J Korean Med Sci.
2024 Oct;39(40):e261. 10.3346/jkms.2024.39.e261.
Barriers and Facilitators of Pediatric Obesity Prevention and Management (POPM) Programs in Korea: Focusing on the Questionnaire About the Linkage in Community Level
- Affiliations
-
- 1Department of Health Sciences, Graduate School, Korea University, Seoul, Korea
- 2Department of Public Health Policy, Gyeonggi Public Health Policy Institute, Seongnam, Korea
- 3Department of Pediatrics, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 4Department of Pediatrics, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 5Department of Pediatrics, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2560662
- DOI: http://doi.org/10.3346/jkms.2024.39.e261
Abstract
- Background
Recent global trends indicate a rise in pediatric obesity, reflecting patterns also observed in South Korea. Given its significant impact on chronic disease prevalence in adulthood, pediatric obesity poses potential societal challenges. For pediatric obesityrelated prevention or management programs in community level to operate effectively, there needs to be a clear understanding of barriers and facilitators of the programs. This study aims to establish a foundation for policy implementation, contributing to pediatric obesity prevention and management (POPM) in Korea.
Methods
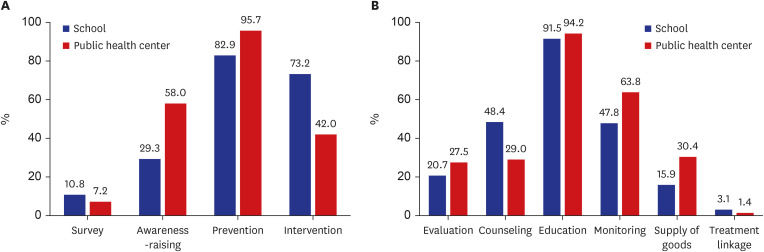
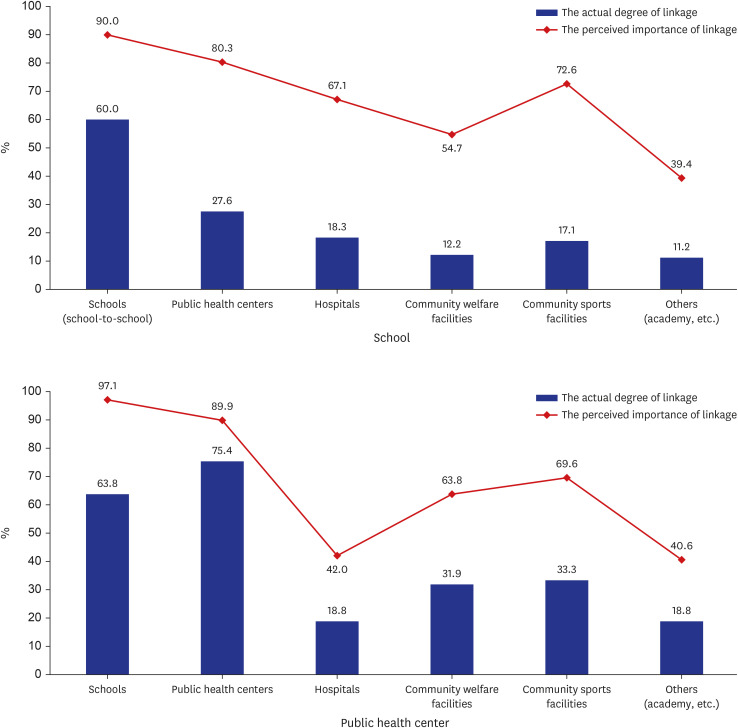
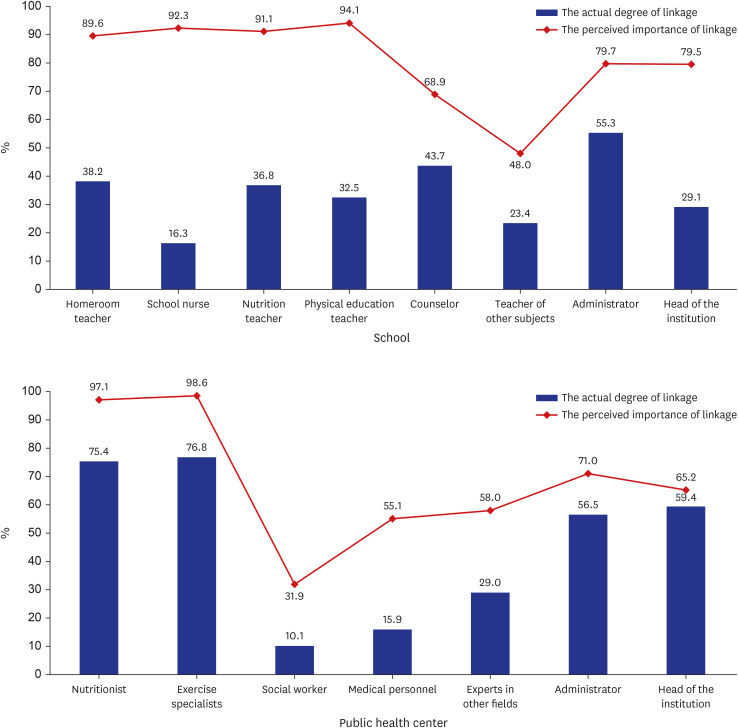
A survey was conducted among program providers involved in domestic POPM programs. A total of 577 individuals completed the survey, including those working in elementary and middle schools (n = 508) and public health centers (n = 69) nationwide. The questionnaire comprised 67 questions covering characteristics of respondents, purpose and contents of POPM programs, measurement of program outcome, level of inter- and intrainstitutional linkage, difficulties in operating programs and factors that facilitate programs. A 5-point Likert scale was used for most questions. Descriptive statistics was employed to analyze characteristics of respondents in POPM programs. The level of linkage in POPM programs was assessed using perceived importance and actual degree of linkage. The difficulties in operating POPM programs were analyzed based on agreement responses, and facilitating factors of program activation were analyzed based on importance responses.
Results
The domestic POPM program showed low actual linkage compared to its perceived importance, both between institutions and among professions within institutions. Difficulties in operating the program included securing availability of students, encouraging participation of reluctant students and development of new programs. The survey suggested that schools require support from parents, guardians and family members, while public health centers need professional providers to facilitate such programs.
Conclusion
The study highlights the urgent need for strategies to address pediatric obesity in South Korea. Weak institutional linkages hinder effective programs. Challenges include student availability, participation, and the need for innovative programs. New approaches to build partnerships in harmony among institutions are necessary. Implementing findings into policy can help prevent obesity in Korean children and adolescents.
Keyword
Figure
Reference
-
1. Bomberg EM, Kyle T, Stanford FC. Considering pediatric obesity as a US public health emergency. Pediatrics. 2023; 152(4):e2023061501. PMID: 37701953.2. Lobstein T, Jackson-Leach R, Powis J, Brinsden H, Gray M. World Obesity Atlas 2023. London, UK: World Obesity Federation;2023.3. Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med. 2017; 377(22):2145–2153. PMID: 29171811.4. Kumar V, Rout C, Singh J, Saharan Y, Goyat R, Umar A, et al. A review on the clean-up technologies for heavy metal ions contaminated soil samples. Heliyon (Lond). 2023; 9(5):e15472.5. Kim JH, Moon JS. Secular trends in pediatric overweight and obesity in Korea. J Obes Metab Syndr. 2020; 29(1):12–17. PMID: 32188238.6. Sherwood NE, French SA, Veblen-Mortenson S, Crain AL, Berge J, Kunin-Batson A, et al. NET-Works: Linking families, communities and primary care to prevent obesity in preschool-age children. Contemp Clin Trials. 2013; 36(2):544–554. PMID: 24120933.7. Dietz WH, Solomon LS, Pronk N, Ziegenhorn SK, Standish M, Longjohn MM, et al. An integrated framework for the prevention and treatment of obesity and its related chronic diseases. Health Aff (Millwood). 2015; 34(9):1456–1463. PMID: 26355046.8. Hampl SE, Hassink SG, Skinner AC, Armstrong SC, Barlow SE, Bolling CF, et al. Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics. 2023; 151(2):e2022060640. PMID: 36622115.9. Richard L, Gauvin L, Raine K. Ecological models revisited: their uses and evolution in health promotion over two decades. Annu Rev Public Health. 2011; 32(1):307–326. PMID: 21219155.10. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988; 15(4):351–377. PMID: 3068205.11. Ward ZJ, Bleich SN, Long MW, Gortmaker SL. Association of body mass index with health care expenditures in the United States by age and sex. PLoS One. 2021; 16(3):e0247307. PMID: 33760880.12. Heerman WJ, Kenney E, Block JP, Fiechtner L, McMahon E, Kruse L, et al. A narrative review of public health interventions for childhood obesity. Curr Obes Rep. 2024; 13(1):87–97. PMID: 38172483.13. Po’e EK, Gesell SB, Lynne Caples T, Escarfuller J, Barkin SL. Pediatric obesity community programs: barriers & facilitators toward sustainability. J Community Health. 2010; 35(4):348–354. PMID: 20352479.14. Sturmberg JP, Martin CM. Complexity and health--yesterday’s traditions, tomorrow’s future. J Eval Clin Pract. 2009; 15(3):543–548. PMID: 19522908.15. Korea Youth Work Agency. Number of academies attended on weekdays (Monday to Friday). 2011 Survey on Demand and Status of After-School Activities for Youth. Seoul, Korea: Korea Youth Work Agency;2022.16. Warnick JL, Darling KE, West CE, Jones L, Jelalian E. Weight stigma and mental health in youth: a systematic review and meta-analysis. J Pediatr Psychol. 2022; 47(3):237–255. PMID: 34791368.17. Block JP, Oken E. Practical considerations for the US Preventive Services Task Force recommendations on obesity in children and adolescents. JAMA Intern Med. 2017; 177(8):1077–1079. PMID: 28632842.18. Barlow SE, Ohlemeyer CL. Parent reasons for nonreturn to a pediatric weight management program. Clin Pediatr (Phila). 2006; 45(4):355–360. PMID: 16703159.19. Proaño GV, Rodriguez Moreno LM, Arciniegas MJ, Sifre-Acosta N, Espinal C, Chowdhury R, et al. Effectiveness, barriers, and facilitators of overweight and obesity prevention strategies in Latin America; a scoping review and qualitative study in Colombia. Lancet Reg Health Am. 2024; 29:100656. PMID: 38250673.20. Park S, Choo J. Ecological factors and strategies for childhood obesity prevention targeting vulnerable children: Using community-based participatory research. J Korean Acad Community Health Nurs. 2020; 31(3):256–268.21. Hayes CB, O’Shea MP, Foley-Nolan C, McCarthy M, Harrington JM. Barriers and facilitators to adoption, implementation and sustainment of obesity prevention interventions in schoolchildren- a DEDIPAC case study. BMC Public Health. 2019; 19(1):198. PMID: 30767770.22. Totura CM, Figueroa HL, Wharton C, Marsiglia FF. Assessing implementation of evidence-based childhood obesity prevention strategies in schools. Prev Med Rep. 2015; 2:347–354. PMID: 26844091.23. Owen B, Brown AD, Kuhlberg J, Millar L, Nichols M, Economos C, et al. Understanding a successful obesity prevention initiative in children under 5 from a systems perspective. PLoS One. 2018; 13(3):e0195141. PMID: 29596488.24. Williams DR, Braddock A, Houser M, Blair G, Browne N. Review of upstream social factors contributing to childhood obesity. Obes Pillars. 2022; 4:100040. PMID: 37990668.25. Vandevijvere S, De Pauw R, Djojosoeparto S, Gorasso V, Guariguata L, Løvhaug AL, et al. Upstream determinants of overweight and obesity in Europe. Curr Obes Rep. 2023; 12(4):417–428. PMID: 37594616.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status and Needs Assessment for Obesity Prevention and Management Project at Public Health Centers
- Facilitators and barriers to achieving dietary and physical activity goals : focus group interviews with city bus drivers and counseling dietitians
- A Comparison on the Tobacco Control Intervention, Barriers, and Facilitators between Oncology Nurses and General Nurses in Clinical Practice
- Ecological Factors and Strategies for Childhood Obesity Prevention Targeting Vulnerable Children: Using Community-Based Participatory Research
- Barriers and facilitators in the provision of palliative care in adult intensive care units: a scoping review