Cardiovasc Prev Pharmacother.
2024 Oct;6(4):128-134. 10.36011/cpp.2024.6.e13.
Use of dual-energy x-ray absorptiometry for body composition in chronic disease management
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2560385
- DOI: http://doi.org/10.36011/cpp.2024.6.e13
Abstract
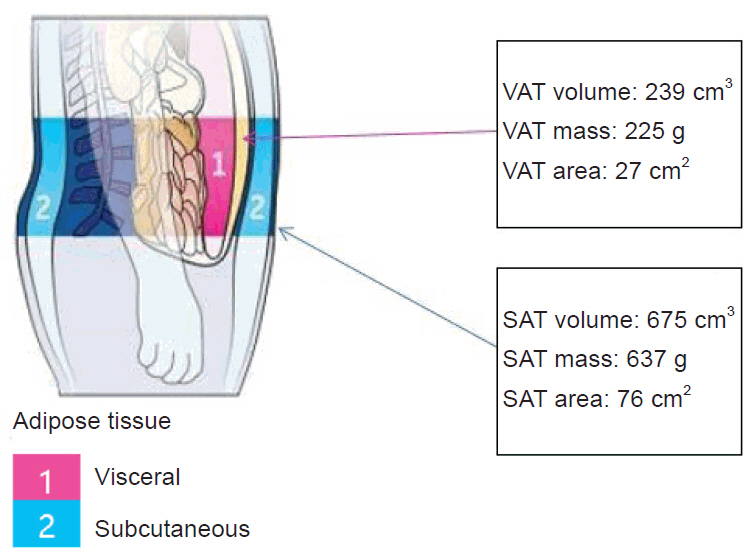
- As individuals age or contend with chronic diseases, shifts in body composition often emerge, characterized by a loss of muscle mass and an increase in fat mass, even among those with stable body weight. Both obesity and sarcopenia are key drivers of frailty, disability, and heightened morbidity and mortality. The simultaneous decline in skeletal muscle and accumulation of visceral fat can work synergistically, magnifying their detrimental effects on physical function and metabolic health. Today, dual-energy x-ray absorptiometry (DEXA) is widely recognized as one of the most versatile imaging techniques for assessing not only osteoporosis but also sarcopenia and obesity. Whole-body DEXA facilitates comprehensive analysis, offering detailed insights into fat mass, non-bone lean mass, and bone mineral content at both total and regional levels. DEXA is highly valued for its accuracy, reproducibility, speed, affordability, and low radiation exposure. Furthermore, advancements in DEXA technology and software now allow for precise estimation of visceral adipose tissue. This review underscores the clinical applications of whole-body DEXA, focusing on the use of muscle and fat mass indices in diagnosing low muscle mass, sarcopenia, and sarcopenic obesity, aligned with the latest research and guidelines.
Figure
Reference
-
1. Roubenoff R. Sarcopenic obesity: the confluence of two epidemics. Obes Res. 2004; 12:887–8.
Article2. Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001; 286:1195–200.
Article3. Kim TN, Choi KM. The implications of sarcopenia and sarcopenic obesity on cardiometabolic disease. J Cell Biochem. 2015; 116:1171–8.
Article4. Nam GE, Kim YH, Han K, Jung JH, Rhee EJ, Lee WY, et al. Obesity fact sheet in Korea, 2020: prevalence of obesity by obesity class from 2009 to 2018. J Obes Metab Syndr. 2021; 30:141–8.
Article5. Nam GE, Kim YH, Han K, Jung JH, Rhee EJ, Lee SS, et al. Obesity fact sheet in Korea, 2019: prevalence of obesity and abdominal obesity from 2009 to 2018 and social factors. J Obes Metab Syndr. 2020; 29:124–32.
Article6. Zamboni M, Mazzali G, Zoico E, Harris TB, Meigs JB, Di Francesco V, et al. Health consequences of obesity in the elderly: a review of four unresolved questions. Int J Obes (Lond). 2005; 29:1011–29.
Article7. Zamboni M, Mazzali G, Fantin F, Rossi A, Di Francesco V. Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovasc Dis. 2008; 18:388–95.
Article8. Kim TN, Yang SJ, Yoo HJ, Lim KI, Kang HJ, Song W, et al. Prevalence of sarcopenia and sarcopenic obesity in Korean adults: the Korean sarcopenic obesity study. Int J Obes (Lond). 2009; 33:885–92.
Article9. Kim TN, Park MS, Lim KI, Yang SJ, Yoo HJ, Kang HJ, et al. Skeletal muscle mass to visceral fat area ratio is associated with metabolic syndrome and arterial stiffness: the Korean Sarcopenic Obesity Study (KSOS). Diabetes Res Clin Pract. 2011; 93:285–91.
Article10. Prado CM, Wells JC, Smith SR, Stephan BC, Siervo M. Sarcopenic obesity: a critical appraisal of the current evidence. Clin Nutr. 2012; 31:583–601.
Article11. Johnson Stoklossa CA, Sharma AM, Forhan M, Siervo M, Padwal RS, Prado CM. Prevalence of sarcopenic obesity in adults with class II/III obesity using different diagnostic criteria. J Nutr Metab. 2017; 2017:7307618.12. Kalinkovich A, Livshits G. Sarcopenic obesity or obese sarcopenia: a cross talk between age-associated adipose tissue and skeletal muscle inflammation as a main mechanism of the pathogenesis. Ageing Res Rev. 2017; 35:200–21.
Article13. Barbat-Artigas S, Pion CH, Leduc-Gaudet JP, Rolland Y, Aubertin-Leheudre M. Exploring the role of muscle mass, obesity, and age in the relationship between muscle quality and physical function. J Am Med Dir Assoc. 2014; 15:303.
Article14. Tian S, Xu Y. Association of sarcopenic obesity with the risk of all-cause mortality: a meta-analysis of prospective cohort studies. Geriatr Gerontol Int. 2016; 16:155–66.
Article15. Newman AB, Haggerty CL, Goodpaster B, Harris T, Kritchevsky S, Nevitt M, et al. Strength and muscle quality in a well-functioning cohort of older adults: the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2003; 51:323–30.
Article16. Wang ZM, Pierson RN Jr, Heymsfield SB. The five-level model: a new approach to organizing body-composition research. Am J Clin Nutr. 1992; 56:19–28.
Article17. Rico H, Revilla M, Villa LF, Alvarez de Buergo M. Age-related differences in total and regional bone mass: a cross-sectional study with DXA in 429 normal women. Osteoporos Int. 1993; 3:154–9.
Article18. Buckley DC, Kudsk KA, Rose BS, Fatzinger P, Koetting CA, Schlatter M. Anthropometric and computerized tomographic measurements of lower extremity lean body mass. J Am Diet Assoc. 1987; 87:196–9.
Article19. Heymsfield SB, McManus C, Smith J, Stevens V, Nixon DW. Anthropometric measurement of muscle mass: revised equations for calculating bone-free arm muscle area. Am J Clin Nutr. 1982; 36:680–90.
Article20. van der Kooy K, Seidell JC. Techniques for the measurement of visceral fat: a practical guide. Int J Obes Relat Metab Disord. 1993; 17:187–96.21. Plourde G. The role of radiologic methods in assessing body composition and related metabolic parameters. Nutr Rev. 1997; 55:289–96.
Article22. Adams JE. Single and dual energy X-ray absorptiometry. Eur Radiol. 1997; 7:20–31.
Article23. Andreoli A, Scalzo G, Masala S, Tarantino U, Guglielmi G. Body composition assessment by dual-energy X-ray absorptiometry (DXA). Radiol Med. 2009; 114:286–300.
Article24. Albanese CV, Diessel E, Genant HK. Clinical applications of body composition measurements using DXA. J Clin Densitom. 2003; 6:75–85.
Article25. Cawthon PM. Assessment of lean mass and physical performance in sarcopenia. J Clin Densitom. 2015; 18:467–71.
Article26. Kendler DL, Borges JL, Fielding RA, Itabashi A, Krueger D, Mulligan K, et al. The official positions of the International Society for Clinical Densitometry: indications of use and reporting of DXA for body composition. J Clin Densitom. 2013; 16:496–507.
Article27. Petak S, Barbu CG, Yu EW, Fielding R, Mulligan K, Sabowitz B, et al. The official positions of the International Society for Clinical Densitometry: body composition analysis reporting. J Clin Densitom. 2013; 16:508–19.
Article28. Kim KM, Jang HC, Lim S. Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia. Korean J Intern Med. 2016; 31:643–50.
Article29. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010; 39:412–23.30. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48:601.
Article31. Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020; 21:300–7.
Article32. Baker JF, Long J, Leonard MB, Harris T, Delmonico MJ, Santanasto A, et al. Estimation of skeletal muscle mass relative to adiposity improves prediction of physical performance and incident disability. J Gerontol A Biol Sci Med Sci. 2018; 73:946–52.
Article33. Kim TN, Park MS, Kim YJ, Lee EJ, Kim MK, Kim JM, et al. Association of low muscle mass and combined low muscle mass and visceral obesity with low cardiorespiratory fitness. PLoS One. 2014; 9:e100118.
Article34. Shea JL, King MT, Yi Y, Gulliver W, Sun G. Body fat percentage is associated with cardiometabolic dysregulation in BMI-defined normal weight subjects. Nutr Metab Cardiovasc Dis. 2012; 22:741–7.
Article35. Carey DG, Jenkins AB, Campbell LV, Freund J, Chisholm DJ. Abdominal fat and insulin resistance in normal and overweight women: direct measurements reveal a strong relationship in subjects at both low and high risk of NIDDM. Diabetes. 1996; 45:633–8.
Article36. Brochu M, Starling RD, Tchernof A, Matthews DE, Garcia-Rubi E, Poehlman ET. Visceral adipose tissue is an independent correlate of glucose disposal in older obese postmenopausal women. J Clin Endocrinol Metab. 2000; 85:2378–84.
Article37. Bazzocchi A, Ponti F, Albisinni U, Battista G, Guglielmi G. DXA: technical aspects and application. Eur J Radiol. 2016; 85:1481–92.
Article38. Karpe F, Pinnick KE. Biology of upper-body and lower-body adipose tissue: link to whole-body phenotypes. Nat Rev Endocrinol. 2015; 11:90–100.
Article39. Muller MJ, Lagerpusch M, Enderle J, Schautz B, Heller M, Bosy-Westphal A. Beyond the body mass index: tracking body composition in the pathogenesis of obesity and the metabolic syndrome. Obes Rev. 2012; 13 Suppl 2:6–13.40. Micklesfield LK, Goedecke JH, Punyanitya M, Wilson KE, Kelly TL. Dual-energy x-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity (Silver Spring). 2012; 20:1109–14.
Article41. Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R. Visceral fat is an independent predictor of all-cause mortality in men. Obesity (Silver Spring). 2006; 14:336–41.
Article42. Kim TN, Park MS, Ryu JY, Choi HY, Hong HC, Yoo HJ, et al. Impact of visceral fat on skeletal muscle mass and vice versa in a prospective cohort study: the Korean Sarcopenic Obesity Study (KSOS). PLoS One. 2014; 9:e115407.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of Dual-Energy X-ray Absorptiometry for Body Composition in Chronic Disease Management
- Validity of Bioelectrical Impedance Analysis (BIA) in Measurement of Human Body Composition
- Comparison between Dual Energy X-ray Absorptiometry (DEXA) and Bioelectrical Impedence Analysis (BIA) in Measurement of Lean Body Mass and Fat Mass in Obese Adults: Based Bland-Altman Plot Analysis
- Need for Cross-calibration of Body Composition Even with the Same Model of Dual-energy X-ray Absorptiometry
- Dual-Energy X-Ray Absorptiometry: Beyond Bone Mineral Density Determination