J Korean Assoc Oral Maxillofac Surg.
2024 Oct;50(5):292-296. 10.5125/jkaoms.2024.50.5.292.
Peripheral ossifying fibroma arising from the maxillary bucco-palatal gingiva in an elderly male patient: a rare case report
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Dankook University, Cheonan, Korea
- KMID: 2560825
- DOI: http://doi.org/10.5125/jkaoms.2024.50.5.292
Abstract
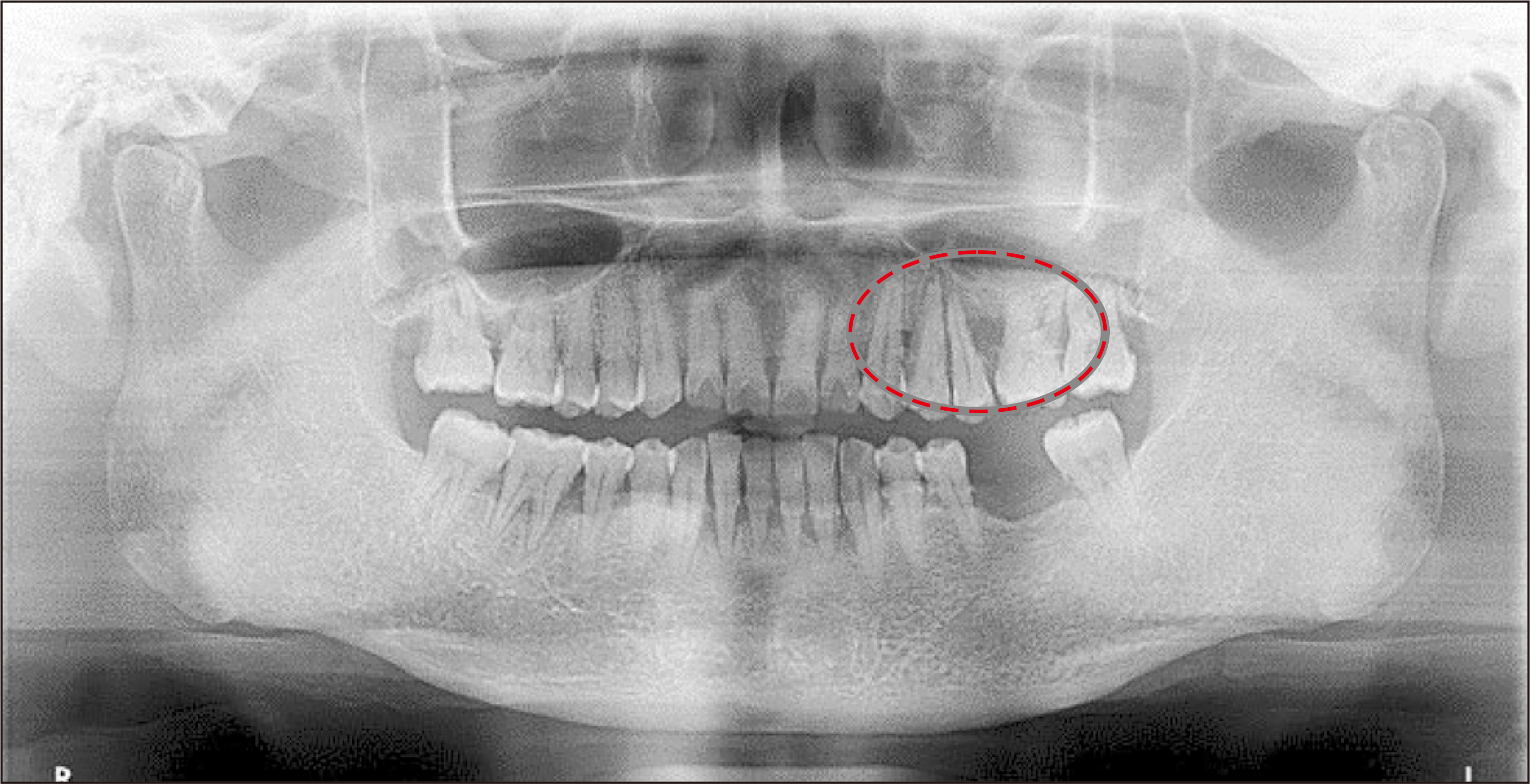
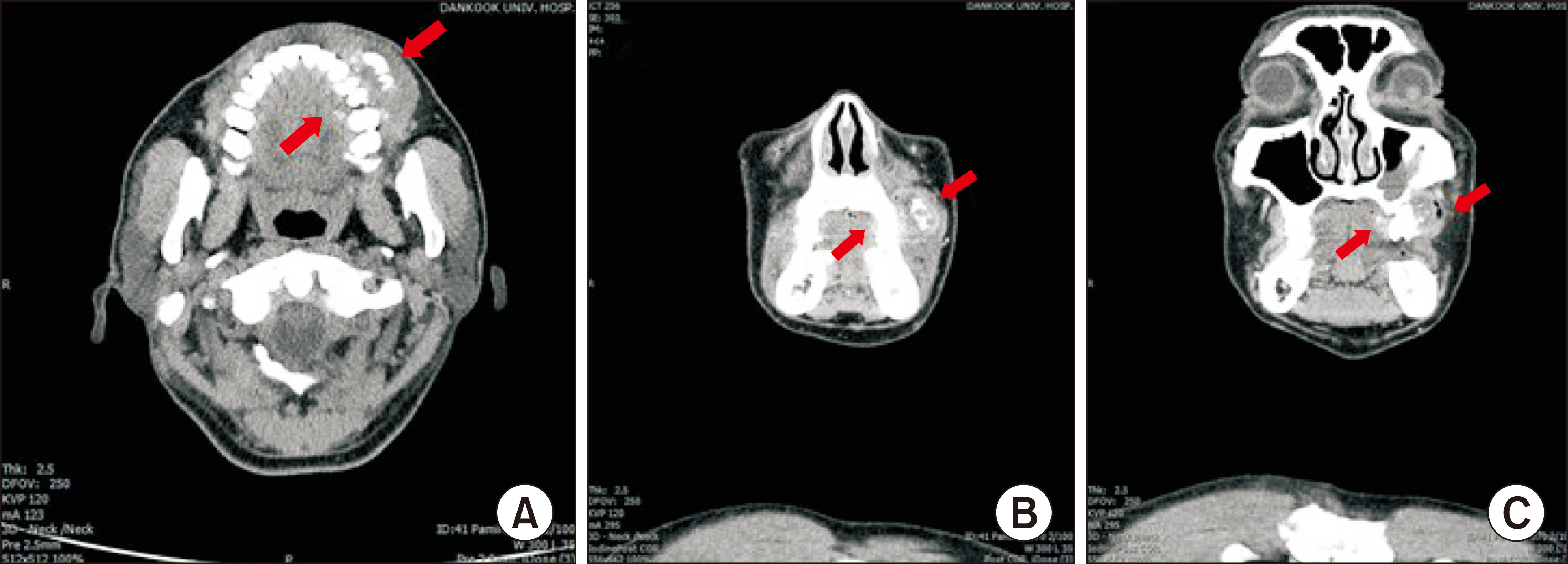
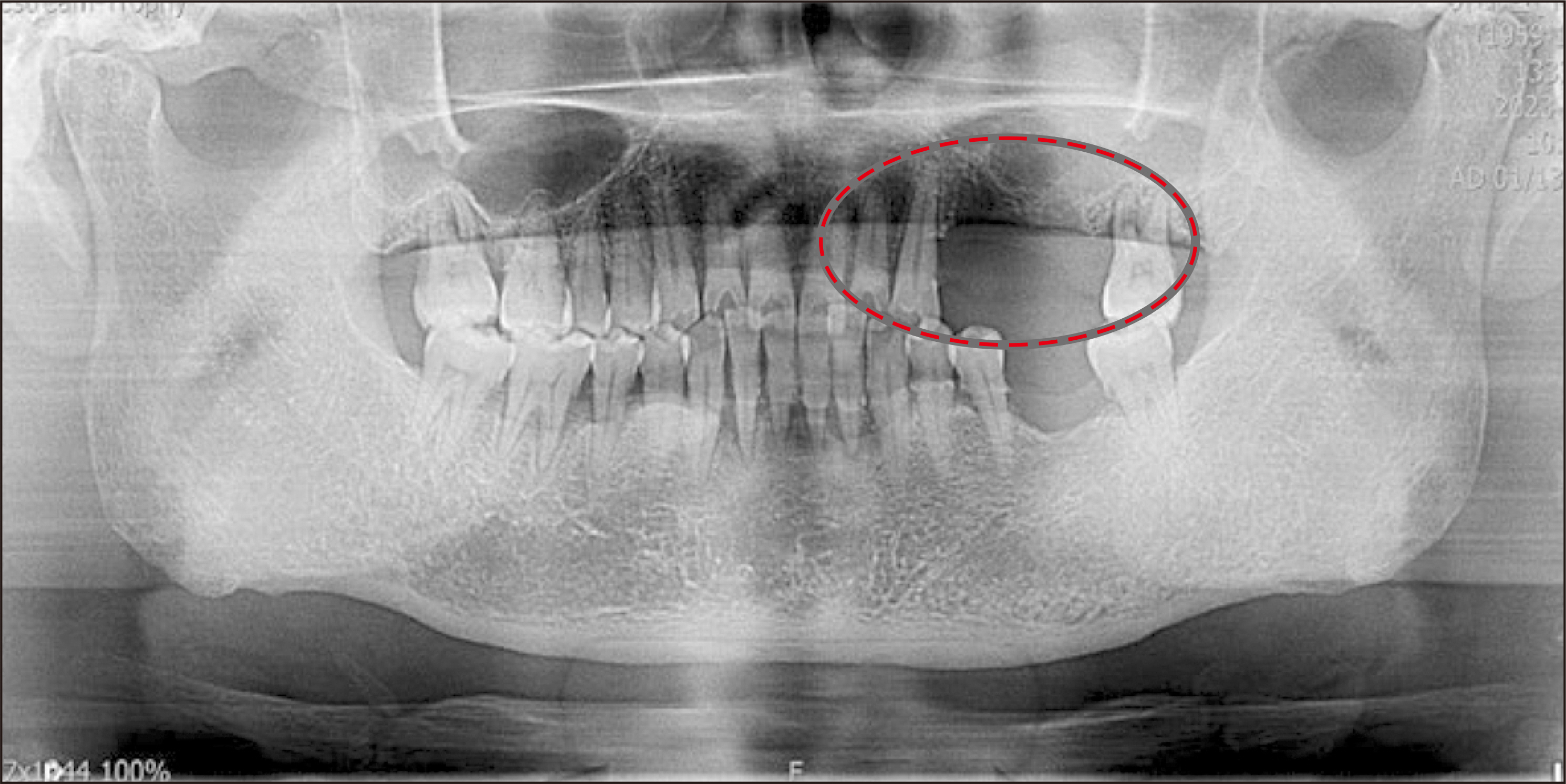
- Peripheral ossifying fibroma (POF) is a benign tumor characterized by dystrophic calcification or ossification within the gingiva, primarily affecting the anterior maxilla of females and young adults. Its pathogenesis is unclear but linked to local irritants such as trauma, biofilm, dental calculus, and poorly fitting prostheses. In this study, a 63-year-old male presented at Dankook University Dental Hospital with a large nodular lesion on the left maxillary bucco-palatal gingiva. Preoperative imaging, including panoramic radiography and cone-beam computed tomography, was performed. Surgical excision and histological examination confirmed POF with specific morphological characteristics, including mineralized tissue with varied deposition patterns, mature and immature bone, cementum-like tissue, and dystrophic calcification. In conclusion, POF is a rare oral tumor, more common in younger females, typically presenting asymptomatically on the anterior maxilla. Histopathological analysis is crucial for diagnosis. Standard treatment involves conservative local resection, but recurrence rates range from 8% to 20%, necessitating continuous follow-up. This report aims to enhance understanding of POF by presenting a rare case of a large POF in the maxillary posterior bucco-palatal gingiva of an elderly male.
Keyword
Figure
Reference
-
References
1. Waldron CA. 1993; Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg. 51:828–35. https://doi.org/10.1016/s0278-2391(10)80097-7. DOI: 10.1016/S0278-2391(10)80097-7. PMID: 8336219.
Article2. Shepherd SM. 1843; Alveolar exostosis. Am J Dent Sci. 4:53–4.3. Eversole LR, Rovin S. 1972; Reactive lesions of the gingiva. J Oral Pathol. 1:30–8. DOI: 10.1111/j.1600-0714.1972.tb02137.x.
Article4. Shrestha A, Keshwar S, Jain N, Raut T, Jaisani MR, Sharma SL. 2021; Clinico-pathological profiling of peripheral ossifying fibroma of the oral cavity. Clin Case Rep. 9:e04966. https://doi.org/10.1002/ccr3.4966. DOI: 10.1002/ccr3.4966. PMID: 34691463. PMCID: PMC8513507.
Article5. Cavalcante IL, Barros CC, Cruz VM, Cunha JL, Leão LC, Ribeiro RR, et al. 2022; Peripheral ossifying fibroma: a 20-year retrospective study with focus on clinical and morphological features. Med Oral Patol Oral Cir Bucal. 27:e460–7. https://doi.org/10.4317/medoral.25454. DOI: 10.4317/medoral.25454. PMID: 35717619. PMCID: PMC9445604.
Article6. Lázare H, Peteiro A, Pérez Sayáns M, Gándara-Vila P, Caneiro J, García-García A, et al. 2019; Clinicopathological features of peripheral ossifying fibroma in a series of 41 patients. Br J Oral Maxillofac Surg. 57:1081–5. https://doi.org/10.1016/j.bjoms.2019.09.020. DOI: 10.1016/j.bjoms.2019.09.020. PMID: 31601435.
Article7. Tsiligkrou IA, Tosios KI, Madianos PN, Vrotsos IA, Panis VG. 2015; Oxytalan-positive peripheral ossifying fibromas express runt-related transcription factor 2, bone morphogenetic protein-2, and cementum attachment protein. An immunohistochemical study. J Oral Pathol Med. 44:628–33. https://doi.org/10.1111/jop.12275. DOI: 10.1111/jop.12275. PMID: 25359431.
Article8. Walters JD, Will JK, Hatfield RD, Cacchillo DA, Raabe DA. 2001; Excision and repair of the peripheral ossifying fibroma: a report of 3 cases. J Periodontol. 72:939–44. https://doi.org/10.1902/jop.2001.72.7.939. DOI: 10.1902/jop.2001.72.7.939. PMID: 11495143.
Article9. El Achkar VNR, Medeiros RDS, Longue FG, Anbinder AL, Kaminagakura E. 2017; The role of osterix protein in the pathogenesis of peripheral ossifying fibroma. Braz Oral Res. 31:e53. https://doi.org/10.1590/1807-3107bor-2017.vol31.0053. DOI: 10.1590/1807-3107bor-2017.vol31.0053. PMID: 28678972.
Article10. Koury ME, Regezi JA, Perrott DH, Kaban LB. 1995; "Atypical" fibro-osseous lesions: diagnostic challenges and treatment concepts. Int J Oral Maxillofac Surg. 24:162–9. https://doi.org/10.1016/s0901-5027(06)80094-9. DOI: 10.1016/S0901-5027(06)80094-9. PMID: 7608584.
Article11. Voytek TM, Ro JY, Edeiken J, Ayala AG. 1995; Fibrous dysplasia and cemento-ossifying fibroma. A histologic spectrum. Am J Surg Pathol. 19:775–81. DOI: 10.1097/00000478-199507000-00005. PMID: 7793475.12. Slootweg PJ. 1996; Maxillofacial fibro-osseous lesions: classification and differential diagnosis. Semin Diagn Pathol. 13:104–12.13. Verma E, Chakki AB, Nagaral SC, Ganji KK. 2013; Peripheral cemento-ossifying fibroma: case series literature review. Case Rep Dent. 2013:930870. https://doi.org/10.1155/2013/930870. DOI: 10.1155/2013/930870. PMID: 23365762. PMCID: PMC3556846.
Article14. Buchner A, Shnaiderman-Shapiro A, Vered M. 2010; Relative frequency of localized reactive hyperplastic lesions of the gingiva: a retrospective study of 1675 cases from Israel. J Oral Pathol Med. 39:631–8. https://doi.org/10.1111/j.1600-0714.2010.00895.x. DOI: 10.1111/j.1600-0714.2010.00895.x. PMID: 20456619.
Article15. Barot VJ, Chandran S, Vishnoi SL. 2013; Peripheral ossifying fibroma: a case report. J Indian Soc Periodontol. 17:819–22. https://doi.org/10.4103/0972-124x.124533. DOI: 10.4103/0972-124X.124533. PMID: 24554899. PMCID: PMC3917219.
Article16. Mishra AK, Maru R, Dhodapkar SV, Jaiswal G, Kumar R, Punjabi H. 2013; Peripheral cemento-ossifying fibroma: a case report with review of literature. World J Clin Cases. 1:128–33. https://doi.org/10.12998/wjcc.v1.i3.128. DOI: 10.12998/wjcc.v1.i3.128. PMID: 24303483. PMCID: PMC3845913.
Article17. Mergoni G, Meleti M, Magnolo S, Giovannacci I, Corcione L, Vescovi P. 2015; Peripheral ossifying fibroma: a clinicopathologic study of 27 cases and review of the literature with emphasis on histomorphologic features. J Indian Soc Periodontol. 19:83–7. https://doi.org/10.4103/0972-124x.145813. DOI: 10.4103/0972-124X.145813. PMID: 25810599. PMCID: PMC4365164.
Article18. Salaria SK, Gupta N, Bhatia V, Nayar A. 2015; Management of residual mucogingival defect resulting from the excision of recurrent peripheral ossifying fibroma by periodontal plastic surgical procedure. Contemp Clin Dent. 6(Suppl 1):S274–7. https://doi.org/10.4103/0976-237x.166832. DOI: 10.4103/0976-237X.166832. PMID: 26604587. PMCID: PMC4632236.
Article19. Cuisia ZE, Brannon RB. 2001; Peripheral ossifying fibroma--a clinical evaluation of 134 pediatric cases. Pediatr Dent. 23:245–8.