Ann Clin Microbiol.
2024 Sep;27(3):185-196. 10.5145/ACM.2024.27.3.6.
Seasonality and epidemiological trends in species distribution and antifungal susceptibility of Candida species isolated from various clinical specimens conducted during 2011–2022, Korea: a retrospective surveillance study
- Affiliations
-
- 1Department of Laboratory Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- KMID: 2559809
- DOI: http://doi.org/10.5145/ACM.2024.27.3.6
Abstract
- Background
As most Candida species cause opportunistic infections, it is helpful for patient care to determine species name of Candida spp. and their distribution in both sterile and non-sterile specimens. We aimed to investigate trends in the distribution of Candida species isolated from a hospital in Korea, along with their antifungal susceptibilities and seasonal variations.
Methods
This study was conducted at the Chung-Ang University Hospital and included 8,760 different clinical specimens from March 2011 to December 2022. Identification of the fungal species and its antifungal susceptibility testing were performed using VITEK 2 ID-YST system for six drugs: amphotericin B, caspofungin, fluconazole, voriconazole, micafungin, and flucytosine.
Results
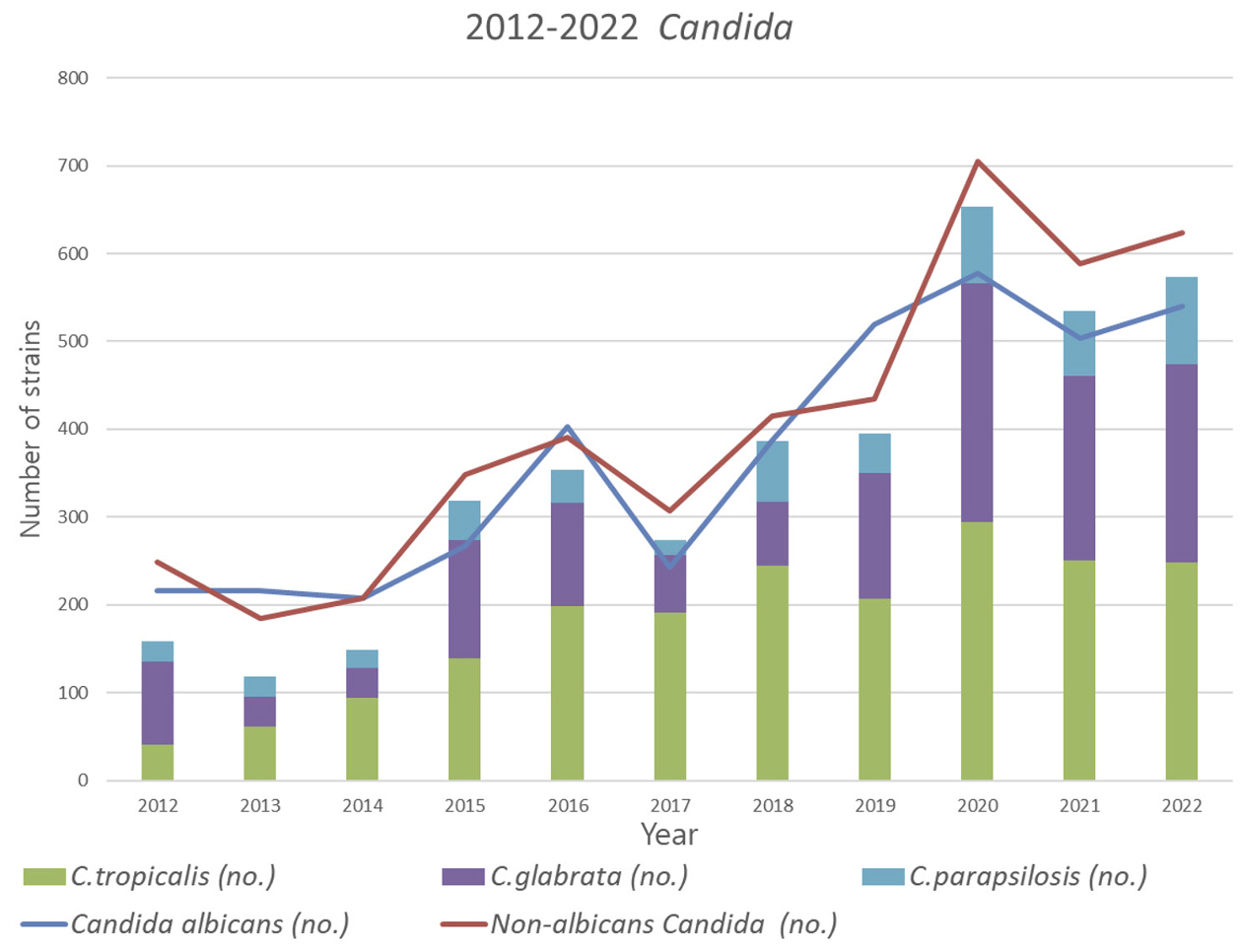
The most common fungal species was Candida albicans. The C. albicans positivity rate gradually increased from 2012 to 2022. Since 2020, however, this trend reversed and the non-albicans Candida (NAC) superseded the count of C. albicans. Among the NAC, C. glabrata showed significant increase. When a weekly analysis was performed, C. glabrata was evenly distributed without any noticeable peak; however, the positive rate decreased from late December to early January across all years.
Conclusion
Monitoring of future trends should necessarily be continued. Our findings revealed that the positive rate for Candida was the lowest in the months of December and January of the studied years, which can be attributed to environmental factors. However, further research needs to be conducted.
Keyword
Figure
Reference
-
1. Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 2022;399:629-55.2. World Health Organization. Global antimicrobial resistance surveillance system (GLASS): technical meeting on the early implementation phase. 22-23 October 2015 WHO Regional Office for Europe Copenhagen, Denmark. Meeting Report. Geneva: WHO Press; 2016 Oct. Report No.: WHO/OHE/PED/AMR/2016.1.3. World Health Organization. GLASS early implementation protocol for inclusion of Candida spp. https://www.who.int/publications/i/item/WHO-WSI-AMR-2019.4 [Online] (last visited on 11 January 2024).4. Lee H, Yoon EJ, Kim D, Jeong SH, Shin JH, Shin JH, et al. Establishment of the South Korean national antimicrobial resistance surveillance system, Kor-GLASS, in 2016. Euro Surveill 2018;23:1700734.5. Korea Disease Control and Prevention Agency. National Antimicrobial Resistance Surveillance in Korea, 2021. https://www.korea.kr/docViewer/skin/doc.html?fn=197089655&rs=/ docViewer/result/2022.11/17/197089655 [Online] (last visited on 11 January 2024).6. Won EJ, Choi MJ, Jeong SH, Kim D, Shin KS, Shin JH, et al. Nationwide surveillance of antifungal resistance of Candida bloodstream isolates in South Korean hospitals: two year report from Kor-GLASS. J Fungi 2022;8:996.7. Won EJ, Shin JH, Choi MJ, Lee WG, Park YJ, Uh Y, et al. Antifungal susceptibilities of bloodstream isolates of Candida species from nine hospitals in Korea: application of new antifungal breakpoints and relationship to antifungal usage. PLoS One 2015;10:e0118770.8. Won EJ, Shin JH, Lee WK, Koo SH, Kim SY, Park YJ, et al. Distribution of yeast and mold species isolated from clinical specimens at 12 hospitals in Korea during 2011. Ann Clin Microbiol 2013;16:92-100.9. Rex JH, Pfaller MA, Walsh TJ, Chaturvedi V, Espinel-Ingroff A, Ghannoum MA, et al. Antifungal susceptibility testing: practical aspects and current challenges. Clin Microbiol Rev 2001;14:643-58.10. Chae MJ, Shin JH, Cho D, Kee SJ, Kim SH, Shin MG, et al. Antifungal susceptibilities and distribution of Candida species recovered from blood cultures over an 8-year period. Korean J Lab Med 2003;329-35.11. Shin JH, Kim HR, Lee JN. Distribution and antifungal susceptibility of Candida species isolated from clinical specimens during the past six years. Korean J Clin Microbiol 2004;16470.12. Lee MK, Yong D, Kim M, Kim MN, Lee K. Species distribution and antifungal susceptibilities of yeast clinical isolates from three hospitals in Korea, 2001 to 2007. Korean J Lab Med 2010;30:364-72.13. Grassly NC and Fraser C. Seasonal infectious disease epidemiology. Proc Biol Sci 2006;273:2541-50.14. Edi-Osagie NE and Emmerson AJ. Seasonality of invasive Candida infection in neonates. Acta Paediatr 2005;94:72-4.15. Donders GGG, Ruban K, Donders F, Reybrouck R. Lab-based retrospective 10-year analysis shows seasonal variation of vaginal Candida infection rates in Belgium. J Clin Med 2022;11:574.16. Kim TH, Lee JY, Chung JD, Lee SH, Lee MK. Species distribution and antifungal susceptibilities of yeast isolated from catheterized urine specimen. Korean J Urogenit Tract Infect Inflamm 2011;6:73-9.17. Pfaller MA, Diekema DJ, Procop GW, Rinaldi MG. Multicenter comparison of the VITEK 2 antifungal susceptibility test with the CLSI broth microdilution reference method for testing amphotericin B, flucytosine, and voriconazole against Candida spp. J Clin Microbiol 2007;45:3522-8.18. Pfaller MA, Diekema DJ, Procop GW, Rinaldi MG. Multicenter comparison of the VITEK 2 yeast susceptibility test with the CLSI broth microdilution reference method for testing f luconazole against Candida spp. J Clin Microbiol 2007;45:796-802.19. Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 2004; 39:309-17.20. Antinori S, Milazzo L, Sollima S, Galli M, Corbellino M. Candidemia and invasive candidiasis in adults: a narrative review. Eur J Intern Med 2016;34:21-8.21. Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 2016;62:e1-50.22. Hwang YY, Kang OK, Park CE, Hong SN, Kim YK, Huh HJ, et al. Frequency of Candida strains isolated from candidiasis patients at a tertiary hospital over the last 10 years. Korean J Clin Lab Sci 2022;54:110-8.23. Tan TY, Hsu LY, Alejandria MM, Chaiwarith R, Chinniah T, Chayakulkeeree M, et al. Antifungal susceptibility of invasive Candida bloodstream isolates from the Asia-Pacific region. Med Mycol 2016;54:471-7.24. Astvad KMT, Johansen HK, Roder BL, Rosenvinge FS, Knudsen JD, Lemming L, et al. Update from a 12-year nationwide fungemia surveillance: increasing intrinsic and acquired resistance causes concern. J Clin Microbiol 2018;56:e01564-17.25. Ko JH, Jung DS, Lee JY, Kim HA, Ryu SY, Jung SI, et al. Changing epidemiology of non-albicans candidemia in Korea. J Infect Chemother 2019;25:388-91.26. Kim TH, Kweon OJ, Kim HR, Lee MK. Identification of uncommon Candida species using commercial identification systems. J Microbiol Biotechnol 2016;26:2206-13.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Distribution and Antifungal Susceptibility of Candida species Isolated from Clinical Specimens during the Past Six Years
- Antifungal Drug Susceptibility
- Changes in Candidemia during the COVID-19 Pandemic: Species Distribution, Antifungal Susceptibility, Initial Antifungal Usage, and Mortality Trends in Two Korean Tertiary Care Hospitals
- Candiduria: Analysis of Changing Trends and Antifungal Dynamics in Acute Healthcare Settings with Special Reference to Rare Candida Species
- Antifungal Susceptibility Testing with Etest for Candida Species Isolated from Patients with Oral Candidiasis