Clin Endosc.
2024 Sep;57(5):620-627. 10.5946/ce.2023.179.
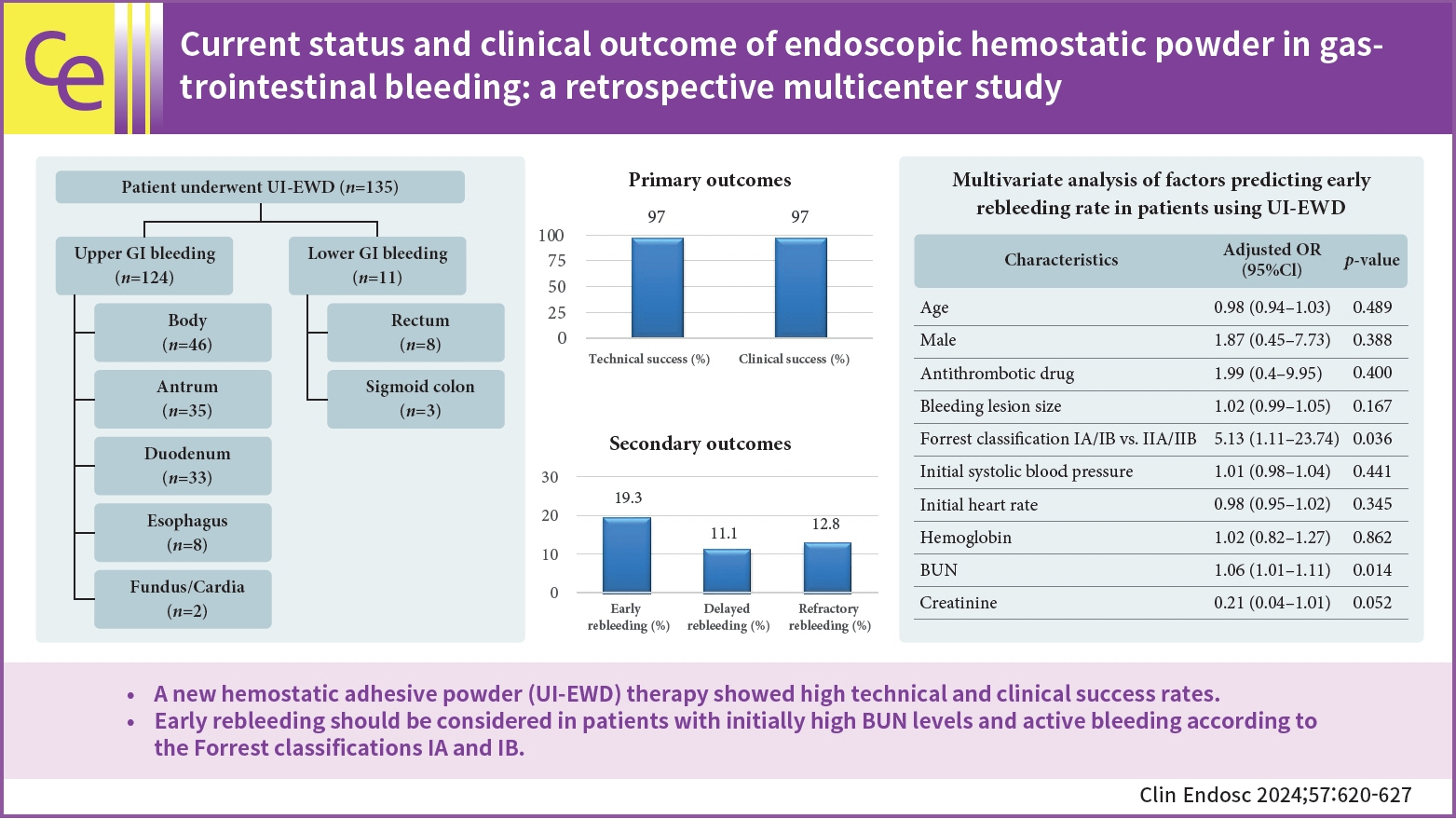
Current status and clinical outcome of endoscopic hemostatic powder in gastrointestinal bleeding: a retrospective multicenter study
- Affiliations
-
- 1Department of Internal Medicine, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea
- 3Division of Gastroenterology, Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- 4Department of Internal Medicine, Yeouido St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2559213
- DOI: http://doi.org/10.5946/ce.2023.179
Abstract
- Background/Aims
Few multicenter studies have investigated the efficacy of hemostatic powders in gastrointestinal (GI) bleeding. We aimed to investigate the clinical outcomes of hemostatic powder therapy and the independent factors affecting rebleeding rates.
Methods
We retrospectively recruited patients who underwent a new hemostatic adhesive powder (UI-EWD; Next-Biomedical) treatment for upper and lower GI bleeding between January 1, 2020 and March 1, 2023. We collected patients’ medical records and bleeding lesions. The primary outcomes were clinical and technical success rates, and the secondary outcomes were early, delayed, and refractory bleeding, mortality, and factors affecting early rebleeding rates.
Results
This study enrolled 135 patients (age: 67.7±13.6 years, male: 74.1%) from five hospitals. Indications for UI-EWD were peptic ulcers (51.1%), post-procedure-related bleeding (23.0%), and tumor bleeding (19.3%). The clinical and technical success rates were both 97%. The early, delayed, and refractory rebleeding rates were 19.3%, 11.1%, and 12.8%, respectively. Initially elevated blood urea nitrogen (BUN) levels (p=0.014) and Forrest classification IA or IB compared with IIA or IIB (p=0.036) were factors affecting early rebleeding.
Conclusions
UI-EWD showed high clinical and technical success rates; however, rebleeding after UI-EWD therapy in patients with initially high BUN levels and active bleeding, according to the Forrest classification, should be considered.
Keyword
Figure
Reference
-
1. Bong SH, Tan BW, Yong JM, et al. Bleeding on the edge-the use of hemostatic powder for treating a bleeding hypopharyngeal tumor. Clin Endosc. 2021; 54:441–442.2. Sung JJ, Chiu PW, Chan FK, et al. Asia-Pacific working group consensus on non-variceal upper gastrointestinal bleeding: an update 2018. Gut. 2018; 67:1757–1768.3. Aziz M, Weissman S, Mehta TI, et al. Efficacy of Hemospray in non-variceal upper gastrointestinal bleeding: a systematic review with meta-analysis. Ann Gastroenterol. 2020; 33:145–154.4. Cha B, Lee D, Shin J, et al. Hemostatic efficacy and safety of the hemostatic powder UI-EWD in patients with lower gastrointestinal bleeding. BMC Gastroenterol. 2022; 22:170.5. Park JS, Bang BW, Hong SJ, et al. Efficacy of a novel hemostatic adhesive powder in patients with refractory upper gastrointestinal bleeding: a pilot study. Endoscopy. 2019; 51:458–462.6. Park JS, Kim HK, Shin YW, et al. Novel hemostatic adhesive powder for nonvariceal upper gastrointestinal bleeding. Endosc Int Open. 2019; 7:E1763–E1767.7. Jung DH, Moon HS, Park CH, et al. Polysaccharide hemostatic powder to prevent bleeding after endoscopic submucosal dissection in high risk patients: a randomized controlled trial. Endoscopy. 2021; 53:994–1002.8. Park JC, Kim YJ, Kim EH, et al. Effectiveness of the polysaccharide hemostatic powder in non-variceal upper gastrointestinal bleeding: using propensity score matching. J Gastroenterol Hepatol. 2018; 33:1500–1506.9. Bang BW, Lee DH, Kim HK, et al. CEGP-003 spray has a similar hemostatic effect to epinephrine injection in cases of acute upper gastrointestinal bleeding. Dig Dis Sci. 2018; 63:3026–3032.10. Baracat FI, de Moura DT, Brunaldi VO, et al. Randomized controlled trial of hemostatic powder versus endoscopic clipping for non-variceal upper gastrointestinal bleeding. Surg Endosc. 2020; 34:317–324.11. Lau JY, Pittayanon R, Kwek A, et al. Comparison of a hemostatic powder and standard treatment in the control of active bleeding from upper nonvariceal lesions: a multicenter, noninferiority, randomized trial. Ann Intern Med. 2022; 175:171–178.12. Mutneja H, Bhurwal A, Go A, et al. Efficacy of hemospray in upper gastrointestinal bleeding: a systematic review and meta-analysis. J Gastrointestin Liver Dis. 2020; 29:69–76.13. Ofosu A, Ramai D, John F, et al. The efficacy and safety of hemospray for the management of gastrointestinal bleeding: a systematic review and meta-analysis. J Clin Gastroenterol. 2021; 55:e37–e45.14. Sung JJ, Moreea S, Dhaliwal H, et al. Use of topical mineral powder as monotherapy for treatment of active peptic ulcer bleeding. Gastrointest Endosc. 2022; 96:28–35.15. Rodríguez de Santiago E, Burgos-Santamaría D, Pérez-Carazo L, et al. Hemostatic spray powder TC-325 for GI bleeding in a nationwide study: survival and predictors of failure via competing risks analysis. Gastrointest Endosc. 2019; 90:581–590.16. Shin J, Cha B, Park JS, et al. Efficacy of a novel hemostatic adhesive powder in patients with upper gastrointestinal tumor bleeding. BMC Gastroenterol. 2021; 21:40.17. Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) Guideline: Update 2021. Endoscopy. 2021; 53:300–332.18. Laine L, Barkun AN, Saltzman JR, et al. ACG clinical guideline: upper gastrointestinal and ulcer bleeding. Am J Gastroenterol. 2021; 116:899–917.19. Galloro G, Zullo A, Luglio G, et al. Endoscopic clipping in non-variceal upper gastrointestinal bleeding treatment. Clin Endosc. 2022; 55:339–346.20. de Groot NL, van Oijen MG, Kessels K, et al. Reassessment of the predictive value of the Forrest classification for peptic ulcer rebleeding and mortality: can classification be simplified? Endoscopy. 2014; 46:46–52.21. Bryant RV, Kuo P, Williamson K, et al. Performance of the Glasgow-Blatchford score in predicting clinical outcomes and intervention in hospitalized patients with upper GI bleeding. Gastrointest Endosc. 2013; 78:576–583.22. Stanley AJ. Update on risk scoring systems for patients with upper gastrointestinal haemorrhage. World J Gastroenterol. 2012; 18:2739–2744.23. Chang A, Ouejiaraphant C, Akarapatima K, et al. Prospective comparison of the AIMS65 score, Glasgow-Blatchford score, and Rockall score for predicting clinical outcomes in patients with variceal and nonvariceal upper gastrointestinal bleeding. Clin Endosc. 2021; 54:211–221.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Hemostatic Treatment of Peptic Ulcer Bleeding
- Clinical Evaluation of Endoscopic Microwave Coagulation Therapy for Upper Gastrointestinal Bleeding
- Endoscopic Therapy for Acute Diverticular Bleeding
- Recent Developments in the Endoscopic Treatment of Patients with Peptic Ulcer Bleeding
- Endoscopy for Nonvariceal Upper Gastrointestinal Bleeding