Intest Res.
2024 Oct;22(4):397-413. 10.5217/ir.2024.00003.
What to do when traditional rescue therapies fail in acute severe ulcerative colitis
- Affiliations
-
- 1Department of Gastroenterology, Austin Health, Melbourne, Australia
- 2Department of Medicine, Austin Academic Centre, University of Melbourne, Melbourne, Australia
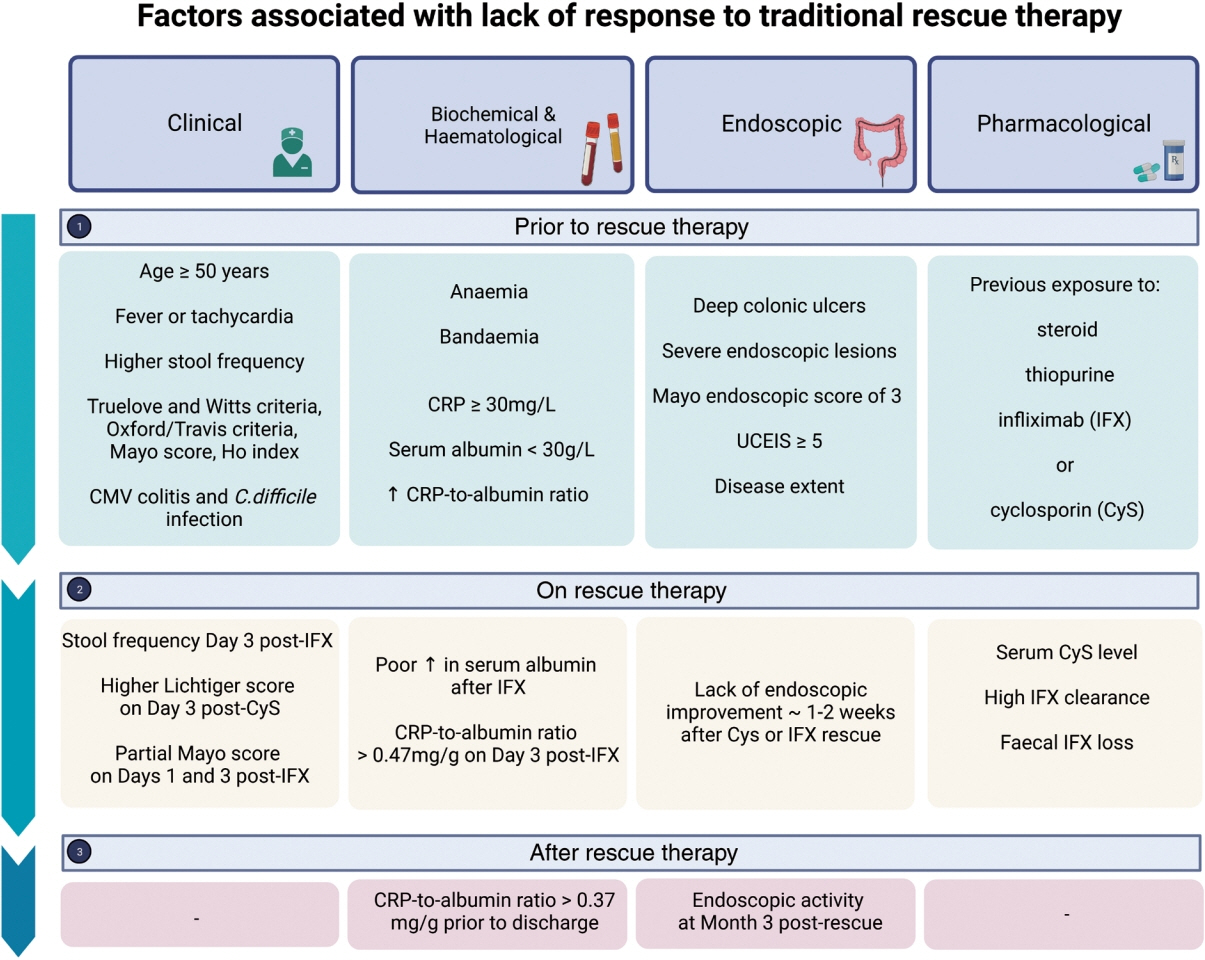
- KMID: 2560291
- DOI: http://doi.org/10.5217/ir.2024.00003
Abstract
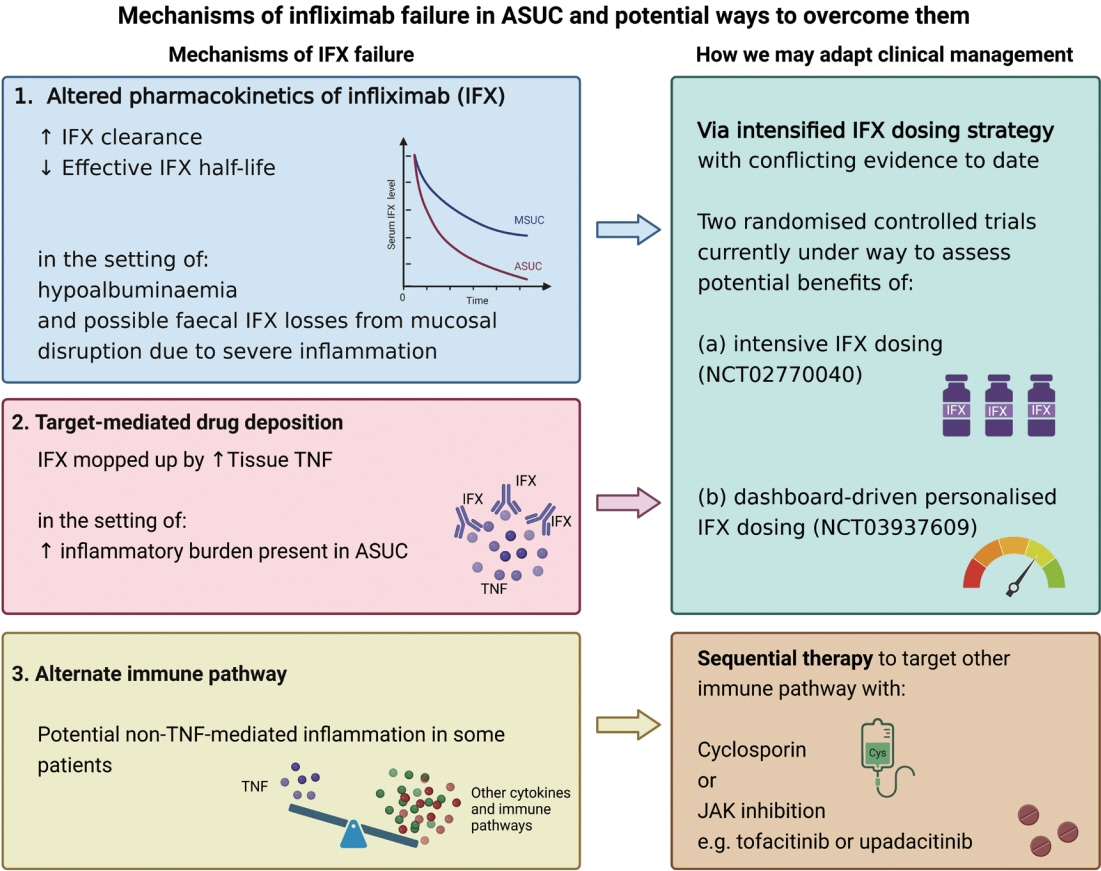
- Acute severe ulcerative colitis (ASUC) is a medical emergency that affects approximately 25% of patients with ulcerative colitis at some point in time in their lives. Outcomes of ASUC are highly variable. Approximately 30% of patients do not respond to corticosteroids and up to 50% of patients do not respond to rescue therapy (infliximab or cyclosporin) and require emergency colectomy. Data are emerging on infliximab dosing strategies, use of cyclosporin as a bridge to slower acting biologic agents and Janus kinase inhibition as primary and sequential therapy. In this review, we outline contemporary approaches to clinical management of ASUC in the setting of failure to respond to traditional rescue therapies.
Keyword
Figure
Reference
-
1. Dinesen LC, Walsh AJ, Protic MN, et al. The pattern and outcome of acute severe colitis. J Crohns Colitis. 2010; 4:431–437.2. Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955; 2:1041–1048.3. Seah D, De Cruz P. Review article: the practical management of acute severe ulcerative colitis. Aliment Pharmacol Ther. 2016; 43:482–513.4. Turner D, Walsh CM, Steinhart AH, Griffiths AM. Response to corticosteroids in severe ulcerative colitis: a systematic review of the literature and a meta-regression. Clin Gastroenterol Hepatol. 2007; 5:103–110.
Article5. Laharie D, Bourreille A, Branche J, et al. Ciclosporin versus infliximab in patients with severe ulcerative colitis refractory to intravenous steroids: a parallel, open-label randomised controlled trial. Lancet. 2012; 380:1909–1915.6. Narula N, Marshall JK, Colombel JF, et al. Systematic review and meta-analysis: infliximab or cyclosporine as rescue therapy in patients with severe ulcerative colitis refractory to steroids. Am J Gastroenterol. 2016; 111:477–491.7. Li Wai Suen CF, Seah D, Choy MC, De Cruz P. Factors associated with response to rescue therapy in acute severe ulcerative colitis. Inflamm Bowel Dis. 2024; 30:1389–1405.
Article8. Gibson DJ, Heetun ZS, Redmond CE, et al. An accelerated infliximab induction regimen reduces the need for early colectomy in patients with acute severe ulcerative colitis. Clin Gastroenterol Hepatol. 2015; 13:330–335.9. Choy MC, Seah D, Faleck DM, et al. Systematic review and meta-analysis: optimal salvage therapy in acute severe ulcerative colitis. Inflamm Bowel Dis. 2019; 25:1169–1186.10. Berinstein JA, Steiner CA, Regal RE, et al. Efficacy of induction therapy with high-intensity tofacitinib in 4 patients with acute severe ulcerative colitis. Clin Gastroenterol Hepatol. 2019; 17:988–990.
Article11. Zinger CH, Ringel Y, Eitan M, et al. Upadacitinib for acute severe ulcerative colitis. Inflamm Bowel Dis. 2023; 29:1667–1669.12. Williams JG, Alam MF, Alrubaiy L, et al. Infliximab versus ciclosporin for steroid-resistant acute severe ulcerative colitis (CONSTRUCT): a mixed methods, open-label, pragmatic randomised trial. Lancet Gastroenterol Hepatol. 2016; 1:15–24.13. Weissman S, Chris-Olaiya A, Mehta TI, et al. A novel player: cyclosporine therapy in the management of inflammatory bowel disease. Transl Gastroenterol Hepatol. 2019; 4:67.
Article14. Lichtiger S, Present DH, Kornbluth A, et al. Cyclosporine in severe ulcerative colitis refractory to steroid therapy. N Engl J Med. 1994; 330:1841–1845.
Article15. D’Haens G, Lemmens L, Geboes K, et al. Intravenous cyclosporine versus intravenous corticosteroids as single therapy for severe attacks of ulcerative colitis. Gastroenterology. 2001; 120:1323–1329.16. Croft A, Walsh A, Doecke J, Cooley R, Howlett M, RadfordSmith G. Outcomes of salvage therapy for steroid-refractory acute severe ulcerative colitis: ciclosporin vs. infliximab. Aliment Pharmacol Ther. 2013; 38:294–302.17. Molnár T, Farkas K, Szepes Z, et al. Long-term outcome of cyclosporin rescue therapy in acute, steroid-refractory severe ulcerative colitis. United European Gastroenterol J. 2014; 2:108–112.
Article18. Sternthal MB, Murphy SJ, George J, Kornbluth A, Lichtiger S, Present DH. Adverse events associated with the use of cyclosporine in patients with inflammatory bowel disease. Am J Gastroenterol. 2008; 103:937–943.
Article19. Van Assche G, D’Haens G, Noman M, et al. Randomized, double-blind comparison of 4 mg/kg versus 2 mg/kg intravenous cyclosporine in severe ulcerative colitis. Gastroenterology. 2003; 125:1025–1031.
Article20. Lamb CA, Kennedy NA, Raine T, et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019; 68(Suppl 3):s1–s106.
Article21. Berends SE, van Steeg TJ, Ahsman MJ, et al. Tumor necrosis factor-mediated disposition of infliximab in ulcerative colitis patients. J Pharmacokinet Pharmacodyn. 2019; 46:543–551.22. Guo Y, Lu N, Bai A. Clinical use and mechanisms of infliximab treatment on inflammatory bowel disease: a recent update. Biomed Res Int. 2013; 2013:581631.
Article23. Van den Brande JM, Braat H, van den Brink GR, et al. Infliximab but not etanercept induces apoptosis in lamina propria T-lymphocytes from patients with Crohn’s disease. Gastroenterology. 2003; 124:1774–1785.
Article24. Veltkamp C, Anstaett M, Wahl K, et al. Apoptosis of regulatory T lymphocytes is increased in chronic inflammatory bowel disease and reversed by anti-TNFα treatment. Gut. 2011; 60:1345–1353.
Article25. Sands BE, Tremaine WJ, Sandborn WJ, et al. Infliximab in the treatment of severe, steroid-refractory ulcerative colitis: a pilot study. Inflamm Bowel Dis. 2001; 7:83–88.
Article26. Järnerot G, Hertervig E, Friis-Liby I, et al. Infliximab as rescue therapy in severe to moderately severe ulcerative colitis: a randomized, placebo-controlled study. Gastroenterology. 2005; 128:1805–1811.27. Ochsenkühn T, Sackmann M, Göke B. Infliximab for acute, not steroid-refractory ulcerative colitis: a randomized pilot study. Eur J Gastroenterol Hepatol. 2004; 16:1167–1171.28. Halpin SJ, Hamlin PJ, Greer DP, Warren L, Ford AC. Efficacy of infliximab in acute severe ulcerative colitis: a single-centre experience. World J Gastroenterol. 2013; 19:1091–1097.
Article29. Pola S, Patel D, Ramamoorthy S, et al. Strategies for the care of adults hospitalized for active ulcerative colitis. Clin Gastroenterol Hepatol. 2012; 10:1315–1325.
Article30. Gordon BL, Battat R. Therapeutic drug monitoring of infliximab in acute severe ulcerative colitis. J Clin Med. 2023; 12:3378.
Article31. Fiske J, Conley T, Sebastian S, Subramanian S. Infliximab in acute severe colitis: getting the right dose. Frontline Gastroenterol. 2020; 11:427–429.32. Kevans D, Murthy S, Mould DR, Silverberg MS. Accelerated clearance of infliximab is associated with treatment failure in patients with corticosteroid-refractory acute ulcerative colitis. J Crohns Colitis. 2018; 12:662–669.
Article33. Kennedy NA, Heap GA, Green HD, et al. Predictors of anti-TNF treatment failure in anti-TNF-naive patients with active luminal Crohn’s disease: a prospective, multicentre, cohort study. Lancet Gastroenterol Hepatol. 2019; 4:341–353.34. Gisbert JP, García MJ, Chaparro M. Rescue therapies for steroidrefractory acute severe ulcerative colitis: a review. J Crohns Colitis. 2023; 17:972–994.
Article35. Rosen MJ, Minar P, Vinks AA. Review article: applying pharmacokinetics to optimise dosing of anti-TNF biologics in acute severe ulcerative colitis. Aliment Pharmacol Ther. 2015; 41:1094–1103.
Article36. Battat R, Hemperly A, Truong S, et al. Baseline clearance of infliximab is associated with requirement for colectomy in patients with acute severe ulcerative colitis. Clin Gastroenterol Hepatol. 2021; 19:511–518.37. Vande Casteele N, Jeyarajah J, Jairath V, Feagan BG, Sandborn WJ. Infliximab exposure-response relationship and thresholds associated with endoscopic healing in patients with ulcerative colitis. Clin Gastroenterol Hepatol. 2019; 17:1814–1821.
Article38. Poullenot F, Nivet D, Paul S, Riviere P, Roblin X, Laharie D. Severe endoscopic lesions are not associated with more infliximab fecal loss in acute severe ulcerative colitis. Dig Liver Dis. 2018; 50:1100–1103.
Article39. Mager DE. Target-mediated drug disposition and dynamics. Biochem Pharmacol. 2006; 72:1–10.
Article40. Yarur AJ, Jain A, Sussman DA, et al. The association of tissue anti-TNF drug levels with serological and endoscopic disease activity in inflammatory bowel disease: the ATLAS study. Gut. 2016; 65:249–255.
Article41. Olsen T, Goll R, Cui G, et al. Tissue levels of tumor necrosis factor-alpha correlates with grade of inflammation in untreated ulcerative colitis. Scand J Gastroenterol. 2007; 42:1312–1320.42. Gilmore R, Hilley P, Srinivasan A, Choy M, De Cruz P. Sequential use of high-dose tofacitinib after infliximab salvage therapy in acute severe ulcerative colitis. J Crohns Colitis. 2022; 16:166–168.
Article43. Weisshof R, Ollech JE, El Jurdi K, et al. Ciclosporin therapy after infliximab failure in hospitalized patients with acute severe colitis is effective and safe. J Crohns Colitis. 2019; 13:1105–1110.
Article44. Uzzan M, Bresteau C, Laharie D, et al. Tofacitinib as salvage therapy for 55 patients hospitalised with refractory severe ulcerative colitis: a GETAID cohort. Aliment Pharmacol Ther. 2021; 54:312–319.
Article45. Berinstein JA, Sheehan JL, Dias M, et al. Tofacitinib for biologic-experienced hospitalized patients with acute severe ulcerative colitis: a retrospective case-control study. Clin Gastroenterol Hepatol. 2021; 19:2112–2120.
Article46. Eqbal A, Hilley P, Choy M, Srinivasan A, de Cruz P. Outcomes out to 12 months after sequential use of high-dose tofacitinib following infliximab in acute severe ulcerative colitis. Intern Med J. 2023; 53:1497–1500.47. Xiao Y, Benoit N, Sedano R, et al. Effectiveness of tofacitinib for hospitalized patients with acute severe ulcerative colitis: case series. Dig Dis Sci. 2022; 67:5213–5219.
Article48. Honap S, Pavlidis P, Ray S, et al. Tofacitinib in acute severe ulcerative colitis: a real-world tertiary center experience. Inflamm Bowel Dis. 2020; 26:e147. –e149.49. Gilmore R, Tan WL, Fernandes R, An YK, Begun J. Upadacitinib salvage therapy for infliximab-experienced patients with acute severe ulcerative colitis. J Crohns Colitis. 2023; 17:2033–2036.
Article50. Berinstein J, Levine J, Satishchandran A, et al. Tu1769 Off-label, high-intensity upadacitinib for hospitalized patients with severe inflammatory bowel disease. Gastroenterology. 2023; 164:S–1118-S-1119.
Article51. Daniel F, Loriot MA, Seksik P, et al. Multidrug resistance gene1 polymorphisms and resistance to cyclosporine A in patients with steroid resistant ulcerative colitis. Inflamm Bowel Dis. 2007; 13:19–23.52. Hebert MF. Contributions of hepatic and intestinal metabolism and P-glycoprotein to cyclosporine and tacrolimus oral drug delivery. Adv Drug Deliv Rev. 1997; 27:201–214.
Article53. Burckart GJ, Starzl TE, Venkataramanan R, et al. Excretion of cyclosporine and its metabolites in human bile. Transplant Proc. 1986; 18(6 Suppl 5):46–49.54. Wang CE, Lu KP, Chang Z, Guo ML, Qiao HL. Association of CYP3A4*1B genotype with cyclosporin A pharmacokinetics in renal transplant recipients: a meta-analysis. Gene. 2018; 664:44–49.
Article55. Hole K, Wollmann BM, Nguyen C, Haslemo T, Molden E. Comparison of CYP3A4-inducing capacity of enzyme-inducing antiepileptic drugs using 4β-hydroxycholesterol as biomarker. Ther Drug Monit. 2018; 40:463–468.
Article56. Takaya S, Zaghloul I, Iwatsuki S, et al. Effect of liver dysfunction on cyclosporine pharmacokinetics. Transplant Proc. 1987; 19(1 Pt 2):1246–1247.57. Narula N, Fine M, Colombel JF, Marshall JK, Reinisch W. Systematic review: sequential rescue therapy in severe ulcerative colitis: do the benefits outweigh the risks? Inflamm Bowel Dis. 2015; 21:1683–1694.58. Bercier B, Niland B. S2282 Use of tofacitinib as rescue therapy in a biologic-experienced patient hospitalized with acute severe ulcerative colitis. Am J Gastroenterol. 2020; 115:S1207.59. Chen CY, Davis E, White L, Patrick D. Tofacitinib-induced remission of infliximab-refractory acute severe ulcerative colitis: a case report. J Gastroenterol Hepatol. 2020; 35:130–131.60. Griller N, Cohen L. Rapid onset of tofacitinib induction therapy for the treatment of ulcerative colitis. Clin Gastroenterol Hepatol. 2019; 17:1213.
Article61. Khan M, Mushtaq K, Yakoob R, AlSoub D. High dose tofacitinib as salvage therapy in steroid refractory acute severe ulcerative colitis following non-response to infliximab. Gastroenterology. 2022; 162:S107.62. Yang Q, Chen L, Feng L, et al. Success of cyclosporin and tofacitinib combination therapy in a patient with severe steroidrefractory ulcerative colitis. Inflamm Bowel Dis. 2021; 27:e157–e158.
Article63. Jena A, Mishra S, Sachan A, Singh H, Singh AK, Sharma V. Tofacitinib in acute severe ulcerative colitis: case series and a systematic review. Inflamm Bowel Dis. 2021; 27:e101–e103.
Article64. Constant BD, Baldassano R, Kirsch J, Mitchel EB, Stein R, Albenberg L. Tofacitinib salvage therapy for children hospitalized for corticosteroid- and biologic-refractory ulcerative colitis. J Pediatr Gastroenterol Nutr. 2022; 75:724–730.
Article65. Rutka M, Pigniczki D, Molnár T. Tofacitinib therapy, the lender of last resort. J Crohns Colitis. 2021; 15:694.
Article66. Kotwani P, Terdiman J, Lewin S. Tofacitinib for rescue therapy in acute severe ulcerative colitis: a real-world experience. J Crohns Colitis. 2020; 14:1026–1028.67. Santos S, Gamelas V, Saraiva R, Simões G, Saiote J, Ramos J. Tofacitinib: an option for acute severe ulcerative colitis? GE Port J Gastroenterol. 2021; 29:132–134.
Article68. Sedano R, Jairath V. High-dose rescue tofacitinib prevented inpatient colectomy in acute severe ulcerative colitis refractory to anti-TNF. Inflamm Bowel Dis. 2021; 27:e59–e60.
Article69. Naganuma M, Kobayashi T, Kunisaki R, et al. Real-world efficacy and safety of advanced therapies in hospitalized patients with ulcerative colitis. J Gastroenterol. 2023; 58:1198–1210.70. Danese S, Grisham M, Hodge J, Telliez JB. JAK inhibition using tofacitinib for inflammatory bowel disease treatment: a hub for multiple inflammatory cytokines. Am J Physiol Gastrointest Liver Physiol. 2016; 310:G155–G162.
Article71. Fernández-Clotet A, Castro-Poceiro J, Panés J. Tofacitinib for the treatment of ulcerative colitis. Expert Rev Clin Immunol. 2018; 14:881–892.72. Parmentier JM, Voss J, Graff C, et al. In vitro and in vivo characterization of the JAK1 selectivity of Upadacitinib (ABT-494). BMC Rheumatol. 2018; 2:23.
Article73. Ali NM, Shehab MA. Upadacitinib as a rescue therapy in acute severe ulcerative colitis: a case report and review of the literature. Am J Case Rep. 2023; 24:e940966.
Article74. Salameh R, Kirchgesner J, Allez M, et al. Long-term outcome of patients with acute severe ulcerative colitis responding to intravenous steroids. Aliment Pharmacol Ther. 2020; 51:1096–1104.
Article75. Feagan BG, Rutgeerts P, Sands BE, et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013; 369:699–710.
Article76. Ollech JE, Dwadasi S, Rai V, et al. Efficacy and safety of induction therapy with calcineurin inhibitors followed by vedolizumab maintenance in 71 patients with severe steroid-refractory ulcerative colitis. Aliment Pharmacol Ther. 2020; 51:637–643.77. Pellet G, Stefanescu C, Carbonnel F, et al. Efficacy and safety of induction therapy with calcineurin inhibitors in combination with vedolizumab in patients with refractory ulcerative colitis. Clin Gastroenterol Hepatol. 2019; 17:494–501.
Article78. Christensen B, Gibson PR, Micic D, et al. Safety and efficacy of combination treatment with calcineurin inhibitors and vedolizumab in patients with refractory inflammatory bowel disease. Clin Gastroenterol Hepatol. 2019; 17:486–493.
Article79. Graziano F, Macaluso FS, Cassata N, Citrano M, Orlando A. Rescue therapy with intensive vedolizumab optimization in a seventeen-year-old girl with acute severe ulcerative colitis. Dig Dis Sci. 2021; 66:2470–2471.
Article80. Hamel B, Wu M, Hamel EO, Bass DM, Park KT. Outcome of tacrolimus and vedolizumab after corticosteroid and antiTNF failure in paediatric severe colitis. BMJ Open Gastroenterol. 2018; 5:e000195.
Article81. Resál T, Pigniczki D, Szántó K, Rutka M, Farkas K, Molnar T. Letter: ciclosporin and vedolizumab for steroid-refractory ulcerative colitis. Aliment Pharmacol Ther. 2020; 52:578–579.82. Szántó K, Molnár T, Farkas K. New promising combo therapy in inflammatory bowel diseases refractory to anti-TNF agents: cyclosporine plus vedolizumab. J Crohns Colitis. 2018; 12:629.
Article83. Tarabar D, El Jurdi K, Traboulsi C, et al. A prospective trial with long term follow-up of patients with severe, steroid-resistant ulcerative colitis who received induction therapy with cyclosporine and were maintained with vedolizumab. Inflamm Bowel Dis. 2022; 28:1549–1554.
Article84. Ashat D, Jain A, Weaver KN, Long MD, Herfarth HH, Barnes EL. An old bridge to the newer biologics: cyclosporine for rescue therapy in acute severe ulcerative colitis. Dig Dis Sci. 2022; 67:5439–5443.85. Veyrard P, Pellet G, Laharie D, Nachury M, Juillerat P, Roblin X. Efficacy of induction therapy with calcineurin inhibitors in combination with ustekinumab for acute severe ulcerative colitis. Clin Gastroenterol Hepatol. 2023; 21:1354–1355.
Article86. Shaffer SR, Traboulsi C, Krugliak Cleveland N, Rubin DT. Combining cyclosporine with ustekinumab in acute severe ulcerative colitis. ACG Case Rep J. 2021; 8:e00604.87. Ganzleben I, Geppert C, Osaba L, et al. Successful cyclosporin and Ustekinumab combination therapy in a patient with severe steroid-refractory ulcerative colitis. Therap Adv Gastroenterol. 2020; 13:1756284820954112.
Article88. Vitali F, Rath T, Klenske E, et al. Long-term outcomes of cyclosporin induction and ustekinumab maintenance combination therapy in patients with steroid-refractory acute severe ulcerative colitis. Therap Adv Gastroenterol. 2023; 17:17562848231218555.
Article89. Sandborn WJ, Su C, Sands BE, et al. Tofacitinib as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2017; 376:1723–1736.
Article90. Danese S, Vermeire S, Zhou W, et al. Upadacitinib as induction and maintenance therapy for moderately to severely active ulcerative colitis: results from three phase 3, multicentre, double-blind, randomised trials. Lancet. 2022; 399:2113–2128.
Article91. Feagan BG, Danese S, Loftus EV Jr, et al. Filgotinib as induction and maintenance therapy for ulcerative colitis (SELECTION): a phase 2b/3 double-blind, randomised, placebo-controlled trial. Lancet. 2021; 397:2372–2384.92. Singh A, Goyal MK, Midha V, et al. Tofacitinib in Acute Severe Ulcerative Colitis (TACOS): a randomized controlled trial. Am J Gastroenterol. 2024; 119:1365–1372.
Article93. Komeda Y, Kono M, Kashida H, et al. Successful initial tofacitinib treatment for acute severe ulcerative colitis with steroid resistance: a case series. Ann Gastroenterol. 2023; 36:97–102.
Article94. Malakar S, Kothalkar S, Shamsul Hoda U, Ghoshal UC. Tofacitinib in steroid-refractory acute severe ulcerative colitis: a retrospective analysis. Cureus. 2023; 15:e45416.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Advances in ulcerative colitis therapy
- A Case of Acute Pancreatitis associated with Ulcerative Colitis
- Comparison of Cell Proliferation between Chronic Ulcerative Colitisand Acute Self-limited Colitis
- Acute Severe Ulcerative Colitis: Optimal Strategies for Drug Therapy
- Efficacy of Infliximab Rescue Therapy in Hospitalized Patients with Steroid-Refractory Ulcerative Colitis: Single Center Experience