J Cerebrovasc Endovasc Neurosurg.
2024 Sep;26(3):324-330. 10.7461/jcen.2024.E2023.04.010.
Primary Angiitis of Central Nervous System related intracranial aneurysm with spontaneous occlusion after immunomodulatory treatment
- Affiliations
-
- 1Department of Neurology and Neurointerventional Surgery, Neurological Institute (NI), Cleveland Clinic Abu Dhabi (CCAD), Abu Dhabi, UAE
- 2Department of Biomedical Engineering, Khalifa University, Abu Dhabi, UAE
- 3Department of Neurology, Neurological Institute (NI), Cleveland Clinic Abu Dhabi (CCAD), Abu Dhabi, UAE
- KMID: 2559444
- DOI: http://doi.org/10.7461/jcen.2024.E2023.04.010
Abstract
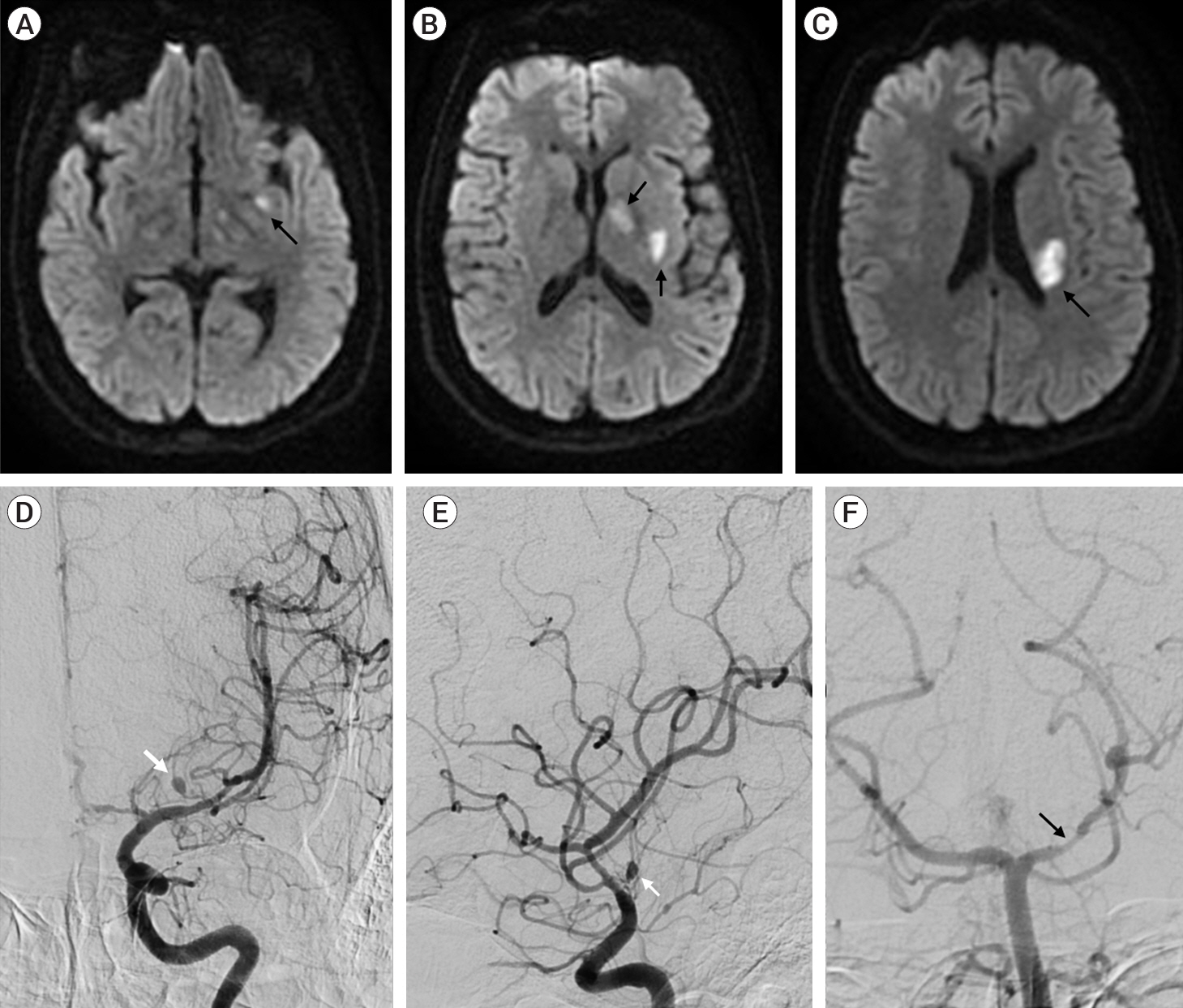
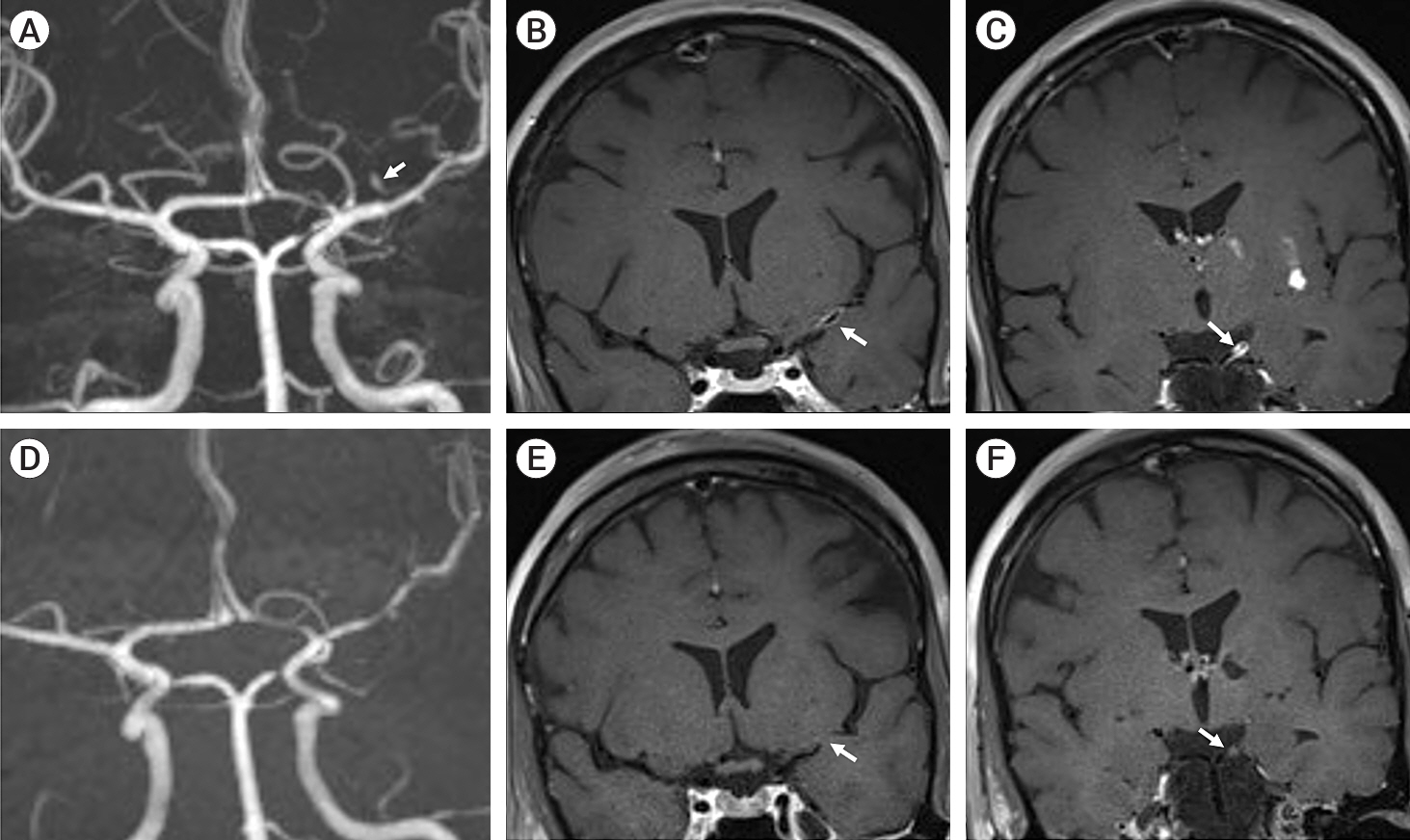
- Primary Angiitis of the Central Nervous System (PACNS) is an uncommon disease with kaleidoscopic clinical manifestations. Ischemic strokes are commoner than their hemorrhagic counterpart. Intracranial pseudoaneurysms are rarely reported in PACNS cohorts. We hereby describe the case of a 39-year-old female, who presented for evaluation of acute onset of left middle cerebral artery (MCA) ischemic stroke, with cerebral angiogram showing multifocal stenosis and irregularities in intracranial blood vessels with an aneurysm arising from the lenticulostriate branch of the left MCA M1 segment. A diagnosis of probable PACNS was made and patient initiated on immunomodulatory treatment with corticosteroids. 12 weeks follow up neuroimaging studies revealed resolution of the previously described intracranial aneurysm, thereby postulating the possibility of a pseudoaneurysm related to the underlying angiitis.
Figure
Reference
-
1. Calabrese LH, Duna GF, Lie JT. Vasculitis in the central nervous system. Arthritis Rheum. 1997; Jul. 40(7):1189–201.
Article2. de Boysson H, Zuber M, Naggara O, Neau JP, Gray F, Bousser MG, et al. Primary angiitis of the central nervous system: Description of the first fifty-two adults enrolled in the French cohort of patients with primary vasculitis of the central nervous system. Arthritis Rheumatol. 2014; May. 66(5):1315–26.
Article3. Gaillard N, Bertrand JL, Dumitrana A, Sablot D. Microaneurysms in primary angiitis of the central nervous system revealed by MRI. Cerebrovasc Dis. 2014; 38(4):308–10.
Article4. Pillai SH, Sreedharan SE, Menon G, Kannoth S, Pn S. Primary CNS vasculitis presenting as intraventricular bleeding. Ann Indian Acad Neurol. 2016; Jul-Sep. 19(3):406–8.
Article5. Pomper MG, Miller TJ, Stone JH, Tidmore WC, Hellmann DB. CNS vasculitis in autoimmune disease: MR imaging findings and correlation with angiography. AJNR Am J Neuroradiol. 1999; Jan. 20(1):75–85.6. Salvarani C, Brown RD Jr, Calamia KT, Christianson TJ, Huston J 3rd, Meschia JF, et al. Primary central nervous system vasculitis presenting with intracranial hemorrhage. Arthritis Rheum. 2011; Nov. 63(11):3598–606.
Article7. Salvarani C, Brown RD Jr, Calamia KT, Christianson TJ, Weigand SD, Miller DV, et al. Primary central nervous system vasculitis: Analysis of 101 patients. Ann Neurol. 2007; Nov. 62(5):442–51.
Article8. Salvarani C, Brown RD Jr, Hunder GG. Adult primary central nervous system vasculitis. Lancet. 2012; Aug. 380(9843):767–77.
Article9. Zheng Y, Lu Z, Shen J, Xu F. Intracranial pseudoaneurysms: Evaluation and management. Front Neurol. 2020; Jul. 11:582.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Angiitis of the Central Nervous System: A Case Presentation
- Childhood Primary Angiitis of the Central Nervous System Presenting as Isolated Middle Cerebral Artery Dissection
- Primary Angiitis of the Central Nervous System Presenting Tumefactive Lesions and Small Arteriolar Ectasias
- Necrotizing Primary Angiitis of the Central Nervous System Mimicking Brain Abscess: A Case Report and Literature Review
- The Teratoma of the Central Nervous System