Kosin Med J.
2024 Sep;39(3):153-159. 10.7180/kmj.24.129.
Oncoplastic breast-conserving surgery: evolution, techniques, and the emerging role of acellular dermal matrix
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Chonnam National University Hospital, Gwangju, Korea
- 2Department of Plastic and Reconstructive Surgery, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- KMID: 2559402
- DOI: http://doi.org/10.7180/kmj.24.129
Abstract
- Oncoplastic breast-conserving surgery (OBCS) has revolutionized breast cancer treatment, aiming to achieve optimal oncological outcomes while preserving an aesthetically favorable appearance. This review explores the evolution, techniques, and outcomes of OBCS, with a particular focus on the emerging role of acellular dermal matrix in volume replacement techniques. We conducted a comprehensive literature review using PubMed, Medline, and Cochrane databases, focusing on studies published between 2010 and 2024. OBCS demonstrates comparable oncological safety to traditional breast-conserving surgery, with local recurrence rates ranging from 2.7% to 5.7% at 5 years. Patient satisfaction rates are consistently high, with 85% to 95% reporting good to excellent aesthetic outcomes. Volume replacement techniques using acellular dermal matrix show promising results, with one study reporting that 94% of patients were highly satisfied with cosmetic outcomes. Although the current results are encouraging, future advancements in OBCS may require innovative approaches, including the integration of robotic surgery and artificial intelligence technologies.
Keyword
Figure
Reference
-
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–49.
Article2. Clough KB, Kaufman GJ, Nos C, Buccimazza I, Sarfati IM. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol. 2010; 17:1375–91.
Article3. Audretsch WP, Rezai M, Kolotas C, Zamboglou N, Schnabel T, Bojar H. Tumor-specific immediate reconstruction in breast cancer patients. Perspect Plast Surg. 1998; 11:71–100.
Article4. Clough KB, Nos C, Salmon RJ, Soussaline M, Durand JC. Conservative treatment of breast cancers by mammaplasty and irradiation: a new approach to lower quadrant tumors. Plast Reconstr Surg. 1995; 96:363–70.5. Silverstein MJ, Mai T, Savalia N, Vaince F, Guerra L. Oncoplastic breast conservation surgery: the new paradigm. J Surg Oncol. 2014; 110:82–9.6. In SK, Kim YS, Kim HS, Park JH, Kim HI, Yi HS, et al. Retrospective review of 108 breast reconstructions using the round block technique after breast-conserving surgery: indications, complications, and outcomes. Arch Plast Surg. 2020; 47:574–82.
Article7. Munhoz AM, Montag E, Gemperli R. Oncoplastic breast surgery: indications, techniques and perspectives. Gland Surg. 2013; 2:143–57.8. Lee JH, Kim HG, Lee WJ. Characterization and tissue incorporation of cross-linked human acellular dermal matrix. Biomaterials. 2015; 44:195–205.
Article9. Gwak H, Jeon YW, Lim ST, Park SY, Suh YJ. Volume replacement with diced acellular dermal matrix in oncoplastic breast-conserving surgery: a prospective single-center experience. World J Surg Oncol. 2020; 18:60.
Article10. De La Cruz L, Blankenship SA, Chatterjee A, Geha R, Nocera N, Czerniecki BJ, et al. Outcomes after oncoplastic breast-conserving surgery in breast cancer patients: a systematic literature review. Ann Surg Oncol. 2016; 23:3247–58.11. Clough KB, van la Parra RF, Thygesen HH, Levy E, Russ E, Halabi NM, et al. Long-term results after oncoplastic surgery for breast cancer: a 10-year follow-up. Ann Surg. 2018; 268:165–71.12. Down SK, Jha PK, Burger A, Hussien MI. Oncological advantages of oncoplastic breast-conserving surgery in treatment of early breast cancer. Breast J. 2013; 19:56–63.
Article13. Dikmans RE, Negenborn VL, Bouman MB, Winters HA, Twisk JW, Ruhe PQ, et al. Two-stage implant-based breast reconstruction compared with immediate one-stage implant-based breast reconstruction augmented with an acellular dermal matrix: an open-label, phase 4, multicentre, randomised, controlled trial. Lancet Oncol. 2017; 18:251–8.
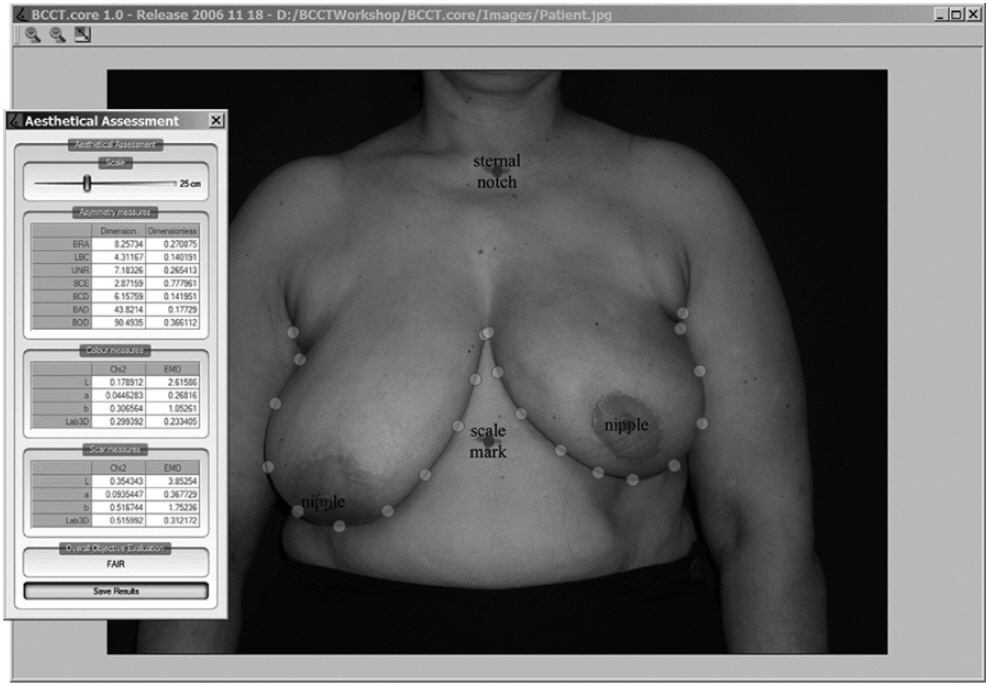
Article14. Cardoso MJ, Cardoso J, Amaral N, Azevedo I, Barreau L, Bernardo M, et al. Turning subjective into objective: the BCCT.core software for evaluation of cosmetic results in breast cancer conservative treatment. Breast. 2007; 16:456–61.
Article15. O’Connell RL, Di Micco R, Khabra K, Wolf L, deSouza N, Roche N, et al. The potential role of three-dimensional surface imaging as a tool to evaluate aesthetic outcome after breast conserving therapy (BCT). Breast Cancer Res Treat. 2017; 164:385–93.16. Jagsi R, Li Y, Morrow M, Janz N, Alderman A, Graff J, et al. Patient-reported quality of life and satisfaction with cosmetic outcomes after breast conservation and mastectomy with and without reconstruction: results of a survey of breast cancer survivors. Ann Surg. 2015; 261:1198–206.17. Santos G, Urban C, Edelweiss MI, Zucca-Matthes G, de Oliveira VM, Arana GH, et al. Long-term comparison of aesthetical outcomes after oncoplastic surgery and lumpectomy in breast cancer patients. Ann Surg Oncol. 2015; 22:2500–8.
Article18. Chen JY, Huang YJ, Zhang LL, Yang CQ, Wang K. Comparison of oncoplastic breast-conserving surgery and breast-conserving surgery alone: a meta-analysis. J Breast Cancer. 2018; 21:321–9.
Article19. Kaidar-Person O, Vrou Offersen B, Hol S, Arenas M, Aristei C, Bourgier C, et al. ESTRO ACROP consensus guideline for target volume delineation in the setting of postmastectomy radiation therapy after implant-based immediate reconstruction for early stage breast cancer. Radiother Oncol. 2019; 137:159–66.
Article20. Kronowitz SJ, Feledy JA, Hunt KK, Kuerer HM, Youssef A, Koutz CA, et al. Determining the optimal approach to breast reconstruction after partial mastectomy. Plast Reconstr Surg. 2006; 117:1–11.21. Weber WP, Soysal SD, El-Tamer M, Sacchini V, Knauer M, Tausch C, et al. First international consensus conference on standardization of oncoplastic breast conserving surgery. Breast Cancer Res Treat. 2017; 165:139–49.
Article22. Salzberg CA, Ashikari AY, Koch RM, Chabner-Thompson E. An 8-year experience of direct-to-implant immediate breast reconstruction using human acellular dermal matrix (AlloDerm). Plast Reconstr Surg. 2011; 127:514–24.
Article23. Sorkin M, Qi J, Kim HM, Hamill JB, Kozlow JH, Pusic AL, et al. Acellular dermal matrix in immediate expander/implant breast reconstruction: a multicenter assessment of risks and benefits. Plast Reconstr Surg. 2017; 140:1091–100.
Article24. Kim MY, Suh YJ, An YY. Imaging surveillance for the detection of ipsilateral local tumor recurrence in patients who underwent oncoplastic breast-conserving surgery with acellular dermal matrix: abbreviated MRI versus conventional mammography and ultrasonography. World J Surg Oncol. 2021; 19:290.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Follow-Up after Volume Replacement Using Acellular Dermal Matrix in Oncoplastic Breast-Conserving Surgery
- Safety and Effectiveness of Acellular Dermal Matrix in Breast-Conserving Surgery for Breast Cancer: A Single-Institution Study
- Comparison of Wound Closure Using Acellular Dermal Matrix With Primary Wound Closure After Breast Conserving Surgery in Breast Cancer Patients
- Use of Acellular Dermal Matrix in Reconstructive Surgery: A Review
- Long-term follow-up results and complications of breast-conserving surgery using multilayer acellular dermal matrix: a retrospective study