J Korean Neurosurg Soc.
2024 Nov;67(6):646-653. 10.3340/jkns.2024.0003.
Preliminary Report of Fully Endoscopic Microvascular Decompression
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Cheonan Hospital, College of Medicine, Soonchunhyang University, Cheonan, Korea
- KMID: 2560406
- DOI: http://doi.org/10.3340/jkns.2024.0003
Abstract
Objective
: Microscopic microvascular decompression (MVD) has been considered to be a useful treatment modality for medically refractory hemifacial spasm (HFS) and trigeminal neuralgia. But, the advent of the endoscopic era has presented new possibilities to MVD surgery. While the microscope remains a valuable tool, the endoscope offers several advantages with comparable clinical outcomes. Thus, fully endoscopic MVD (E-MVD) could be a reasonable alternative to microscopic MVD. This paper explores the safety and efficacy of the fully E-MVD technique.
Methods
: A single-center retrospective study was conducted in 25 patients diagnosed with HFS between September 2019 and July 2023. All surgeries were performed by a single neurosurgeon using the fully E-MVD technique without any assistance of a microscope. The study reviewed intraoperative brainstem auditory evoked potentials and disappearance of the lateral spread response. Outcomes were assessed based on the patients’ clinical status immediately after surgery and at their last follow-up. Complications, including facial palsy, hearing loss, ataxia, dysphagia, palsy of other cranial nerves, and cerebrospinal fluid leakage, were also examined.
Results
: The most common offending artery was the anterior inferior cerebellar artery (AICA) in 15 cases (60.0%), followed by the posterior inferior cerebellar artery in eight cases (32.0%), vertebral artery (VA) in one case (4.0%), tandem lesions involving the AICA and VA in one case (4.0%). Ten patients (40.0%) had pre-operative facial palsy on the ipsilateral side, and eight patients (32.0%) experienced delayed facial palsy on the ipsilateral side, from which they fully recovered by the last follow-up. The median operation time was 105 minutes. All patients were symptom free immediately after surgery and at the last follow-up. One patient experienced a permanent complication, such as high-frequency hearing loss, from which he partially recovered over time.
Conclusion
: Fully E-MVD demonstrated similar clinical outcomes to microscopic MVD. It offered a similar complication rate, shorter operation time, and a panoramic view with a smaller craniectomy size. Although there is a learning curve associated with fully E-MVD, it presents a viable alternative in the endoscopic era.
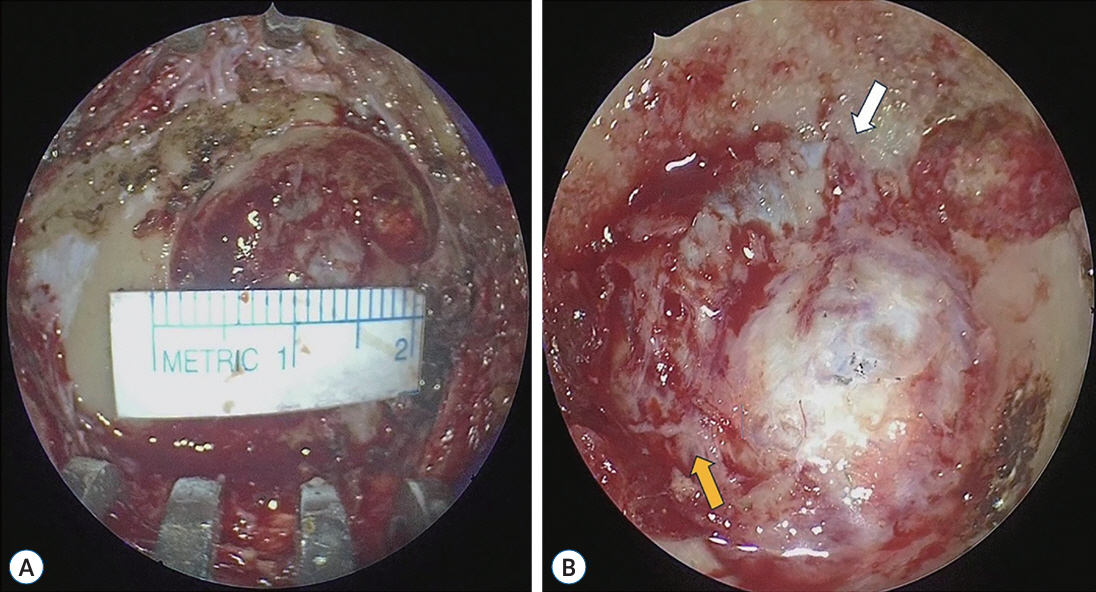
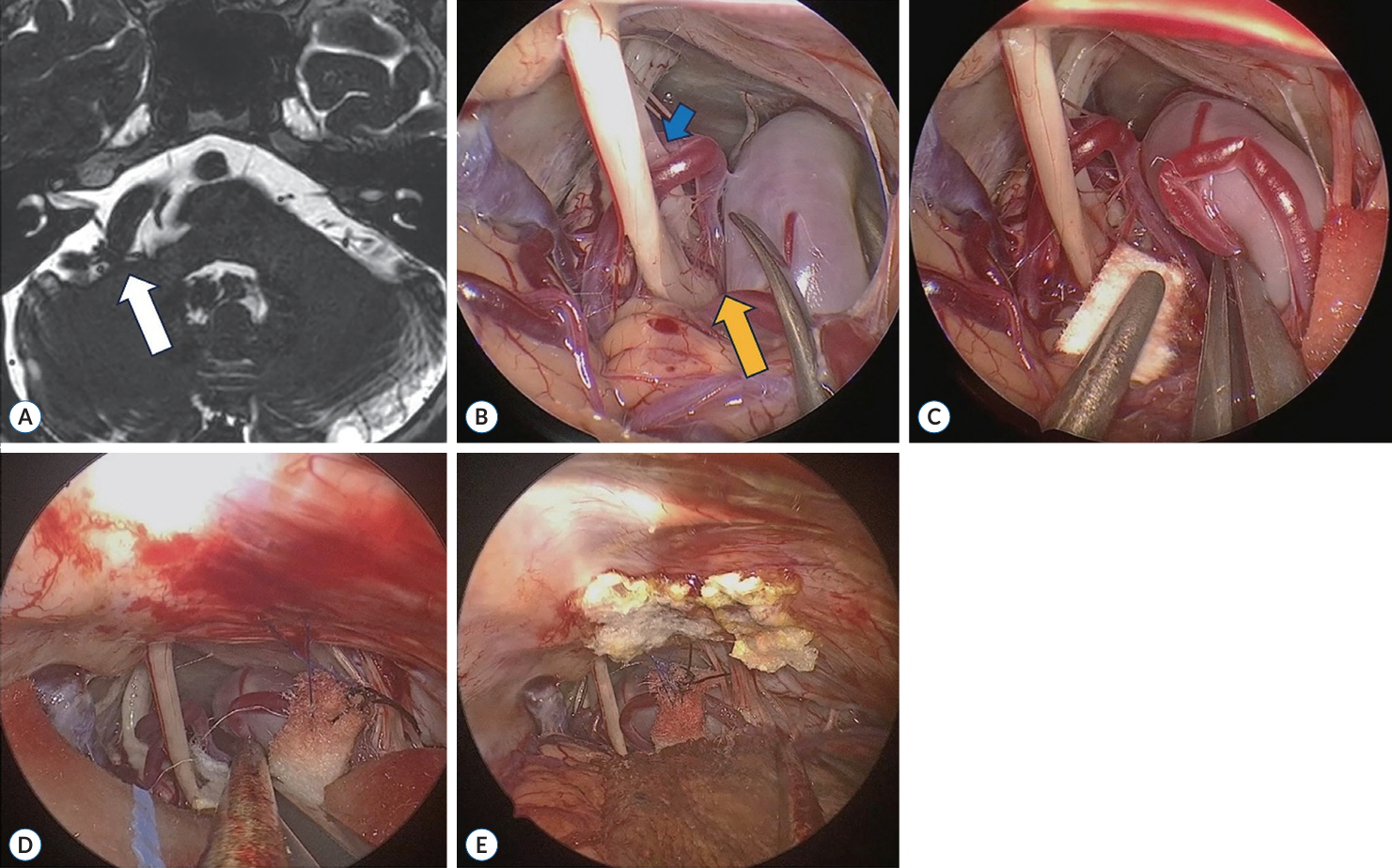
Figure
Reference
-
References
1. Barker FG 2nd, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD. The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med. 334:1077–1084. 1996.
Article2. Barker FG 2nd, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD. Microvascular decompression for hemifacial spasm. J Neurosurg. 82:201–210. 1995.
Article3. Bohman LE, Pierce J, Stephen JH, Sandhu S, Lee JYK. Fully endoscopic microvascular decompression for trigeminal neuralgia: technique review and early outcomes. Neurosurg Focus. 37:E18. 2014.
Article4. Cheng WY, Chao SC, Shen CC. Endoscopic microvascular decompression of the hemifacial spasm. Surg Neurol 70 Suppl. 1:40–46. 2008.
Article5. Flanders TM, Blue R, Roberts S, McShane BJ, Wilent B, Tambi V, et al. Fully endoscopic microvascular decompression for hemifacial spasm. J Neurosurg. 131:813–819. 2018.
Article6. Halpern CH, Lang SS, Lee JYK. Fully endoscopic microvascular decompression: our early experience. Minim Invasive Surg. 2013:739432. 2013.
Article7. Jarrahy R, Eby JB, Cha ST, Shahinian HK. Fully endoscopic vascular decompression of the trigeminal nerve. Minim Invasive Neurosurg. 45:32–35. 2002.
Article8. Lee JYK, Pierce JT, Sandhu SK, Petrov D, Yang AI. Endoscopic versus microscopic microvascular decompression for trigeminal neuralgia: equivalent pain outcomes with possibly decreased postoperative headache after endoscopic surgery. J Neurosurg. 126:1676–1684. 2017.
Article9. Lu AY, Yeung JT, Gerrard JL, Michaelides EM, Sekula RF Jr, Bulsara KR. Hemifacial spasm and neurovascular compression. ScientificWorldJournal. 2014:3493. 2014.
Article10. Nielsen VK. Pathophysiology of hemifacial spasm: I. Ephaptic transmission and ectopic excitation. Neurology. 34:418–426. 1984.11. Pak HL, Lambru G, Okasha M, Maratos E, Thomas N, Shapey J, et al. Fully endoscopic microvascular decompression for trigeminal neuralgia: technical note describing a single-center experience. World Neurosurg. 166:159–167. 2022.
Article12. Park JS, Kong DS, Lee JA, Park K. Hemifacial spasm: neurovascular compressive patterns and surgical significance. Acta Neurochir (Wien). 150:235–241. discussion 241. 2008.
Article13. Phang SY, Martin J, Zilani G. Assessing the safety and learning curve of a neurosurgical trainee in performing a microvascular decompression (MVD). Br J Neurosurg. 33:486–489. 2019.
Article14. Wang A, Jankovic J. Hemifacial spasm: clinical findings and treatment. Muscle Nerve. 21:1740–1747. 1998.
Article15. Zagzoog N, Attar A, Takroni R, Alotaibi MB, Reddy K. Endoscopic versus open microvascular decompression for trigeminal neuralgia: a systematic review and comparative meta-analysis. J Neurosurg. 131:1532–1540. 2018.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Significance of Intraoperative BAEPs Monitoring during Microvascular Decompression Surgery
- Preliminary Results of The Treatment for Failed Back Surgery Syndrome by Full Endoscopic Approach at Saint Paul General Hospital, in Hanoi, Vietnam
- Intraoperative monitoring of microvascular decompression in hemifacial spasm
- Two Portal Percutaneous Endoscopic Decompression for Lumbar Spinal Stenosis: Preliminary Study
- Surgical Treatment of Spasmodic Torticollis by Microvascular Decompression with Selective Dorsal Cervical Phizotomy: Case Report