Cancer Res Treat.
2024 Oct;56(4):1277-1287. 10.4143/crt.2023.1243.
Development of a Prediction Model for Delirium in Hospitalized Patients with Advanced Cancer
- Affiliations
-
- 1Division of Hematology and Medical Oncology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Center for Palliative Care and Clinical Ethics, Seoul National University Hospital, Seoul, Korea
- 3Palliative Care Center, Yonsei Cancer Center, Yonsei University Health System, Seoul, Korea
- 4Division of Medical Oncology, Yonsei Cancer Center, Yonsei University Health System, Seoul, Korea
- 5Yonsei Graduate School, Yonsei University College of Medicine, Seoul, Korea
- 6Division of Medical Oncology, Department of Internal Medicine, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- KMID: 2560261
- DOI: http://doi.org/10.4143/crt.2023.1243
Abstract
- Purpose
Delirium is a common neurocognitive disorder in patients with advanced cancer and is associated with poor clinical outcomes. As a potentially reversible phenomenon, early recognition of delirium by identifying the risk factors demands attention. We aimed to develop a model to predict the occurrence of delirium in hospitalized patients with advanced cancer.
Materials and Methods
This retrospective study included patients with advanced cancer admitted to the oncology ward of four tertiary cancer centers in Korea for supportive cares and excluded those discharged due to death. The primary endpoint was occurrence of delirium. Sociodemographic characteristics, clinical characteristics, laboratory findings, and concomitant medication were investigated for associating variables. The predictive model developed using multivariate logistic regression was internally validated by bootstrapping.
Results
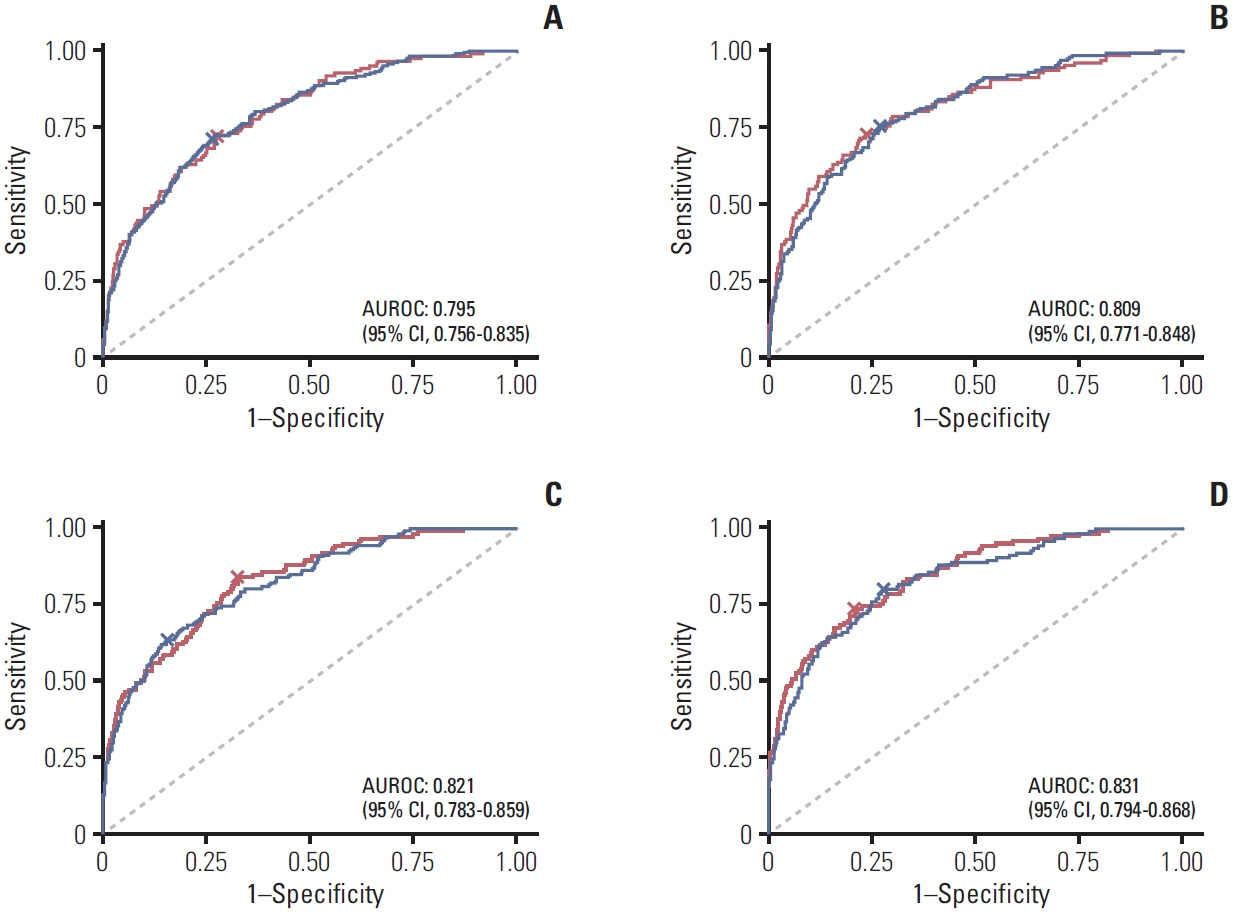
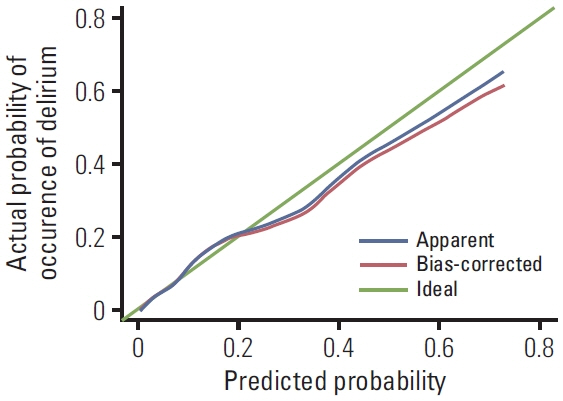
From January 2019 to December 2020, 2,152 patients were enrolled. The median age of patients was 64 years, and 58.4% were male. A total of 127 patients (5.9%) developed delirium during hospitalization. In multivariate logistic regression, age, body mass index, hearing impairment, previous delirium history, length of hospitalization, chemotherapy during hospitalization, blood urea nitrogen and calcium levels, and concomitant antidepressant use were significantly associated with the occurrence of delirium. The predictive model combining all four categorized variables showed the best performance among the developed models (area under the curve 0.831, sensitivity 80.3%, and specificity 72.0%). The calibration plot showed optimal agreement between predicted and actual probabilities through internal validation of the final model.
Conclusion
We proposed a successful predictive model for the risk of delirium in hospitalized patients with advanced cancer.
Keyword
Figure
Reference
-
References
1. Caraceni A, Simonetti F. Palliating delirium in patients with cancer. Lancet Oncol. 2009; 10:164–72.
Article2. Sands MB, Wee I, Agar M, Vardy JL. The detection of delirium in admitted oncology patients: a scoping review. Eur Geriatr Med. 2022; 13:33–51.
Article3. Watt CL, Momoli F, Ansari MT, Sikora L, Bush SH, Hosie A, et al. The incidence and prevalence of delirium across palliative care settings: a systematic review. Palliat Med. 2019; 33:865–77.
Article4. Mercadante S, Adile C, Ferrera P, Cortegiani A, Casuccio A. Symptom expression in patients with advanced cancer admitted to an acute supportive/palliative care unit with and without delirium. Oncologist. 2019; 24:e358–64.
Article5. Mah K, Rodin RA, Chan VW, Stevens BJ, Zimmermann C, Gagliese L. Health-care workers’ hudgments about pain in older palliative care patients with and without delirium. Am J Hosp Palliat Care. 2017; 34:958–65.
Article6. Seiler A, Blum D, Deuel JW, Hertler C, Schettle M, Zipser CM, et al. Delirium is associated with an increased morbidity and in-hospital mortality in cancer patients: results from a prospective cohort study. Palliat Support Care. 2021; 19:294–303.
Article7. Featherstone I, Sheldon T, Johnson M, Woodhouse R, Boland JW, Hosie A, et al. Risk factors for delirium in adult patients receiving specialist palliative care: a systematic review and meta-analysis. Palliat Med. 2022; 36:254–67.
Article8. Lawlor PG, Davis DH, Ansari M, Hosie A, Kanji S, Momoli F, et al. An analytical framework for delirium research in palliative care settings: integrated epidemiologic, clinician-researcher, and knowledge user perspectives. J Pain Symptom Manage. 2014; 48:159–75.
Article9. Bush SH, Lawlor PG, Ryan K, Centeno C, Lucchesi M, Kanji S, et al. Delirium in adult cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2018; 29:iv143–65.
Article10. Seiler A, Schubert M, Hertler C, Schettle M, Blum D, Guckenberger M, et al. Predisposing and precipitating risk factors for delirium in palliative care patients. Palliat Support Care. 2020; 18:437–46.
Article11. Hamano J, Mori M, Ozawa T, Sasaki J, Kawahara M, Nakamura A, et al. Comparison of the prevalence and associated factors of hyperactive delirium in advanced cancer patients between inpatient palliative care and palliative home care. Cancer Med. 2021; 10:1166–79.
Article12. Mercadante S, Adile C, Ferrera P, Cortegiani A, Casuccio A. Delirium assessed by Memorial Delirium Assessment Scale in advanced cancer patients admitted to an acute palliative/supportive care unit. Curr Med Res Opin. 2017; 33:1303–8.
Article13. Nam BH, D’Agostino RB. Discrimination index, the area under the ROC curve. In : Huber-Carol C, Balakrishnan N, Nikulin MS, Mesbah M, editors. Goodness-of-fit tests and model validity. Boston, MA: Birkhäuser Boston;2002. p. 267–79.14. Mercadante S, Masedu F, Balzani I, De Giovanni D, Montanari L, Pittureri C, et al. Prevalence of delirium in advanced cancer patients in home care and hospice and outcomes after 1 week of palliative care. Support Care Cancer. 2018; 26:913–9.
Article15. Gaudreau JD, Gagnon P, Harel F, Roy MA, Tremblay A. Psychoactive medications and risk of delirium in hospitalized cancer patients. J Clin Oncol. 2005; 23:6712–8.
Article16. Balasubramanian P, Kiss T, Tarantini S, Nyul-Toth A, Ahire C, Yabluchanskiy A, et al. Obesity-induced cognitive impairment in older adults: a microvascular perspective. Am J Physiol Heart Circ Physiol. 2021; 320:H740–61.
Article17. Feinkohl I, Winterer G, Pischon T. Obesity and post-operative cognitive dysfunction: a systematic review and meta-analysis. Diabetes Metab Res Rev. 2016; 32:643–51.
Article18. Hung KC, Chiu CC, Hsu CW, Ho CN, Ko CC, Chen IW, et al. Association of preoperative prognostic nutritional index with risk of postoperative delirium: a systematic review and meta-analysis. Front Med (Lausanne). 2022; 9:1017000.
Article19. Nakatani S, Ida M, Wang X, Naito Y, Kawaguchi M. Incidence and factors associated with postoperative delirium in patients undergoing transurethral resection of bladder tumor. JA Clin Rep. 2022; 8:6.
Article20. Wang ML, Kuo YT, Kuo LC, Liang HP, Cheng YW, Yeh YC, et al. Early prediction of delirium upon intensive care unit admission: model development, validation, and deployment. J Clin Anesth. 2023; 88:111121.
Article21. Ko Y, Kim HE, Park JY, Kim JJ, Cho J, Oh J. Relationship between body mass index and risk of delirium in an intensive care unit. Arch Gerontol Geriatr. 2023; 108:104921.
Article22. Lee DH, Giovannucci EL. The obesity paradox in cancer: epidemiologic insights and perspectives. Curr Nutr Rep. 2019; 8:175–81.
Article23. Park Y, Peterson LL, Colditz GA. The plausibility of obesity paradox in cancer-point. Cancer Res. 2018; 78:1898–903.
Article24. Stevens LE, de Moore GM, Simpson JM. Delirium in hospital: does it increase length of stay? Aust N Z J Psychiatry. 1998; 32:805–8.
Article25. Inouye SK, Viscoli CM, Horwitz RI, Hurst LD, Tinetti ME. A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Intern Med. 1993; 119:474–81.
Article26. Matsuoka H, Yoshiuchi K, Koyama A, Otsuka M, Nakagawa K. Chemotherapeutic drugs that penetrate the blood-brain barrier affect the development of hyperactive delirium in cancer patients. Palliat Support Care. 2015; 13:859–64.
Article27. Matsuo N, Morita T, Matsuda Y, Okamoto K, Matsumoto Y, Kaneishi K, et al. Predictors of delirium in corticosteroid-treated patients with advanced cancer: an exploratory, multicenter, prospective, observational study. J Palliat Med. 2017; 20:352–9.
Article28. Gaudreau JD, Gagnon P. Psychotogenic drugs and delirium pathogenesis: the central role of the thalamus. Med Hypotheses. 2005; 64:471–5.
Article29. Litaker D, Locala J, Franco K, Bronson DL, Tannous Z. Preoperative risk factors for postoperative delirium. Gen Hosp Psychiatry. 2001; 23:84–9.
Article30. Marcantonio ER, Juarez G, Goldman L, Mangione CM, Ludwig LE, Lind L, et al. The relationship of postoperative delirium with psychoactive medications. JAMA. 1994; 272:1518–22.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and Validation of a Prediction Model: Application to Digestive Cancer Research
- Delirium in Frail Older Adults
- Delirium Screening, Delirium Knowledge, and Delirium Care among Hospital Nurses at a Tertiary Hospital based on Postoperative Delirium Cases
- Diagnosis and Evaluation for the Early Detection of Delirium
- Clinical Approach to Delirium in Elderly Patients