J Korean Med Sci.
2024 Sep;39(36):e252. 10.3346/jkms.2024.39.e252.
Direct Oral Anticoagulants in Antiphospholipid Syndrome-Associated Venous Thromboembolism: Real World Evidence
- Affiliations
-
- 1Respiratory Division, Department of Internal Medicine, Soonchunhyang University Gumi Hospital, Soonchunhyang University School of Medicine, Gumi, Korea
- 2Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 3Respiratory Division, Department of Internal Medicine, Soonchunhyang University Seoul Hospital, Soonchunhyang University School of Medicine, Seoul, Korea
- 4Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Jeonbuk National University Medical School, Jeonju, Korea
- KMID: 2559774
- DOI: http://doi.org/10.3346/jkms.2024.39.e252
Abstract
- Background
The efficacy and safety of direct oral anticoagulants (DOACs) versus warfarin in patients with antiphospholipid syndrome-associated venous thromboembolism (APS-VTE) remain uncertain. We aimed to evaluate efficacy and safety of DOACs in patients with APSVTE.
Methods
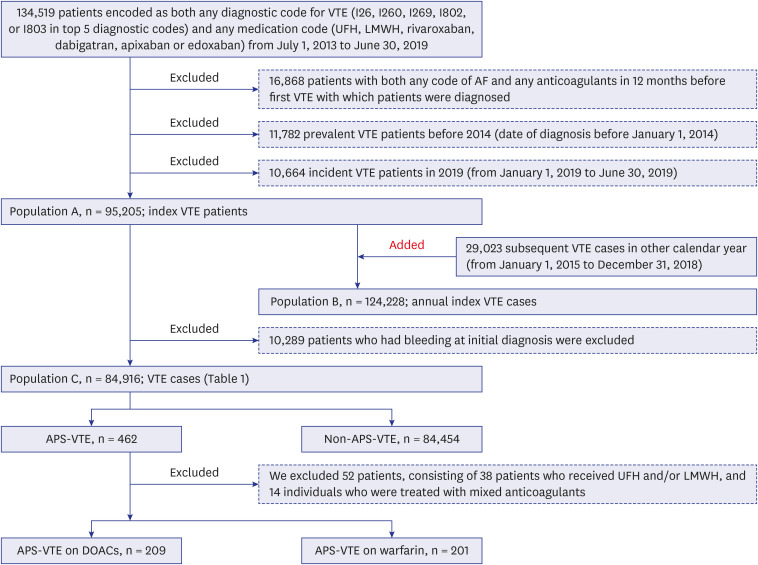
Using the Korean Health Insurance Review and Assessment Service database, we retrospectively identified all APS-VTE cases. We examined the VTE recurrence, arterial thrombosis, death and bleeding in patients who received DOACs compared with warfarin for therapeutic anticoagulation.
Results
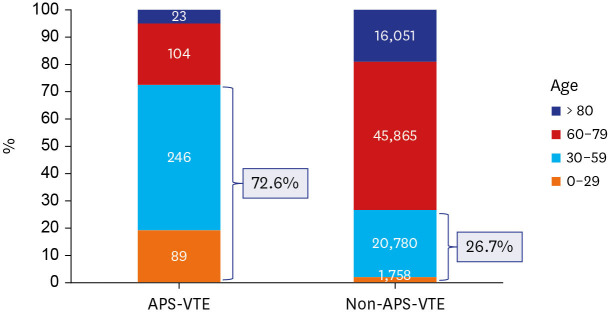
Of all the VTE cases (n = 84,916) detected between 2014 and 2018, patients with APS-VTE (n = 410) accounted for 0.48%. Most patients with APS-VTE (73%) were aged < 60 years. The recurrent VTE occurred in 8 of 209 patients (3.8%) who received DOACs and in 7 of 201 (3.5%) who received warfarin (relative risk [RR], 1.099; 95% confidence interval [CI], 0.41–2.98; P = 1.000). The arterial thrombosis (ATE) occurred in 8 of 209 patients (3.8%) who received DOAC and in 20 of 201 (10%) who received warfarin (RR, 0.385; 95% CI, 0.17–0.85; P = 0.024). The composite outcomes of VTE recurrence, ATE, or mortality were significantly lower in patients (9.1%) on DOAC than in those (16.3%) on warfarin (RR, 0.537; 95% CI, 0.32–0.91; P = 0.028). The bleeding outcome occurred in 7 of 209 (3.4%) patients in the DOACs group and 7 of 201 (3.5%) patients in the warfarin group (RR, 0.96; 95% CI, 0.34–2.69; P = 0.840).
Conclusion
In patients with APS-VTE, DOACs group showed comparable rates of recurrent VTE, bleeding, and deaths, but a significantly lower incidence of ATE and composite outcomes compared with the warfarin group in Korea.
Keyword
Figure
Reference
-
1. Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006; 4(2):295–306. PMID: 16420554.2. Bertin D, Camoin-Jau L, Veit V, Resseguier N, Lambert M, Buffet Delmas P, et al. Single or triple positivity for antiphospholipid antibodies in “carriers” or symptomatic patients: Untangling the knot. J Thromb Haemost. 2021; 19(12):3018–3030. PMID: 34469630.3. Na YS, Jang S, Hong S, Oh YM, Lee SD, Lee JS. Clinical phenotype of a first unprovoked acute pulmonary embolism associated with antiphospholipid antibody syndrome. Tuberc Respir Dis (Seoul). 2019; 82(1):53–61. PMID: 30574689.4. Yelnik CM, Urbanski G, Drumez E, Sobanski V, Maillard H, Lanteri A, et al. Persistent triple antiphospholipid antibody positivity as a strong risk factor of first thrombosis, in a long-term follow-up study of patients without history of thrombosis or obstetrical morbidity. Lupus. 2017; 26(2):163–169. PMID: 27432808.5. Petri M. Epidemiology of the antiphospholipid antibody syndrome. J Autoimmun. 2000; 15(2):145–151. PMID: 10968901.6. Hwang JJ, Shin SH, Kim YJ, Oh YM, Lee SD, Kim YH, et al. Epidemiology of Antiphospholipid Syndrome in Korea: a nationwide population-based study. J Korean Med Sci. 2020; 35(5):e35. PMID: 32030922.7. Zuily S, Cohen H, Isenberg D, Woller SC, Crowther M, Dufrost V, et al. Use of direct oral anticoagulants in patients with thrombotic antiphospholipid syndrome: Guidance from the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2020; 18(9):2126–2137. PMID: 32881337.8. Stevens SM, Woller SC, Baumann Kreuziger L, Bounameaux H, Doerschug K, Geersing GJ, et al. Executive summary: antithrombotic therapy for VTE disease: second update of the CHEST guideline and expert panel report. Chest. 2021; 160(6):2247–2259. PMID: 34352279.9. Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014; 36:e2014008. PMID: 25078381.10. National Health Insurance Service. Utilization of Medical Services by Region in 2014. The 2014 Statistical Yearbook on Utilization of Medical Services by Region. Volume 1. Wonju, Korea: National Health Insurance Service;2015.11. Jang MJ, Bang SM, Oh D. Incidence of venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost. 2011; 9(1):85–91. PMID: 20942850.12. Jang MJ, Bang SM, Oh D. Incidence of pregnancy-associated venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost. 2011; 9(12):2519–2521. PMID: 21951997.13. Hong J, Lee JH, Yhim HY, Choi WI, Bang SM, Lee H, et al. Incidence of venous thromboembolism in Korea from 2009 to 2013. PLoS One. 2018; 13(1):e0191897. PMID: 29370290.14. Hwang HG, Lee JH, Kim SA, Kim YK, Yhim HY, Hong J, et al. Incidence of venous thromboembolism: the 3rd Korean nationwide study. J Korean Med Sci. 2022; 37(17):e130. PMID: 35502501.15. Pengo V, Denas G, Zoppellaro G, Jose SP, Hoxha A, Ruffatti A, et al. Rivaroxaban vs warfarin in high-risk patients with antiphospholipid syndrome. Blood. 2018; 132(13):1365–1371. PMID: 30002145.16. Khairani CD, Bejjani A, Piazza G, Jimenez D, Monreal M, Chatterjee S, et al. Direct oral anticoagulants vs vitamin K antagonists in patients with antiphospholipid syndromes: meta-analysis of randomized trials. J Am Coll Cardiol. 2023; 81(1):16–30. PMID: 36328154.17. Ordi-Ros J, Sáez-Comet L, Pérez-Conesa M, Vidal X, Riera-Mestre A, Castro-Salomó A, et al. Rivaroxaban versus vitamin K antagonist in antiphospholipid syndrome: a randomized noninferiority trial. Ann Intern Med. 2019; 171(10):685–694. PMID: 31610549.18. Cohen H, Hunt BJ, Efthymiou M, Arachchillage DR, Mackie IJ, Clawson S, et al. Rivaroxaban versus warfarin to treat patients with thrombotic antiphospholipid syndrome, with or without systemic lupus erythematosus (RAPS): a randomised, controlled, open-label, phase 2/3, non-inferiority trial. Lancet Haematol. 2016; 3(9):e426–e436. PMID: 27570089.19. Mustonen P, Lehtonen KV, Javela K, Puurunen M. Persistent antiphospholipid antibody (aPL) in asymptomatic carriers as a risk factor for future thrombotic events: a nationwide prospective study. Lupus. 2014; 23(14):1468–1476. PMID: 25164304.20. van Walraven C, Jennings A, Oake N, Fergusson D, Forster AJ. Effect of study setting on anticoagulation control: a systematic review and metaregression. Chest. 2006; 129(5):1155–1166. PMID: 16685005.21. Samsa GP, Matchar DB, Goldstein LB, Bonito AJ, Lux LJ, Witter DM, et al. Quality of anticoagulation management among patients with atrial fibrillation: results of a review of medical records from 2 communities. Arch Intern Med. 2000; 160(7):967–973. PMID: 10761962.22. Levy RA, Signorelli F. Patient-health care provider relationship: how can it impact on APS (Hughes’ syndrome) adherence to treatment? Lupus. 2014; 23(12):1265–1268. PMID: 25228722.23. Hwang HG, Lee JH, Hong J, Kim SA, Kim YK, Kim MS, et al. Recurrence of cancer-associated venous thromboembolism between 2009 and 2013: a nationwide Korean study. Clin Exp Thromb Hemost. 2021; 7(1):14–19.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypercoagulable states: an algorithmic approach to laboratory testing and update on monitoring of direct oral anticoagulants
- A Case of Antiphospholipid Syndrome Associated with Protein C Deficiency
- Direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism
- Inferior Vena Cava Thrombectomy in a Patient with Antiphospholipid Syndrome : A case report
- Current Management of Pulmonary Thromboembolism