J Korean Acad Oral Health.
2024 Sep;48(3):124-132. 10.11149/jkaoh.2024.48.3.124.
Relationship between depression and stress and oral-health behavior among Koreans before and during the COVID-19 pandemic
- Affiliations
-
- 1Department of Dental Hygiene, Daegu Health College, Daegu, Korea
- KMID: 2559882
- DOI: http://doi.org/10.11149/jkaoh.2024.48.3.124
Abstract
Objectives
This study aimed to analyze the relationship between depression and stress and oralhealth behavior among Koreans before and during the coronavirus disease 2019 pandemic to provide basic data for systematically managing oral health in future infectious disasters and for developing mental-health policies based on oral health.
Methods
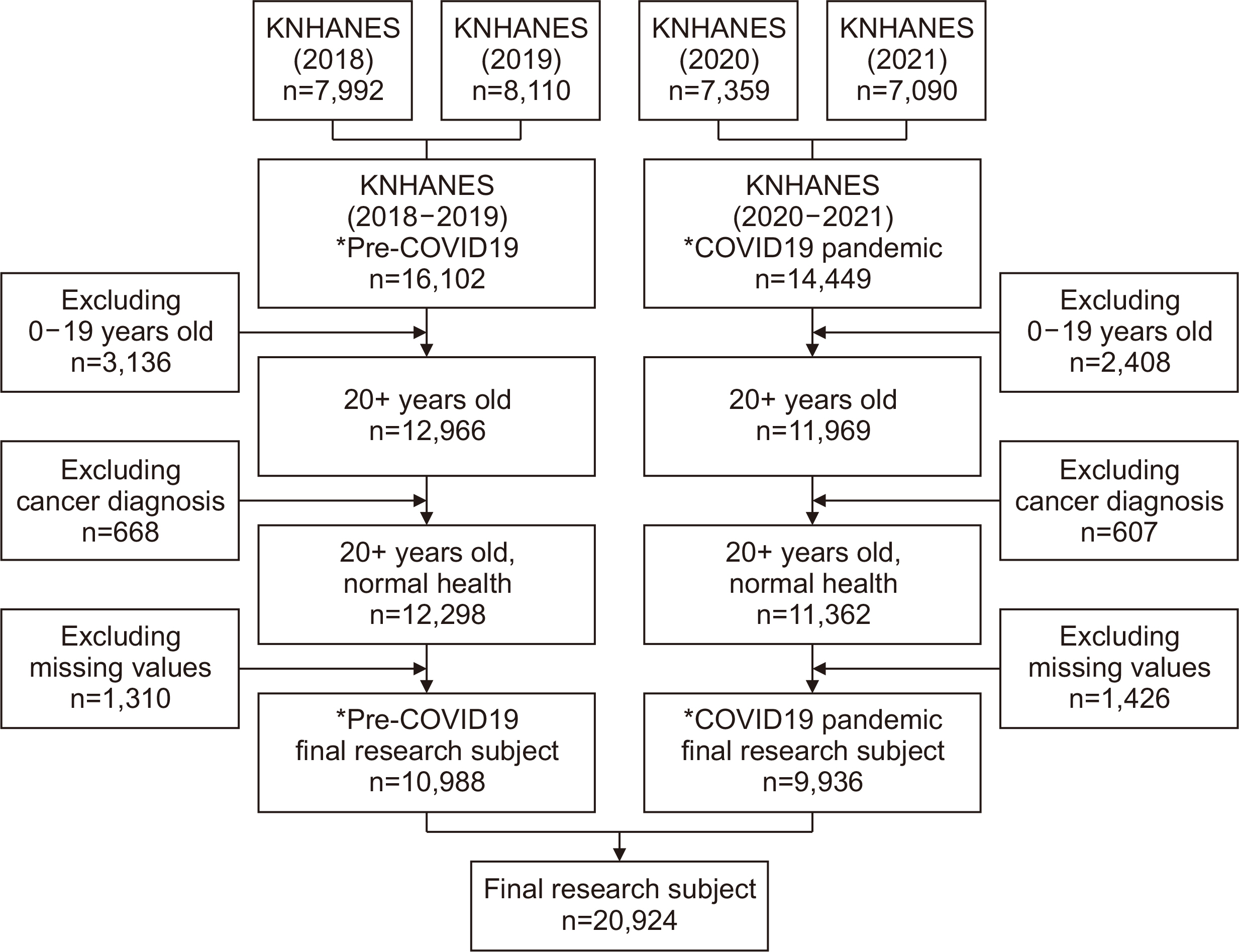
We used raw national health and nutrition research data for the years 2018-2021. The years 2018 and 2019 were classified as ‘the pre-pandemic period’ and 2020 and 2021 were classified as ‘the pandemic period.’ The pre-pandemic and pandemic groups included 16,102 and 14,449 individuals, respectively. We excluded individuals aged <20 years, patients with cancer which could affect the research results, and individuals with missing data. Finally, 20,924 individuals were included in the study, of which, 10,988 and 9,936 were classified into the pre-pandemic and pandemic groups, respectively.
Results
Oral-health behavior in patients with depression was significantly different between the pre-pandemic and pandemic periods. The proportion of participants with ideal oral-health behavior was significantly higher among individuals without depression than among those with depression. In the pre-pandemic and pandemic groups, the odds ratios for practicing ideal oral-health behavior among individuals with low stress perception were 1.182 (P=.002) and 1.148 (P=.010), respectively.
Conclusions
In preparation for a future pandemic, identifying and supporting individuals with high levels of depression or stress is necessary to establish guidelines for regular mental-health checkups in the dental-care environment. Additionally, integrative standard policies must be framed considering the complex interactions between mental health and stress and oral-health behavior.
Keyword
Figure
Reference
-
References
1. Murray J. L., Lopez A. D.. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. World Health Organization;1996. p. 41. https://iris.who.int/handle/10665/41864.2. James S. L., Abate D., Abate K. H., Abay S. M., Abbafati C., Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global eurden of disease study 2017. The Lancet. 2018; 392:789–1858. DOI: 10.1016/S0140-6736(18)32279-7.3. Korea Disease Control and Prevention Agency. 2020. Major results of the 2019 Community health survey. KDCA;from kdca.go.kr/board/board.es?mid=a20602010000&bid=0034&act=view&list_no=367616.4. Organisation for Economic Co-operation and Development. Tackling the Mental Health Impact of the COVID-19 Crisis: An Integrated, Whole of-Society Response. 2021. OECD Publishing.5. Lee DH, Kim YJ, Lee DH, Hwang HH, Nam SK, Kim JY. 2020; The influence of public fear, and psycho-social experiences during the coronavirus disease 2019 (COVID19) pandemic on depression and anxiety in South Korea. Korean J. Counsel. 32:2119–2156. https://doi.org/10.23844/kjcp.2020.11.32.4.2119. DOI: 10.23844/kjcp.2020.11.32.4.2119.6. KDCA. KDCA, Korea Community Health at a Glance 2023: Korea Community Health Survey (Brief version). 2023. https://chs.kdca.go.kr/chs/stats/statsMain.do.7. Korea Health Statistics 2022: Korea National Health and Nutrition Examination Survey (KNHANES Ⅸ-1). http://knhanes.kdca.go.kr/.8. Bambra C, Albani V, Franklin P. 2021; COVID-19 and the gender health paradox. Scand J Public Health. 49:17–26. https://doi.org/10.1177/1403494820975604). DOI: 10.1177/1403494820975604. PMID: 33308006. PMCID: PMC7859577.9. Brown T. A., Chorpita B. F., Korotitsch W., Barlow D. H.. 1997; Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behav. Res. Ther. 35:79–89. DOI: 10.1016/S0005-7967(96)00068-X. PMID: 9009048.10. Kim HM, Jeon YH, Hong JP. 1997; The effect of salivary gland of streptozotocin induced diabetic rats by stress. KJOM. 1:65–80.11. Kim YJ, Park SY, Oh KW. Changes in health behavior and chronic diseases after the COVID-19 pandemic (Report No. 11-1790387-000384-01). Cheongju: Korea Disease Control and Prevention Agency;2021.12. Solomou I., Constantinidou F. 2020; Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: Age and sex matter. Int. J. Environ. Res. Public Health. 17:4924. https://doi.org/10.3390/ijerph17144924. DOI: 10.3390/ijerph17144924. PMID: 32650522. PMCID: PMC7400373.13. Kang MC, Cho HJ, Lee JS. 2013; A latent profile analysis of depression, anxiety, shame, and suicidal ideation. Korean J. Counsel. 25:873–896.14. Jain M., Mathur A., Sawla L., Choudhary G., Kabra K., Duraiswamy P., et al. 2009; Oral health status of mentally disabled subjects in India. J Oral Sci. 51:333–340. DOI: 10.2334/josnusd.51.333. DOI: 10.2334/josnusd.51.333. PMID: 19776499.15. Lee HJ, Kim YS. Relationship between oral health status and depressive symptoms in middle-aged women: the sixth korea national health and nutrition examination survey. JKSDH. 22019;19:941–950.16. Won YS, Kim JH. 2015; The relationship between psychological health and self-rated oral health on convergence study. J Digit Converg. 13:239–48. https://doi.org/10.14400/JDC.2015.13.7.239. DOI: 10.14400/JDC.2015.13.7.239.17. Oh JG, Kim YJ, Go HS. 2001; A study on the clinical characteristics of patients with dry mouth. J Oral Med Pain. 26:331–43.18. Heo SE, Kim YR. 2021; Fusion correlation between the degree of depression and oral health behavior, autologous oral health symptoms, and quality of life due to COVID-19. KCS. 1:27–34.19. Brennan D, Spencer A, Roberts-Thomson K. 2019; Socioeconomic and psychosocial associations with oral health impact and general health. Community Dent. Oral Epidemiol. 47:32–39. http://dx.doi.org/10.1111/cdoe.12419. DOI: 10.1111/cdoe.12419. PMID: 30256446.20. The relationship between distress and oral health management and awareness of generation Y amid the COVID-19 pandemic. 2021; KJ-HSM. 15:35–49. https://doi.org/10.12811/kshsm.2021.15.3.035. DOI: 10.12811/kshsm.2021.15.3.035.21. Lee EJ, Kim SJ. 2023; Prevalence and related factors of depression before and during the COVID-19 pandemic: Findings from the Korea national health and nutrition examination survey. J Korean Med Sci. 38:e74. https://doi.org/10.3346/jkms.2023.38.e74. DOI: 10.3346/jkms.2023.38.e74. PMID: 36918028. PMCID: PMC10010913.22. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. 2020; Prevalence of depression symptoms in us adults before and during the Covid-19 Pandemic. JAMA Netw Open. 3:e2019686. DOI: 10.1001/jamanetworkopen.2020.19686. PMID: 32876685. PMCID: PMC7489837.23. Kim JH, Won YS. 2016; A study on depressive symptoms and periodontal diseases. J Korean Acad Oral Health. 40:250–254. https://doi.org/10.11149/jkaoh.2016.40.4.250. DOI: 10.11149/jkaoh.2016.40.4.250.24. COVID-19 Mental Disorders Collaborators. 2021; Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 398:1700–1712. DOI: 10.1016/S0140-6736(21)02143-7. PMID: 34634250. PMCID: PMC8500697.25. Shin SH, Kim SS, Hong JI. 2018; Pandemic influenza preparedness and response plan. PHWR KCDC. 11:1163–1166.26. Cao R., Lai J., Fu X., Qiu P., Chen J., Liu W. Association between psychological stress, anxiety and oral health status among college students during the Omicron wave: a cross-sectional study. BMC Oral Health. 2023; (23):470. https://doi.org/10.1186/s12903-023-03151-3. DOI: 10.1186/s12903-023-03151-3. PMID: 37424009. PMCID: PMC10332074.27. Stanton R., To G.Q., Khalesi S., Williams S.L., Alley S.J., Thwaite T.L., et al. 2020; Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health. 17:4065. doi: 10.3390/ijerph17114065. DOI: 10.3390/ijerph17114065. PMID: 32517294. PMCID: PMC7312903.28. Heo SE, Kim YR. 2021; Fusion correlation between the degree of depression and oral health behavior, autologous oral health symptoms, and quality of life due to COVID-19. JKCS. 12:27–34. https://doi.org/10.15207/JKCS.2021.12.3.027.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The relationship between stress and oral health-related quality of life in public officials during the COVID-19 pandemic
- The impact of the COVID-19 pandemic on oral health behavior and oral symptoms in young adults
- The Mediating Effects of Health Concern and Depression in the Relation between Self-quarantined People’s COVID-19 Stress and Fatigue
- Factors Influencing Changes in Parenting Behavior during Coronavirus Disease 2019 Pandemic
- How the COVID-19 Pandemic Affects the Mental Health of University Hospital Nurses?: Focusing on Resilience, Stress, Depression, Anxiety, and Sleep