Clin Transplant Res.
2024 Sep;38(3):203-211. 10.4285/ctr.24.0033.
Experience from 100 consecutive pancreas transplants amidst low national transplant activity: a retrospective study at a single center in Korea
- Affiliations
-
- 1Division of Hepato-Biliary-Pancreatic Surgery and Transplantation, Department of Surgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 3Department of Vascular Surgery, Innlandet Hospital Trust, Brumunddal, Norway
- 4Pusan National University School of Medicine, Yangsan, Korea
- KMID: 2559808
- DOI: http://doi.org/10.4285/ctr.24.0033
Abstract
- Background
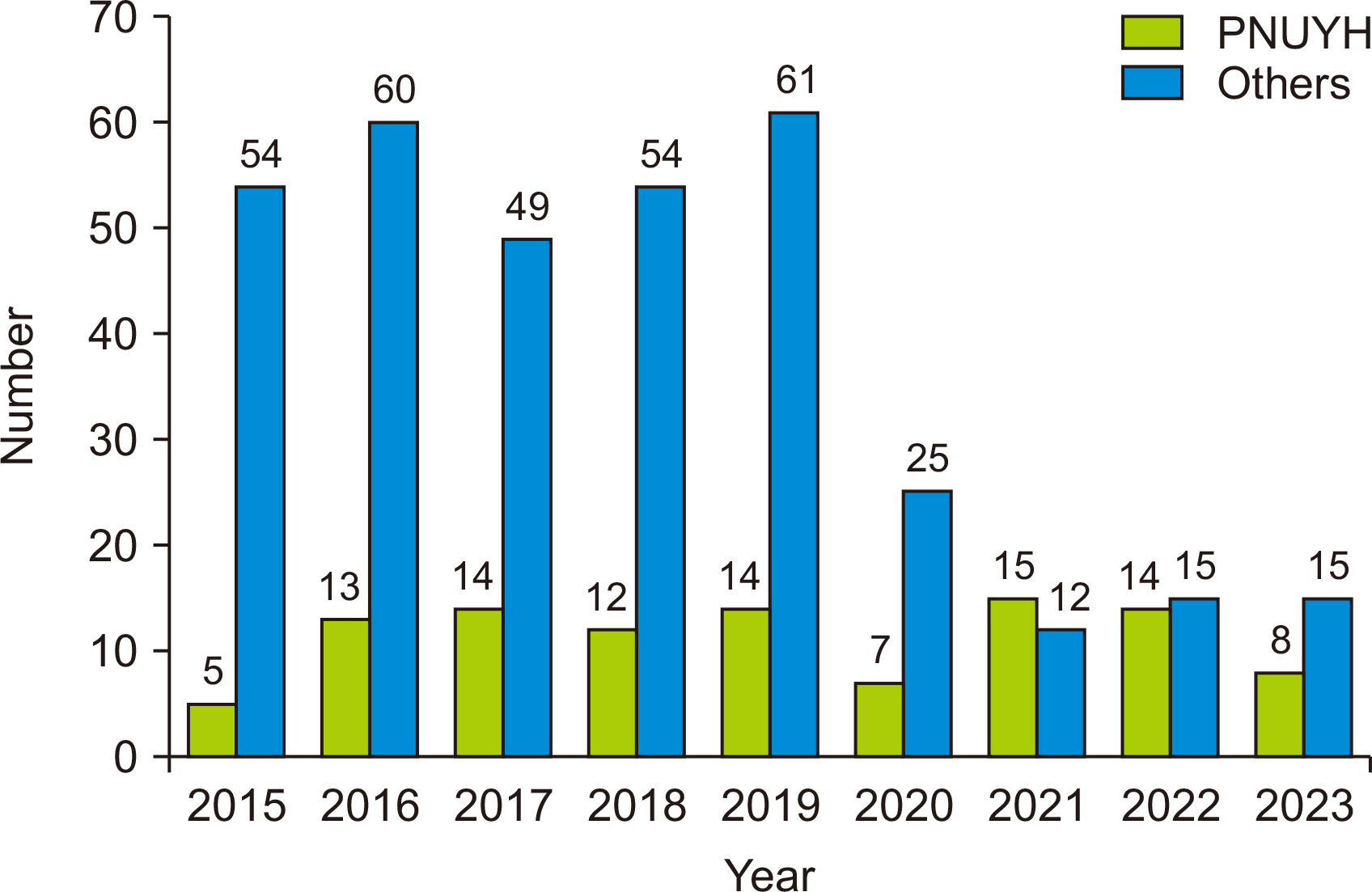
Since 1992, over 800 pancreas transplants have been performed in Korea. However, this number is significantly lower compared to the number of kidney or liver transplants.
Methods
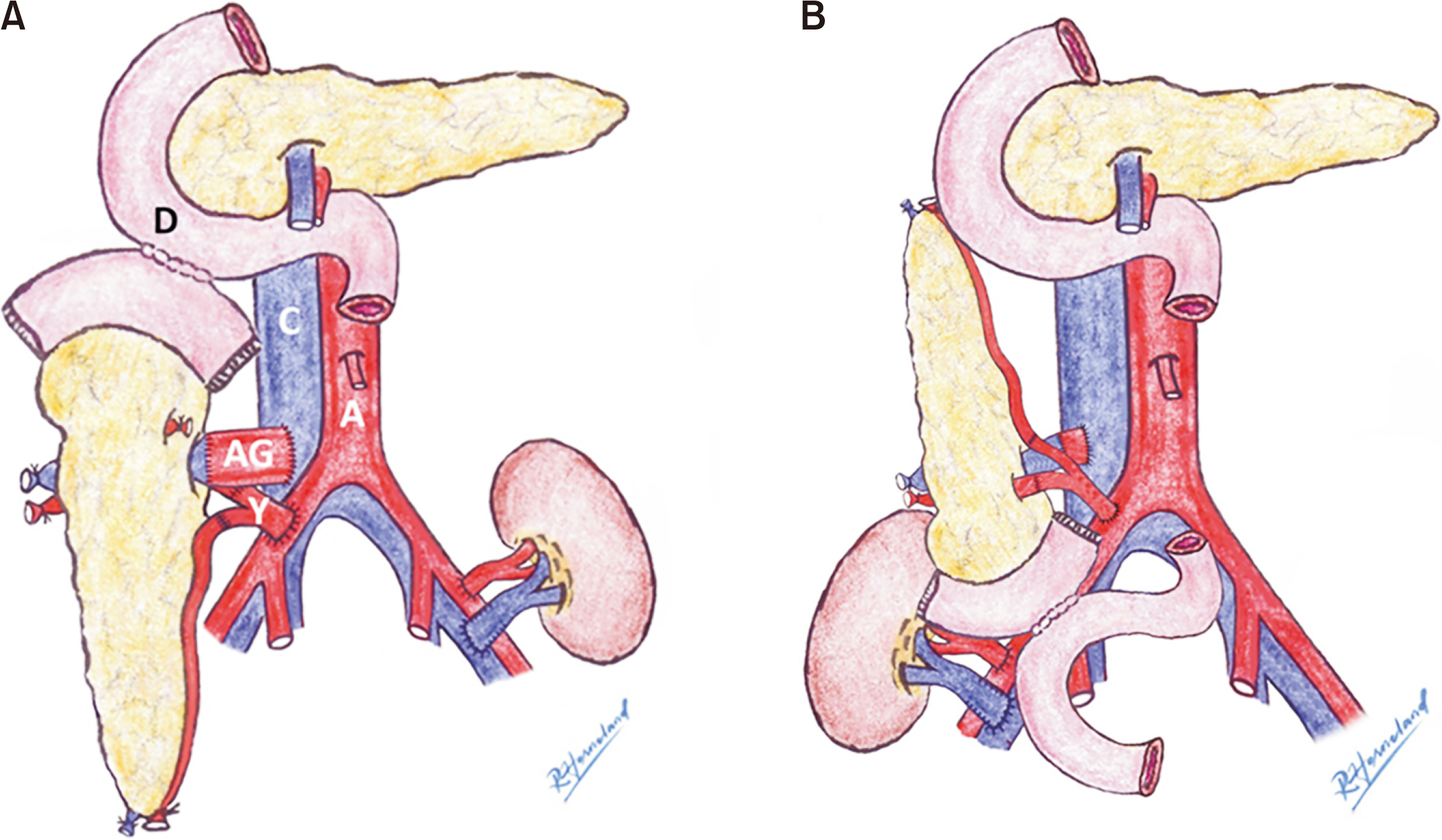
Between 2015 and July 2023, Pusan National University Yangsan Hospital conducted 100 pancreas transplants, accounting for about 20% of all transplants performed in Korea during this period. The study comprised 27 simultaneous pancreas and kidney (SPK) transplants, 23 pancreas after kidney (PAK) transplants, and 50 pancreas transplant alone (PTA) cases. Duodenoduodenostomy was the primary surgical technique employed for exocrine drainage, along with various modifications of the venous outflow anastomosis.
Results
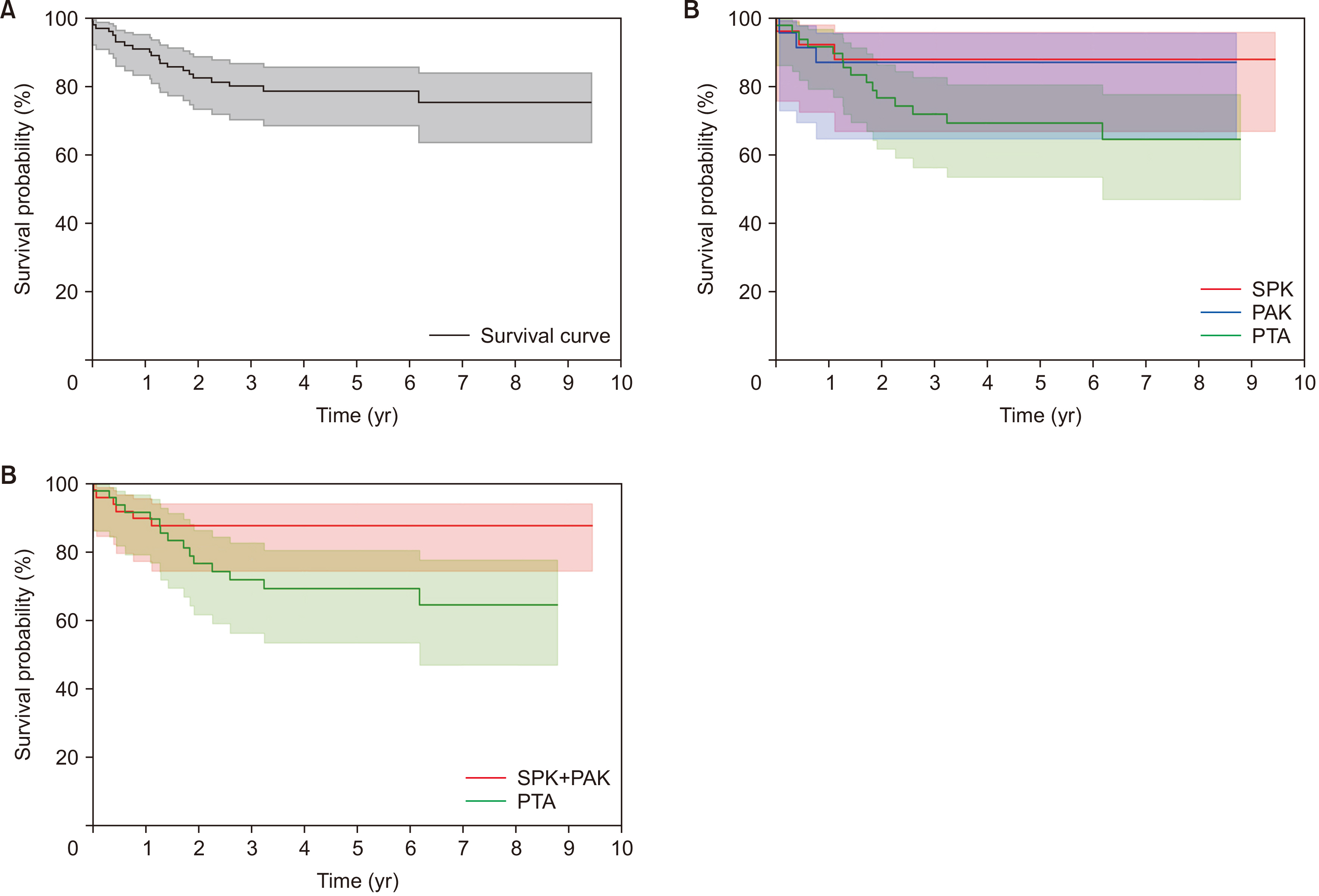
The availability of brain-dead donors for kidney transplants was lower compared to isolated pancreas transplants. Patients undergoing SPK transplants faced significantly longer waiting times than those receiving PTA or PAK transplants. The rate of surgical complications was acceptable, with a notably low thrombotic graft failure rate of 1.0%. In the PTA group, acute rejection of the graft pancreas occurred frequently (18.0%), though this was not statistically significant (P=0.328). The pancreas transplantation survival rates were 91.0%, 78.5%, and 75.4% at 1, 5, and 9 years, respectively. The PTA group exhibited a lower graft survival rate than the SPK and PAK groups, with marginal statistical significance (P=0.059).
Conclusions
Graft survival rates have improved over time due to advancements in surgical techniques and immunosuppressant strategies. By sharing our experiences, we aim to enhance the activity and success of pancreas transplantation in Korea.
Keyword
Figure
Reference
-
1. KONOS database. Available from: www.KONOS.go.kr.2. Korean Organ Transplantation Registry (KOTRY). 2023. 2022 KOTRY annual data report [Internet]. KOTRY;Available from: https://www.kotryfoundation.org/rang_board/list.html?num=204&code=mem_ref. cited 2024 Jun 15.3. Gruessner AC, Gruessner RW. 2022; The 2022 International Pancreas Transplant Registry report-a review. Transplant Proc. 54:1918–43. DOI: 10.1016/j.transproceed.2022.03.059. PMID: 35970624.4. Dean PG, Kukla A, Stegall MD, Kudva YC. 2017; Pancreas transplantation. BMJ. 357:j1321. DOI: 10.1136/bmj.j1321. PMID: 28373161.5. Redfield RR, Rickels MR, Naji A, Odorico JS. 2016; Pancreas transplantation in the modern era. Gastroenterol Clin North Am. 45:145–66. DOI: 10.1016/j.gtc.2015.10.008. PMID: 26895686.6. Fridell JA, Niederhaus S, Curry M, Urban R, Fox A, Odorico J. 2019; The survival advantage of pancreas after kidney transplant. Am J Transplant. 19:823–30. DOI: 10.1111/ajt.15106. PMID: 30188614.7. Niederhaus SV. 2015; Pancreas transplant alone. Curr Opin Organ Transplant. 20:115–20. DOI: 10.1097/MOT.0000000000000157. PMID: 25563998.8. Ryu JH, Ko HJ, Shim JR, Lee TB, Yang KH, Kim T, et al. 2021; Technical factors that minimize the occurrence of early graft failure in pancreas transplantation. Clin Transplant. 35:e14455. DOI: 10.1111/ctr.14455. PMID: 34390276.9. Ryu JH, Lee TB, Park YM, Yang KH, Chu CW, Lee JH, et al. 2017; Pancreas transplant with duodeno-duodenostomy and caval drainage using a diamond patch graft: a single-center experience. Ann Transplant. 22:24–34. DOI: 10.12659/AOT.901469. PMID: 28100901.10. Choi BH, Park YM, Yang KH, Chu CW, Ryu JH. 2016; Inferior vena cava-duodenal drainage in pancreas alone transplantation for chronic pancreatitis: a case report. Transplant Proc. 48:3217–21. DOI: 10.1016/j.transproceed.2016.02.068. PMID: 27932185.11. Ryu JH, Shim JR, Lee TB, Yang KH, Kim T, Kim SR, et al. 2022; Modification of venous outflow to avoid thrombotic graft failure in pancreas transplantation. Ann Transplant. 27:e937514. DOI: 10.12659/AOT.937514. PMID: 36482773. PMCID: PMC9749327.12. Ryu JH, Lee TB, Yang KH, Kim T, Chung YS, Choi B. 2018; Fence angioplasty prevents narrowing of venous anastomosis in solitary pancreas transplant. Ann Transplant. 23:681–90. DOI: 10.12659/AOT.911379. PMID: 30275438. PMCID: PMC6248316.13. Axelrod DA, Sung RS, Meyer KH, Wolfe RA, Kaufman DB. 2010; Systematic evaluation of pancreas allograft quality, outcomes and geographic variation in utilization. Am J Transplant. 10:837–45. DOI: 10.1111/j.1600-6143.2009.02996.x. PMID: 20121753.14. Min SI, Ahn C, Han DJ, Kim SI, Chung SY, Lee SK, et al. 2015; To achieve national self-sufficiency: recent progresses in deceased donation in Korea. Transplantation. 99:765–70. DOI: 10.1097/TP.0000000000000412. PMID: 25226175.15. Korean Network for Organ Sharing (KONOS). 2023. Annual Report of the transplant 2022 [Internet]. KONOS;Available from: http://konos.go.kr. cited 2024 Jun 15.16. Nordheim E, Horneland R, Aandahl EM, Grzyb K, Aabakken L, Paulsen V, et al. 2018; Pancreas transplant rejection episodes are not revealed by biopsies of the donor duodenum in a prospective study with paired biopsies. Am J Transplant. 18:1256–61. DOI: 10.1111/ajt.14658. PMID: 29316221.17. Ryu DG, Kang DH, Choi CW, Choi BH, Kim HW, Park SB, et al. 2022; Endoscopic visualization of graft status in patients with pancreas transplantation. Surg Endosc. 36:4057–66. DOI: 10.1007/s00464-021-08727-0. PMID: 34782963.18. Kandaswamy R, Stock PG, Miller JM, Booker SE, White J, Israni AK, et al. 2024; OPTN/SRTR 2022 annual data report: pancreas. Am J Transplant. 24(2S1):S119–75. DOI: 10.1016/j.ajt.2024.01.013. PMID: 38431358.19. Harbell JW, Morgan T, Feldstein VA, Roll GR, Posselt A, Kang SM, et al. 2017; Splenic vein thrombosis following pancreas transplantation: identification of factors that support conservative management. Am J Transplant. 17:2955–62. DOI: 10.1111/ajt.14428. PMID: 28707821.20. Laftavi MR, Pankewycz O, Kohli R, Feng L, Said M, Sharma R, et al. 2014; Short and long-term outcomes of systemic drainage to IVC: a new technique for pancreas transplantation. Transplant Proc. 46:1900–4. DOI: 10.1016/j.transproceed.2014.06.043. PMID: 25131066.21. Gruessner AC, Sutherland DE, Gruessner RW. 2010; Pancreas transplantation in the United States: a review. Curr Opin Organ Transplant. 15:93–101. DOI: 10.1097/MOT.0b013e32833552d2. PMID: 20009932.22. Parajuli S, Arunachalam A, Swanson KJ, Aziz F, Garg N, Redfield RR, et al. 2019; Outcomes after simultaneous kidney-pancreas versus pancreas after kidney transplantation in the current era. Clin Transplant. 33:e13732. DOI: 10.1111/ctr.13732. PMID: 31628870.23. Ryu JH, Ko HJ, Shim JR, Lee TB, Yang KH, Lee JH, et al. 2020; Eosinophil-to-monocyte ratio is an excellent predictor of acute cellular rejection in pancreas transplant alone recipients. Clin Transplant. 34:e13785. DOI: 10.1111/ctr.13785. PMID: 31957063.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CORRECTION: Experience from 100 consecutive pancreas transplants amidst low national transplant activity: a retrospective study at a single center in Korea
- Pancreas transplantation: a 12-year single-center experience at Siriraj Hospital, Thailand
- Virtual crossmatch versus complement-dependent cytotoxicity crossmatch in deceased kidney paired donations: a single-center experience from India
- Simultaneous pancreas kidney transplant: a tertiary care center experience in India
- The pancreas after kidney transplant is the second-best option, comparable to the simultaneous pancreas and kidney transplant