J Liver Cancer.
2024 Sep;24(2):263-273. 10.17998/jlc.2024.06.03.
Assessment of real-time US-CT/MR-guided percutaneous gold fiducial marker implementation in malignant hepatic tumors for stereotactic body radiation therapy
- Affiliations
-
- 1Department of Radiology, Inje University Ilsan Paik Hospital, Goyang, Korea
- 2Department of Radiation Oncology, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea
- 3Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea
- 4Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul, Korea
- 5Department of Radiology, Seoul National University Hospital, Seoul, Korea
- KMID: 2559473
- DOI: http://doi.org/10.17998/jlc.2024.06.03
Abstract
- Backgrounds/Aims
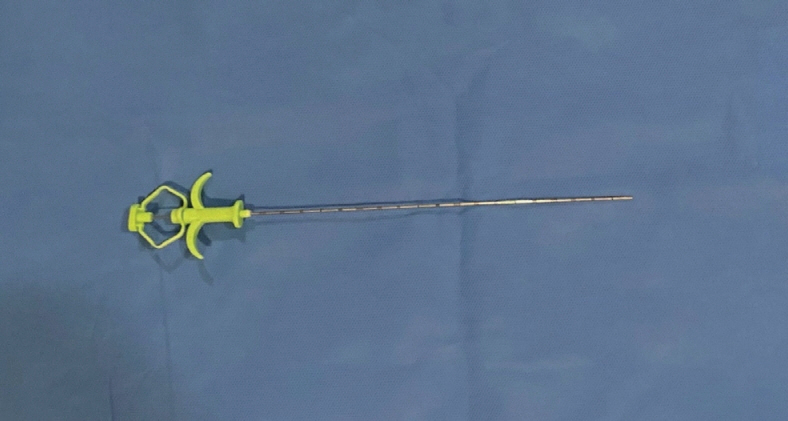
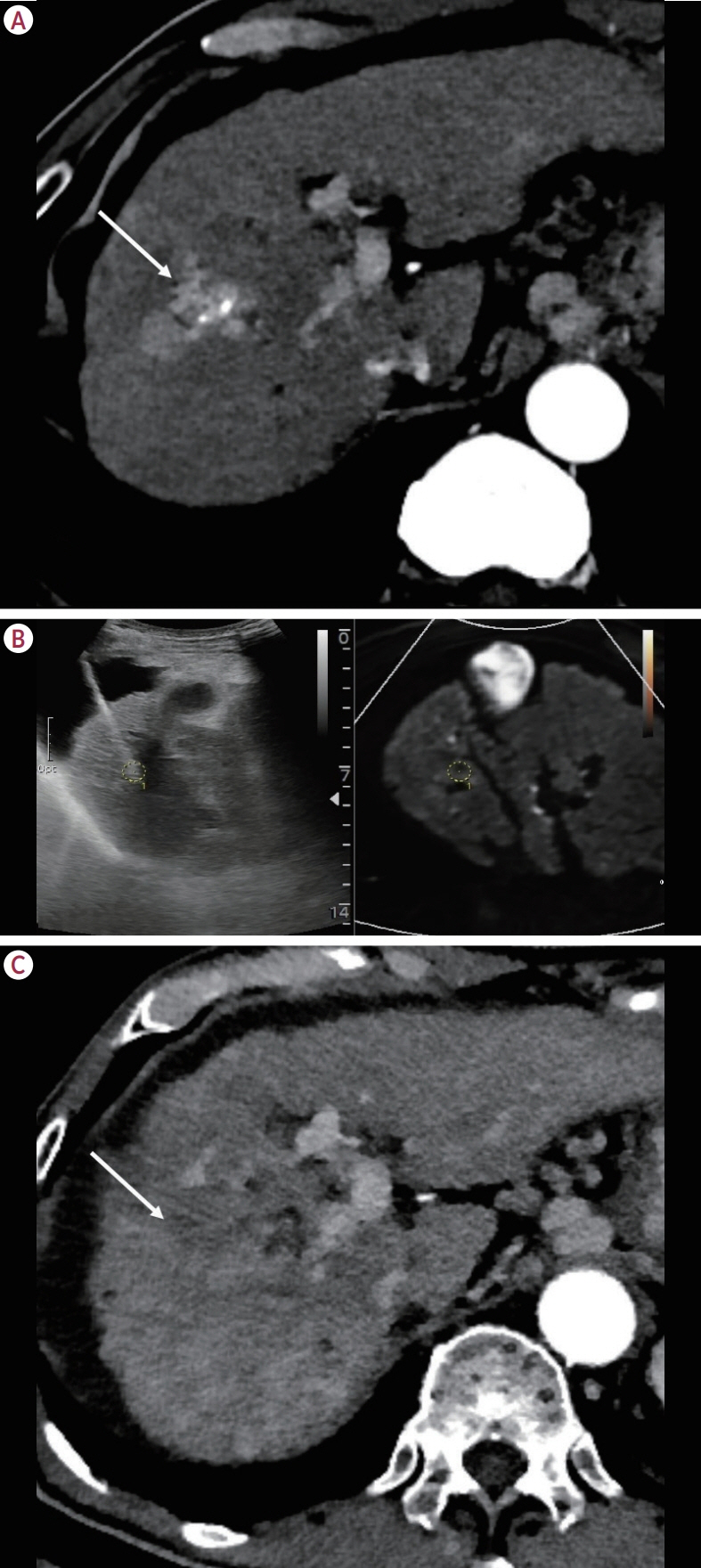
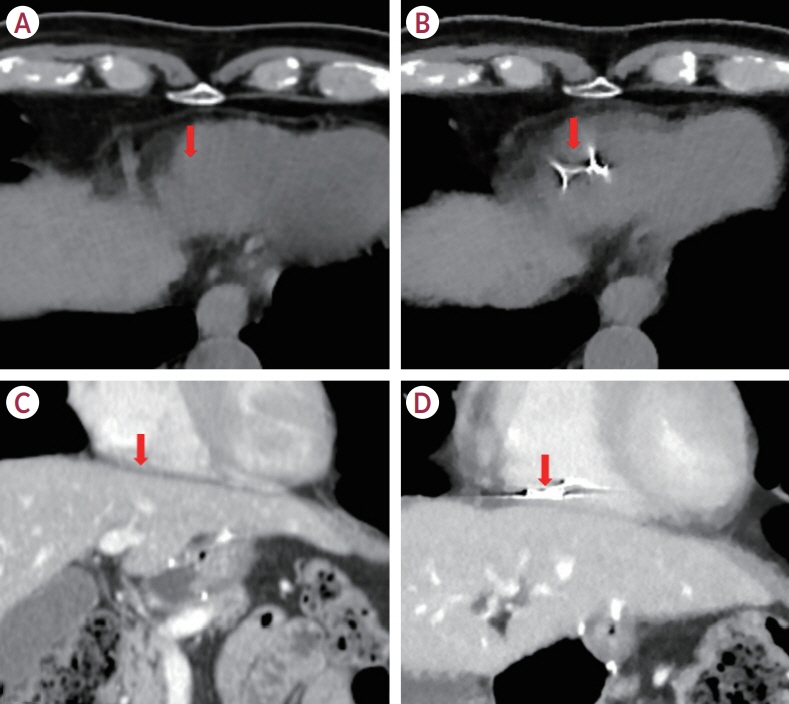
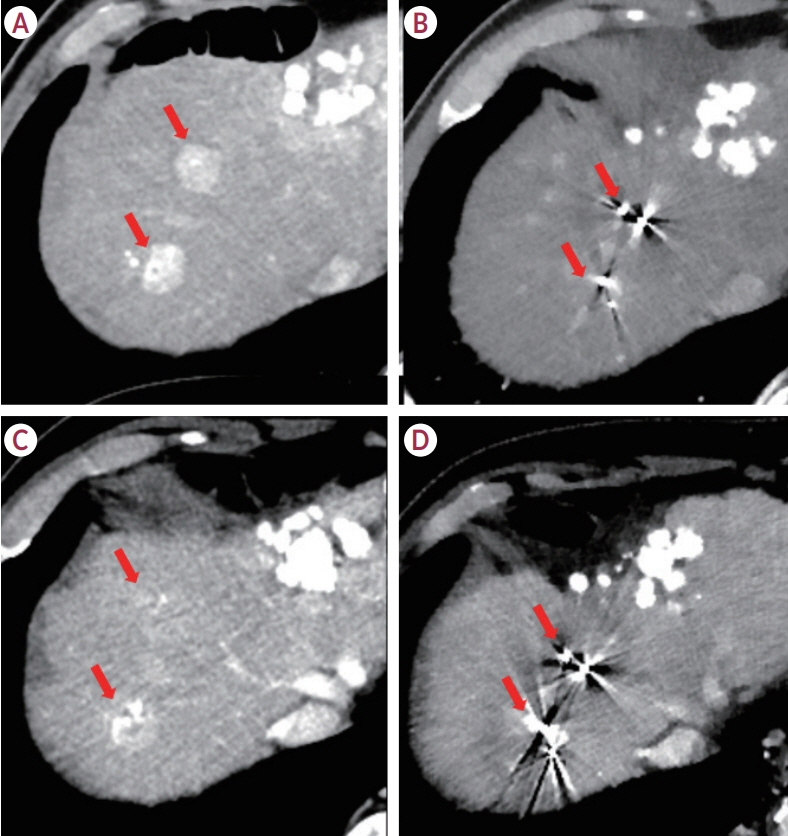
This study explored the initial institutional experience of using gold fiducial markers for stereotactic body radiotherapy (SBRT) in treating malignant hepatic tumors using real-time ultrasound-computed tomography (CT)/magnetic resonance (MR) imaging fusion-guided percutaneous placement.
Methods
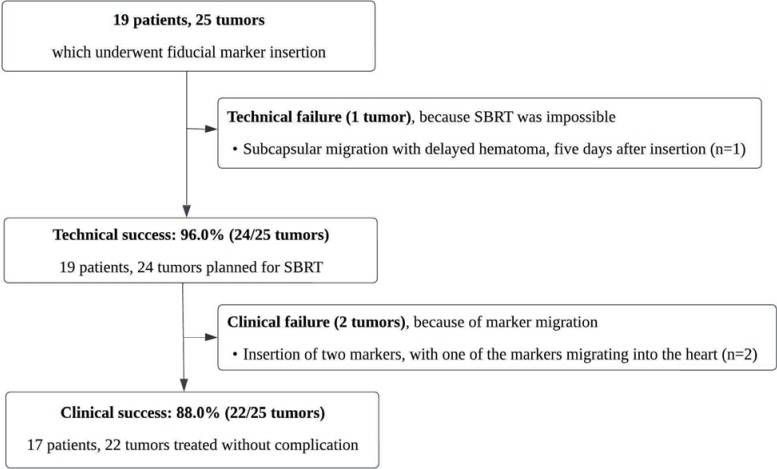
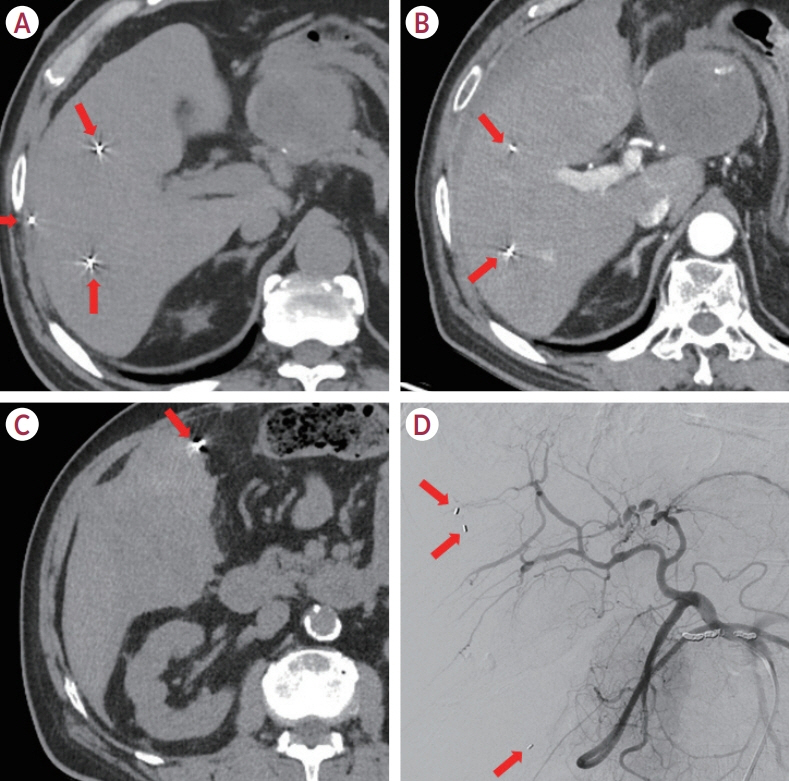
From May 2021 to August 2023, 19 patients with 25 liver tumors that were invisible on pre-contrast CT received fiducial markers following these guidelines. Postprocedural scans were used to confirm their placement. We assessed technical and clinical success rates and monitored complications. The implantation of fiducial markers facilitating adequate treatment prior to SBRT, which was achieved in 96% of the cases (24 of 25 tumors), was considered technical success. Clinical success was the successful completion of SBRT without evidence of marker displacement and was achieved in 88% of cases (22 of 25 tumors). Complications included one major subcapsular hematoma and marker migration into the right atrium in two cases, which prevented SBRT.
Results
Among the treated tumors, 20 of 24 (83.3%) showed a complete response, three of 24 (12.5%) remained stable, and one of 24 (4.2%) progressed during an average 11.7-month follow-up (range, 2-32 months).
Conclusions
This study confirms that percutaneous gold fiducial marker placement using real-time CT/MR guidance is effective and safe for SBRT in hepatic tumors, but warns of marker migration risks, especially near the hepatic veins and in subcapsular locations. Using fewer markers than traditionally recommended-typically two per patient, the outcomes were still satisfactory, particularly given the increased risk of migration when markers were placed near major hepatic veins.
Figure
Reference
-
References
1. Jackson WC, Tao Y, Mendiratta-Lala M, Bazzi L, Wahl DR, Schipper MJ, et al. Comparison of stereotactic body radiation therapy and radiofrequency ablation in the treatment of intrahepatic metastases. Int J Radiat Oncol Biol Phys. 2018; 100:950–958.
Article2. Lee MT, Kim JJ, Dinniwell R, Brierley J, Lockwood G, Wong R, et al. Phase I study of individualized stereotactic body radiotherapy of liver metastases. J Clin Oncol. 2009; 27:1585–1591.
Article3. Rusthoven KE, Kavanagh BD, Cardenes H, Stieber VW, Burri SH, Feigenberg SJ, et al. Multi-institutional phase I/II trial of stereotactic body radiation therapy for liver metastases. J Clin Oncol. 2009; 27:1572–1578.
Article4. Wahl DR, Stenmark MH, Tao Y, Pollom EL, Caoili EM, Lawrence TS, et al. Outcomes after stereotactic body radiotherapy or radiofrequency ablation for hepatocellular carcinoma. J Clin Oncol. 2016; 34:452–459.5. Kim JH, Lee JY, Yu SJ, Lee DH, Joo I, Yoon JH, et al. Fusion imagingguided radiofrequency ablation with artificial ascites or pleural effusion in patients with hepatocellular carcinomas: the feasibility rate and midterm outcome. Int J Hyperthermia. 2023; 40:2213424.
Article6. Vouche M, Habib A, Ward TJ, Kim E, Kulik L, Ganger D, et al. Unresectable solitary hepatocellular carcinoma not amenable to radiofrequency ablation: multicenter radiology-pathology correlation and survival of radiation segmentectomy. Hepatology. 2014; 60:192–201.
Article7. Rim CH, Lee JS, Kim SY, Seong J. Comparison of radiofrequency ablation and ablative external radiotherapy for the treatment of intrahepatic malignancies: a hybrid meta-analysis. JHEP Rep. 2022; 5:100594.
Article8. Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018; 67:358–380.
Article9. Korean Liver Cancer Association (KLCA); National Cancer Center (NCC) Korea. 2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma. J Liver Cancer. 2023; 23:1–120.10. Weykamp F, Hoegen P, Klüter S, Spindeldreier CK, König L, Seidensaal K, et al. Magnetic resonance-guided stereotactic body radiotherapy of liver tumors: initial clinical experience and patient-reported outcomes. Front Oncol. 2021; 11:610637.11. Jaffray DA, Siewerdsen JH, Wong JW, Martinez AA. Flat-panel conebeam computed tomography for image-guided radiation therapy. Int J Radiat Oncol Biol Phys. 2002; 53:1337–1349.
Article12. Lam KL, Ten Haken RK, McShan DL, Thornton AF Jr. Automated determination of patient setup errors in radiation therapy using spherical radio-opaque markers. Med Phys. 1993; 20:1145–1152.
Article13. Goodman KA, Kavanagh BD. Stereotactic body radiotherapy for liver metastases. Semin Radiat Oncol. 2017; 27:240–246.
Article14. Chang SD, Main W, Martin DP, Gibbs IC, Heilbrun MP. An analysis of the accuracy of the CyberKnife: a robotic frameless stereotactic radiosurgical system. Neurosurgery. 2003; 52:140–146. discussion 146-147.
Article15. Shirato H, Harada T, Harabayashi T, Hida K, Endo H, Kitamura K, et al. Feasibility of insertion/implantation of 2.0-mm-diameter gold internal fiducial markers for precise setup and real-time tumor tracking in radiotherapy. Int J Radiat Oncol Biol Phys. 2003; 56:240–247.16. Chang SD, Adler JR. Robotics and radiosurgery--the cyberknife. Stereotact Funct Neurosurg. 2001; 76:204–208.17. Moskalenko M, Jones BL, Mueller A, Lewis S, Shiao JC, Zakem SJ, et al. Fiducial markers allow accurate and reproducible delivery of liver stereotactic body radiation therapy. Curr Oncol. 2023; 30:5054–5061.
Article18. Oldrini G, Taste-George H, Renard-Oldrini S, Baumann AS, Marchesi V, Troufléau P, et al. Implantation of fiducial markers in the liver for stereotactic body radiation therapy: feasibility and results. Diagn Interv Imaging. 2015; 96:589–592.
Article19. Ohta K, Shimohira M, Iwata H, Hashizume T, Ogino H, Miyakawa A, et al. Percutaneous fiducial marker placement under CT fluoroscopic guidance for stereotactic body radiotherapy of the lung: an initial experience. J Radiat Res. 2013; 54:957–961.
Article20. Bertholet J, Worm E, Høyer M, Poulsen P. Cone beam CT-based set-up strategies with and without rotational correction for stereotactic body radiation therapy in the liver. Acta Oncol. 2017; 56:860–866.21. Sotiropoulou E, Stathochristopoulou I, Stathopoulos K, Verigos K, Salvaras N, Thanos L. CT-guided fiducial placement for cyberknife stereotactic radiosurgery: an initial experience. Cardiovasc Intervent Radiol. 2010; 33:586–589.
Article22. Anstadt EJ, Shumway R, Colasanto J, Grew D. Single community-based institutional series of stereotactic body radiation therapy (SBRT) for treatment of liver metastases. J Gastrointest Oncol. 2019; 10:330–338.
Article23. Han S, Lee JM, Lee DH, Yoon JH, Chang W. Utility of real-time CT/MRI-US automatic fusion system based on vascular matching in percutaneous radiofrequency ablation for hepatocellular carcinomas: a prospective study. Cardiovasc Intervent Radiol. 2021; 44:1579–1596.
Article24. Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010; 30:52–60.
Article25. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: fiveyear experience. Ann Surg. 2009; 250:187–196.26. Backlund EO, Johansson L, Sarby B. Studies on craniopharyngiomas. II. Treatment by stereotaxis and radiosurgery. Acta Chir Scand. 1972; 138:749–759.27. Lohr F, Debus J, Frank C, Herfarth K, Pastyr O, Rhein B, et al. Noninvasive patient fixation for extracranial stereotactic radiotherapy. Int J Radiat Oncol Biol Phys. 1999; 45:521–527.
Article28. Miura H, Doi Y, Nakao M, Ozawa S, Kenjo M, Nagata Y. Interfractional liver positional motion under exhaled breath holding based on cone beam computed tomography. In Vivo. 2023; 37:1822–1827.
Article29. Kim JH, Hong SS, Kim JH, Park HJ, Chang YW, Chang AR, et al. Safety and efficacy of ultrasound-guided fiducial marker implantation for CyberKnife radiation therapy. Korean J Radiol. 2012; 13:307–313.
Article30. Ohta K, Shimohira M, Murai T, Nishimura J, Iwata H, Ogino H, et al. Percutaneous fiducial marker placement prior to stereotactic body radiotherapy for malignant liver tumors: an initial experience. J Radiat Res. 2016; 57:174–177.31. Kothary N, Heit JJ, Louie JD, Kuo WT, Loo BW Jr, Koong A, et al. Safety and efficacy of percutaneous fiducial marker implantation for image-guided radiation therapy. J Vasc Interv Radiol. 2009; 20:235–239.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Ultrasound–Guided Fiducial Placement for Stereotactic Body Radiation Therapy in Pancreatic Malignancy
- Fiducial Placement for Stereotactic Body Radiation Therapy under Only Endoscopic Ultrasonography Guidance in Pancreatic and Hepatic Malignancy: Practical Feasibility and Safety
- Stereotactic Body Radiation Therapy
- Safety and Efficacy of Ultrasound-Guided Fiducial Marker Implantation for CyberKnife Radiation Therapy
- Assessment of Imaging Distortion in Magnetic Resonance Imaging for Stereotactic Radiosurgery: Through Phantom Study