J Korean Neurosurg Soc.
2024 Nov;67(6):602-608. 10.3340/jkns.2024.0121.
Enhancing Professional Awareness of Informed Consent : Safeguarding the Rights of Patients and Practitioners
- Affiliations
-
- 1Healthcare, Legal and Policy Center, Legal Research Institute of Korea University, Seoul, Korea
- KMID: 2560402
- DOI: http://doi.org/10.3340/jkns.2024.0121
Abstract
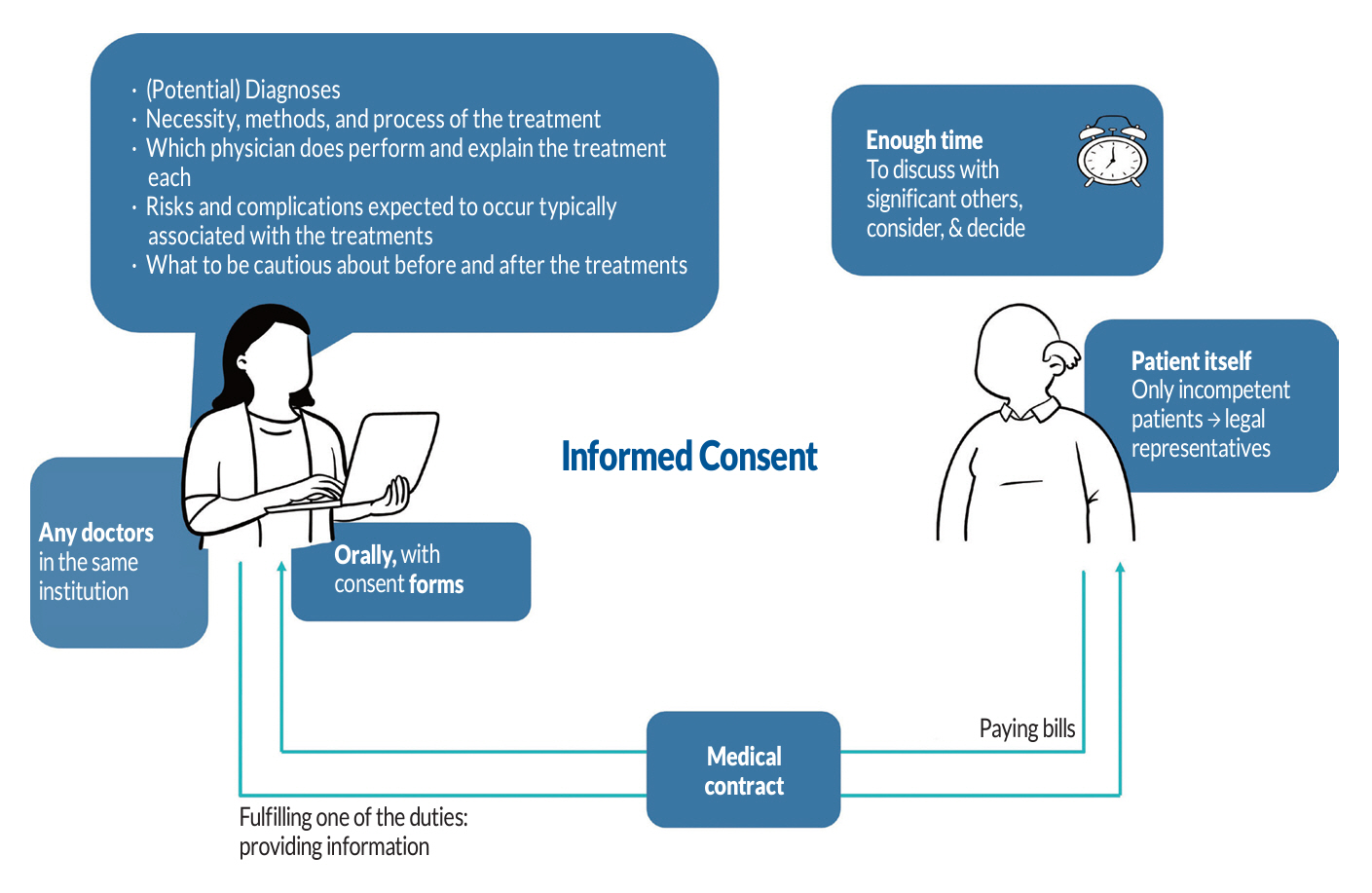
- Informed consent is a crucial communication process between doctors and patients for obtaining patients’ approval before initiating medical treatment. It is derived from the legal principles of medical contracts and requires doctors to explain the treatment process to patients. Surgeons should be aware of informed consent not only to avoid unnecessary litigation risks but also to provide patients with the right to self-determination. The aim of the study is to help surgeons in Korea understand the legal doctrine on informed consent for practical application. This article reviews the legal doctrine of informed consent according to 5W1H—why, who, whom, what, when, and how—with judicial cases to communicate effectively with patients in clinical settings. Irrespective of the seniority and rank of a doctor, they have the responsibility to provide patients with the information required to protect their right to self-determination. Informed consent should be advanced for patients to consider, discuss with significant others, and determine whether or not to undergo medical treatment. At that stage, patients need to be informed of the necessity, risks, and so on. The most common method of informed consent is an oral explanation utilizing certain forms for documentation. However, the informed consent of patients can be exempted on certain occasions. Optimal informed consent, when implemented, leads to patient-centered care, which significantly improves patient satisfaction and outcomes. Ultimately, it not only protects doctors from litigation risks but also upholds patients’ autonomy.
Figure
Reference
-
References
1. Alomar AZ. Confidence level, challenges, and obstacles faced by orthopedic residents in obtaining informed consent. J Orthop Surg Res. 16:390. 2021.
Article2. American Medical Association. The AMA Code of Medical Ethics. Available at : https://code-medical-ethics.ama-assn.org/.3. American Medical Association; New York Academy of Medicine. Code of medical ethics. New York: H. Ludwig & Company;1848.4. Baek K. A study on recent discussions ahout the pysician's explanation in medical litigation. Korean Soc Law Med. 24:37–63. 2023.
Article5. Baek K, Ahn Y, Kim N, Kim M. A study on the nurse in charge of education's current status and legal status. Korean Soc Law Med. 14:261–280. 2013.6. Beauchamp TL. Autonomy and consent. In : Miller FG, Wertheimer A, editors. The ethics of consent: theory and practice. New York: Oxford University Press;2010. p. 55–78.7. Beauchamp TL, Childress JF. Principles of biomedical ethics. ed 8th. New York: Oxford University Press;2019.8. Berg JW, Appelbaum PS, Lidz CW, Parker LS, Berg JW, Appelbaum PS, et al. Exceptions to the legal requirements: emergency, waiver, therapeutic privilege, and compulsory treatment : Informed consent: legal theory and clinical practice. Oxford: Oxford University Press;2001.9. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 155:97–107. 2011.
Article10. Buchner B, Freye M. Informed Consent in German Medical Law: Finding the right path between patient autonomy and information overload. Bremen: Proceedings of the Young Universities for the Future of Europe Law Conferences;2021.11. Chin JJ. Doctor-patient relationship: from medical paternalism to enhanced autonomy. Singapore Med J. 43:152–155. 2002.12. General Medical Council. Guidance on professional standards and ethics for doctors: Decision making and consent. Manchester: General Medical Council;2020.13. Giudici-Wach K, Gillois P, Remen T, Claudot F. Learning from informed consent litigation to improve practices: a systematic review. Patient Educ Couns. 105:1714–1721. 2022.
Article14. Huang D. The concept of “self-government” across cultures: from the western world to Japan and China. Cultura. 15:53–72. 2018.
Article15. Hyun D. A critical review on informed consent in the revised Medical Law. Korean Soc Law Med. 18:3–35. 2017.16. Jang C. A study on the doctor's explanation of obligation: on the basis of protective interests. Ajou Law Rev. 13:80–100. 2019.17. Jefford M, Moore R. Improvement of informed consent and the quality of consent documents. Lancet Oncol. 9:485–493. 2008.
Article18. Korea Medical Dispute Mediation and Arbitration Agency. Medical dispute mediation and arbitration statistical yearbook 2023. Seoul: Korea Medical Dispute Mediation and Arbitration Agency;2024.19. Lee JH. Explanation duty of doctor in case the malpractice suit. J Law Res. 12:5–38. 2014.20. Lin YK, Liu KT, Chen CW, Lee WC, Lin CJ, Shi L, et al. How to effectively obtain informed consent in trauma patients: a systematic review. BMC Med Ethics. 20:8. 2019.
Article21. Park J, Park H. Surgical informed consent process in neurosurgery. J Korean Neurosurg Soc. 60:385–390. 2017.
Article22. Quill TE, Brody H. Physician recommendations and patient autonomy: finding a balance between physician power and patient choice. Ann Intern Med. 125:763–769. 1996.
Article23. Rubenfeld J. The right of privacy. Harv Law Rev. 737–807. 1989.
Article24. Seoul Central District Court. 2014Gahab509854. Decision of May 18, 2016.25. Shah P, Thornton I, Turrin D, Hipskind JE. Informed consent : StatPearls [Internet]. Treasure Island: StatPearls Publishing;2023.26. Shin HH, Baek KH. The theory and practice of medical disputes. Seoul: Parkyoungsa;2022.27. Suk H. The functional classification of physician’s duty of information and liability for violation of the duty. Korean Soc Law Med. 18:3–46. 2017.28. Supreme Court of Korea. 2005Da5867. Decision of May 31, 2007.29. Supreme Court of Korea. 2009Da17417. Decision of May 21, 2009.30. Supreme Court of Korea. 2009Da70906. Decision of Nov 24, 2011.31. Supreme Court of Korea. 2021Da265010. Decision of Jan 27, 2022.32. Supreme Court of Korea. 94Da3421. Decision of Jan 20, 1995.33. Supreme Court of Korea. 94Da35674. Decision of Nov 25, 1994.34. Supreme Court of Korea. 99Da10479. Decision of Sep 3, 1999.35. Supreme Court of Korea. 2020Na22793. Decision of Oct 13, 2022.36. The Joint Commission. Informed consent: more than getting a signature. Quick Saf. 21:1–3. 2016.37. Uijeongbu District Court. 2015Gadan111549. Decision of Dec 7, 2016.38. The Emergency Medical Service Act. Amended by Act No. 19654, Aug 16, 2023.39. The Medical Service Act. Amended by Act No. 19421, May 19, 2023.40. The Constitution of the Republic of Korea. Wholly Amended by the Constitution No. 10, Oct 29, 1987.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 'Informed Consent' in Public Health Activities: Based on the Universal Declaration on Bioethics and Human Rights, UNESCO
- Anesthetic Informed Consent
- Legal Issues Concerning Informed Consent
- Knowledge and Attitude Toward Informed Consent Among Private Dental Practitioners in Bathinda City, Punjab, India
- Informed Consent in Psychiatry