J Korean Neurosurg Soc.
2024 Nov;67(6):622-636. 10.3340/jkns.2023.0205.
High-Volume Hospital Had Lower Mortality of Severe Intracerebral Hemorrhage Patients
- Affiliations
-
- 1Department of Neurosurgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Molecular Biophysics and Biochemistry, Yale University, New Haven, CT, USA
- 3Department of Neurosurgery, Cheonan Hospital, College of Medicine, Soonchunhyang University, Cheonan, Korea
- 4Health Insurance Review & Assessment Service (HIRA), Wonju, Korea
- KMID: 2560404
- DOI: http://doi.org/10.3340/jkns.2023.0205
Abstract
Objective
: Intracerebral hemorrhage (ICH) accompanies higher mortality rates than other type of stroke. This study aimed to investigate the association between hospital volume and mortality for cases of ICH.
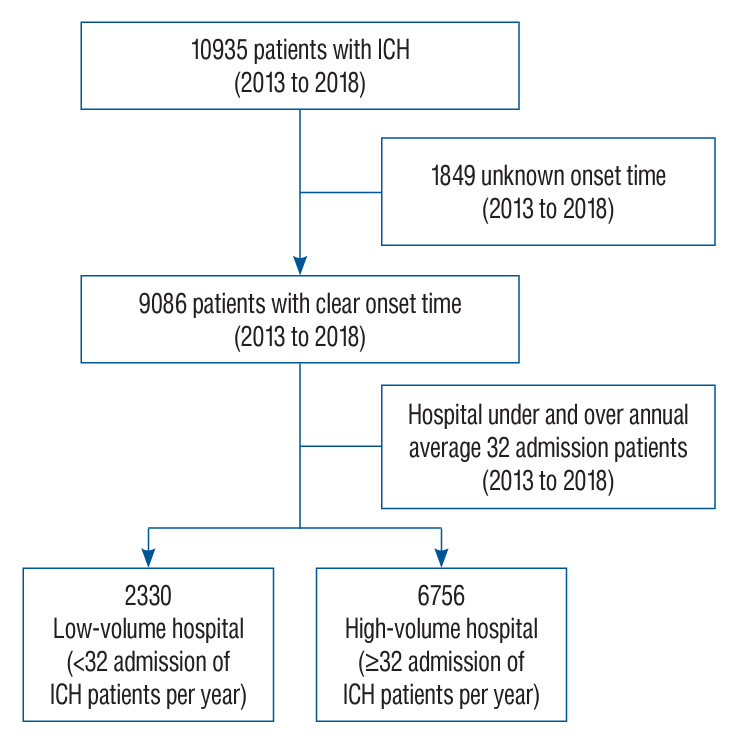
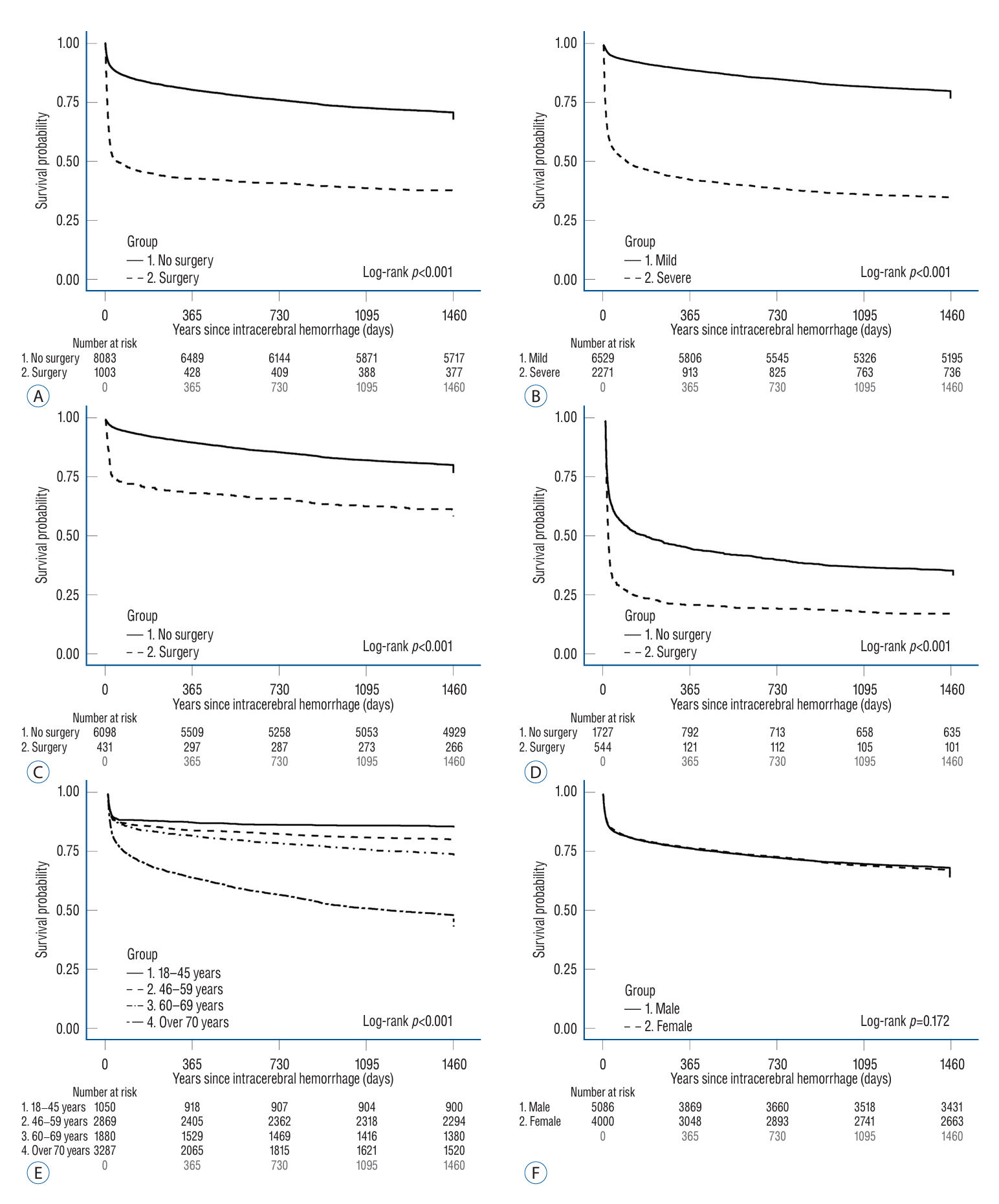
Methods
: We used nationwide data from 2013 to 2018 to compare high-volume hospitals (≥32 admissions/year) and low-volume hospitals (<32 admissions/year). We tracked patients’ survival at 3-month, 1-year, 2-year, and 4-year endpoints. The survival of ICH patients was analyzed at 3-month, 1-year, 2-year, and 4-year endpoints using Kaplan-Meier survival analysis. Multivariable logistic regression analysis and Cox regression analysis were performed to determine predictive factors of poor outcomes at discharge and death.
Results
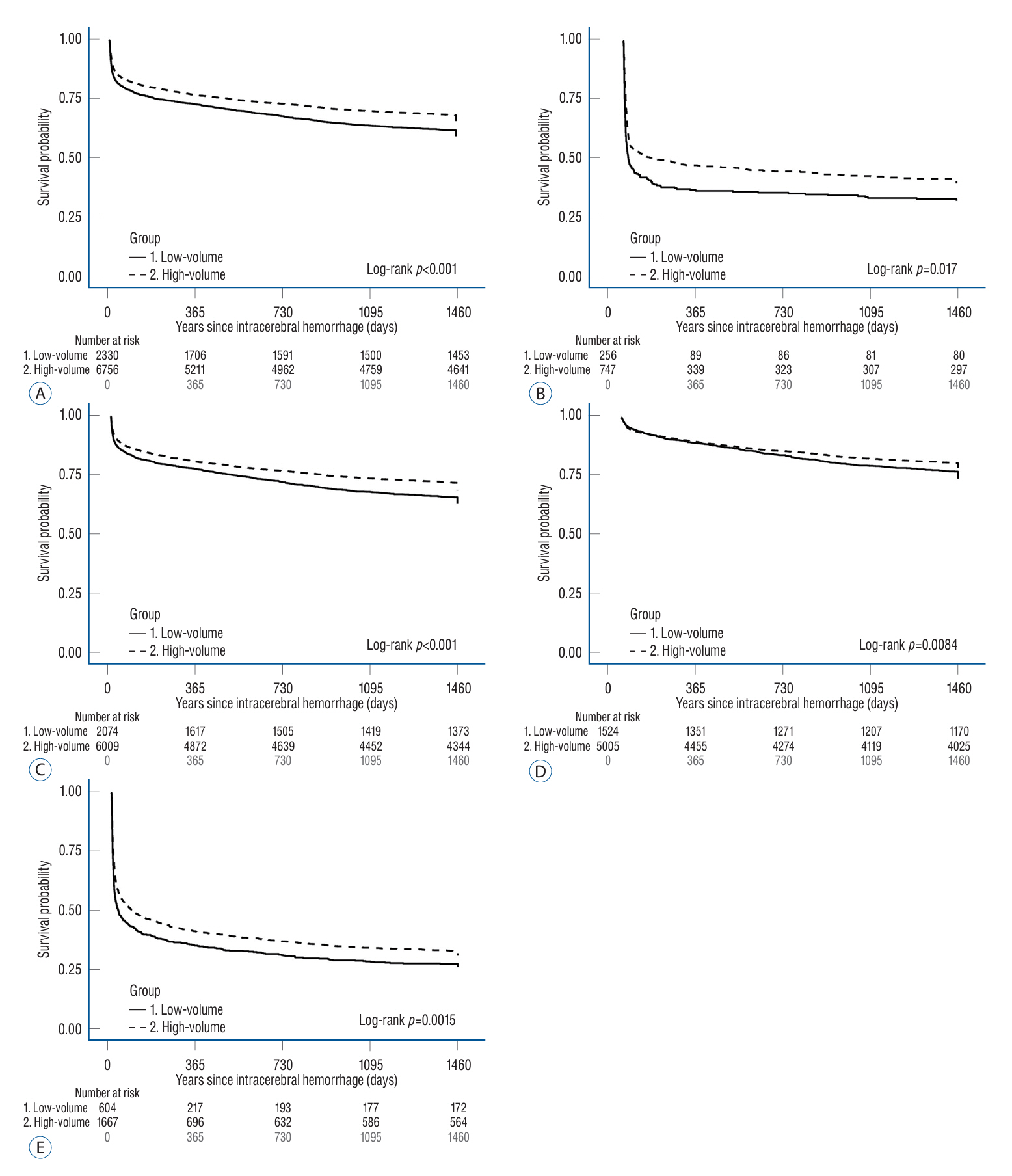
: Among 9086 ICH patients who admitted to hospital during 18-month period, 6756 (74.4%) and 2330 (25.6%) patients were admitted to high-volume and low-volume hospitals. The mortality of total ICH patients was 18.25%, 23.87%, 27.88%, and 35.74% at the 3-month, 1-year, 2-year, and 4-year, respectively. In multivariate logistic analysis, high-volume hospitals had lower poor functional outcome at discharge than low-volume hospitals (odds ratio, 0.80; 95% confidence interval, 0.72–0.91; p<0.001). In the Cox analysis, high-volume hospitals had significantly lower 3-month, 1-year, 2-year, and 4-year mortality than low-volume hospitals (p<0.05).
Conclusion
: The poor outcome at discharge, short- and long-term mortality in ICH patients differed according to hospital volume. High-volume hospitals showed lower rates of mortality for ICH patients, particularly those with severe clinical status.
Keyword
Figure
Reference
-
References
1. Chiu D, Peterson L, Elkind MSV, Rosand J, Gerber LM, Silverstein MD, et al. Comparison of outcomes after intracerebral hemorrhage and ischemic stroke. J Stroke Cerebrovasc Dis. 19:225–229. 2010.
Article2. Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA. 283:1159–1166. 2000.3. Durairaj L, Torner JC, Chrischilles EA, Vaughan Sarrazin MS, Yankey J, Rosenthal GE. Hospital volume-outcome relationships among medical admissions to ICUs. Chest. 128:1682–1689. 2005.
Article4. Farley DE, Ozminkowski RJ. Volume-outcome relationships and in-hospital mortality: the effect of changes in volume over time. Med Care. 30:77–94. 1992.
Article5. Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke. 17:18–29. 2022.
Article6. Flaherty ML, Haverbusch M, Sekar P, Kissela B, Kleindorfer D, Moomaw CJ, et al. Long-term mortality after intracerebral hemorrhage. Neurology. 66:1182–1186. 2006.
Article7. Fletcher JJ, Kotagal V, Mammoser A, Peterson M, Morgenstern LB, Burke JF. Cost-effectiveness of transfers to centers with neurological intensive care units after intracerebral hemorrhage. Stroke. 46:58–64. 2015.
Article8. Fried TR, van Doorn C, O’Leary JR, Tinetti ME, Drickamer MA. Older person’s preferences for home vs hospital care in the treatment of acute illness. Arch Intern Med. 160:1501–1506. 2000.
Article9. Hacke W, Albers G, Al-Rawi Y, Bogousslavsky J, Davalos A, Eliasziw M, et al. The Desmoteplase in Acute Ischemic Stroke Trial (DIAS): a phase II MRI-based 9-hour window acute stroke thrombolysis trial with intravenous desmoteplase. Stroke. 36:66–73. 2005.
Article10. Hajian-Tilaki K. The choice of methods in determining the optimal cutoff value for quantitative diagnostic test evaluation. Stat Methods Med Res. 27:2374–2383. 2018.
Article11. Hall RE, Fang J, Hodwitz K, Saposnik G, Bayley MT. Does the volume of ischemic stroke admissions relate to clinical outcomes in the ontario stroke system? Circ Cardiovasc Qual Outcomes. 8(6 Suppl 3):S141–S147. 2015.
Article12. Hamilton BH, Ho V. Does practice make perfect? Examining the relationship between hospital surgical volume and outcomes for hip fracture patients in Quebec. Med Care. 36:892–903. 1998.13. Heit JJ, Iv M, Wintermark M. Imaging of intracranial hemorrhage. J Stroke. 19:11–27. 2017.
Article14. Heo NH, Lee MR, Yang KH, Hong OR, Shin JH, Lee BY, et al. Short- and long-term mortality after intravenous thrombolysis for acute ischemic stroke: a propensity score-matched cohort with 5-year follow-up. Medicine (Baltimore). 100:e27652. 2021.15. Jang WM, Lee J, Eun SJ, Yim J, Kim Y, Kwak MY. Travel time to emergency care not by geographic time, but by optimal time: a nationwide cross-sectional study for establishing optimal hospital access time to emergency medical care in South Korea. PLoS One. 16:e0251116. 2021.
Article16. Kim JY, Kang K, Kang J, Koo J, Kim DH, Kim BJ, et al. Executive summary of stroke statistics in Korea 2018: a report from the Epidemiology Research Council of the Korean Stroke Society. J Stroke. 21:42–59. 2019.
Article17. Kim YM, June KJ, Cho SH. Factors related to nurse staffing levels in tertiary and general hospitals. Taehan Kanho Hakhoe Chi. 35:1493–1499. 2005.
Article18. Lahr MM, Luijckx GJ, Vroomen PC, van der Zee DJ, Buskens E. Proportion of patients treated with thrombolysis in a centralized versus a decentralized acute stroke care setting. Stroke. 43:1336–1340. 2012.
Article19. Lee BY, Ha S, Lee YH. Association between volume of surgery for acute hemorrhagic stroke and mortality. Medicine (Baltimore). 97:e12105. 2018.
Article20. Lee DW, Moon HJ, Heo NH; KoCARC. Association between ambulance response time and neurologic outcome in patients with cardiac arrest. Am J Emerg Med. 37:1999–2003. 2019.
Article21. Lee JY, Heo NH, Lee MR, Ahn JM, Oh HJ, Shim JJ, et al. Short and long-term outcomes of subarachnoid hemorrhage treatment according to hospital volume in Korea: a nationwide multicenter registry. J Korean Med Sci. 36:e146. 2021.
Article22. Lee KJ, Kim JY, Kang J, Kim BJ, Kim SE, Oh H, et al. Hospital volume and mortality in acute ischemic stroke patients: effect of adjustment for stroke severity. J Stroke Cerebrovasc Dis. 29:104753. 2020.
Article23. Leifer D, Fonarow GC, Hellkamp A, Baker D, Hoh BL, Prabhakaran S, et al. Association between hospital volumes and clinical outcomes for patients with nontraumatic subarachnoid hemorrhage. J Am Heart Assoc. 10:e018373. 2021.
Article24. Lindner A, Kofler M, Rass V, Ianosi B, Gaasch M, Schiefecker AJ, et al. Early predictors for infectious complications in patients with spontaneous intracerebral hemorrhage and their impact on outcome. Front Neurol. 10:817. 2019.
Article25. Liu X, Zhou M, Zhao J, Gao Y, Wang Y, Zhou J, et al. Functional independence and disability evaluation in stroke patients: optimal cutoff scores for a pictorial-based longshi scale, barthel index, and modified rankin scale. Front Neurol. 13:710852. 2022.
Article26. Luft HS, Hunt SS, Maerki SC. The volume-outcome relationship: practice-makes-perfect or selective-referral patterns? Health Serv Res. 22:157–182. 1987.27. Luk JK, Cheung RT, Ho SL, Li L. Does age predict outcome in stroke rehabilitation? A study of 878 Chinese subjects. Cerebrovasc Dis. 21:229–234. 2006.
Article28. Mailles A, De Broucker T, Costanzo P, Martinez-Almoyna L, Vaillant V, Stahl JP, et al. Long-term outcome of patients presenting with acute infectious encephalitis of various causes in France. Clin Infect Dis. 54:1455–1464. 2012.
Article29. Sasichay-Akkadechanunt T, Scalzi CC, Jawad AF. The relationship between nurse staffing and patient outcomes. J Nurs Adm. 33:478–485. 2003.
Article30. Singla A, Simons J, Li Y, Csikesz NG, Ng SC, Tseng JF, et al. Admission volume determines outcome for patients with acute pancreatitis. Gastroenterology. 137:1995–2001. 2009.
Article31. Sobrino T, Hurtado O, Moro MA, Rodríguez-Yáñez M, Castellanos M, Brea D, et al. The increase of circulating endothelial progenitor cells after acute ischemic stroke is associated with good outcome. Stroke. 38:2759–2764. 2007.
Article32. Solomon RA, Mayer SA, Tarmey JJ. Relationship between the volume of craniotomies for cerebral aneurysm performed at New York state hospitals and in-hospital mortality. Stroke. 27:13–17. 1996.
Article33. Song SO, Jung CH, Song YD, Park CY, Kwon HS, Cha BS, et al. Background and data configuration process of a nationwide population-based study using the Korean national health insurance system. Diabetes Metab J. 38:395–403. 2014.
Article34. Starke RM, Komotar RJ, Kim GH, Kellner CP, Otten ML, Hahn DK, et al. Evaluation of a revised glasgow coma score scale in predicting long-term outcome of poor grade aneurysmal subarachnoid hemorrhage patients. J Clin Neurosci. 16:894–899. 2009.
Article35. Ungerer MN, Ringleb P, Reuter B, Stock C, Ippen F, Hyrenbach S, et al. Stroke unit admission is associated with better outcome and lower mortality in patients with intracerebral hemorrhage. Eur J Neurol. 27:825–832. 2020.36. Yoneda Y, Okuda S, Hamada R, Toyota A, Gotoh J, Watanabe M, et al. Hospital cost of ischemic stroke and intracerebral hemorrhage in Japanese stroke centers. Health Policy. 73:202–211. 2005.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Percutaneous Needle Aspiration for Evacuation of Intracerebral Hemorrhage: A Volumetric and Clincal Outcone Study
- Bilateral Simultaneous Hypertensive Intracerebral Hemorrhages in Both Thalami: A Case Report
- Recombinant Factor VIIa Treatment for Acute Intracerebral Hemorrhage
- A Clinical Analysis of 553 Cases of Hypertensive Intracerebral Hemorrhage
- Stereotatic Aspiration of Simultaneous Bilateral Spontaneous Intracerebral Hemorrhage: Case Report