5):624–631. DOI: 10.1093/bja/aem264. PMID: 17913754.
Article14. De Hert SG, Cromheecke S, ten Broecke PW, Mertens E, De Blier IG, Stockman BA, et al. Effects of propofol, desflurane, and sevoflurane on recovery of myocardial function after coronary surgery in elderly high-risk patients. Anesthesiology. 2003; 99(2):314–323. DOI: 10.1097/00000542-200308000-00013. PMID: 12883404.
Article15. De Hert SG, ten Broecke PW, Mertens E, Van Sommeren EW, De Blier IG, Stockman BA, et al. Sevoflurane but not propofol preserves myocardial function in coronary surgery patients. Anesthesiology. 2002; 97(1):42–49. DOI: 10.1097/00000542-200207000-00007. PMID: 12131102.
Article16. Ali ZA, Callaghan CJ, Lim E, Ali AA, Reza Nouraei SA, Akthar AM, et al. Remote ischemic preconditioning reduces myocardial and renal injury after elective abdominal aortic aneurysm repair: a randomized controlled trial. Circulation. 2007; 116:11 Suppl. I98–I105. DOI: 10.1161/circulationaha.106.679167. PMID: 17846333.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Hypoxic-Preconditioning on the Reperfusion-Induced Arrhythmias in the Cat Hearts
- Neurogenic pathways in remote ischemic preconditioning induced cardioprotection: Evidences and possible mechanisms
- Mechanisms and Prospects of Ischemic Tolerance Induced by Cerebral Preconditioning
- Effects of Ischemic preconditioning on the Post-ischemic Myocardial Dysfunction and Coronary Flow in the Isolated Rat Hearts
- Effect of Ischemic Preconditioning on Catecholamine Release from the Isolated, Ischemic Reperfused Hearts of Rats