Clin Endosc.
2024 Sep;57(5):559-570. 10.5946/ce.2023.263.
Surveillance for metachronous cancers after endoscopic resection of esophageal squamous cell carcinoma
- Affiliations
-
- 1Department of Gastrointestinal Oncology, Osaka International Cancer Institute, Osaka, Japan
- KMID: 2559204
- DOI: http://doi.org/10.5946/ce.2023.263
Abstract
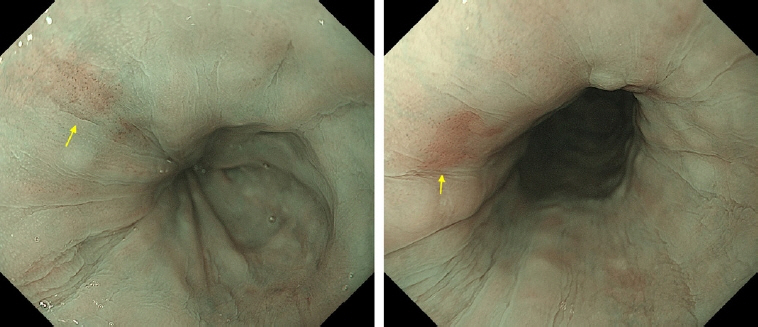
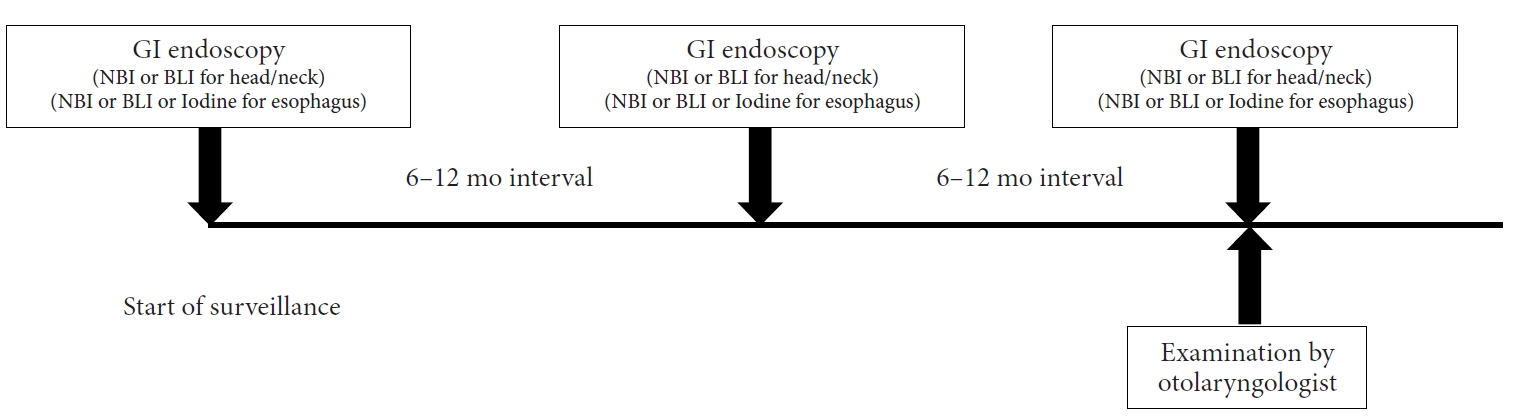
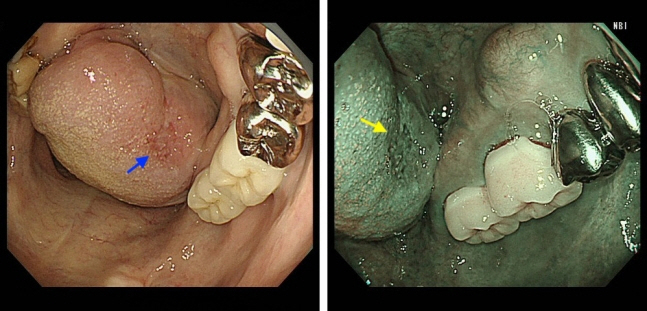
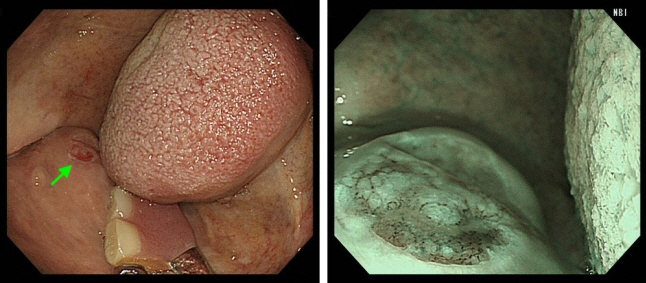
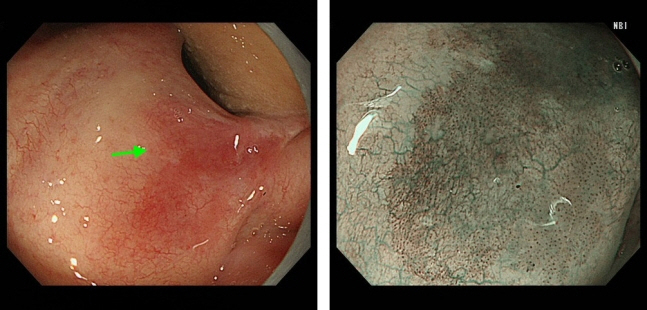
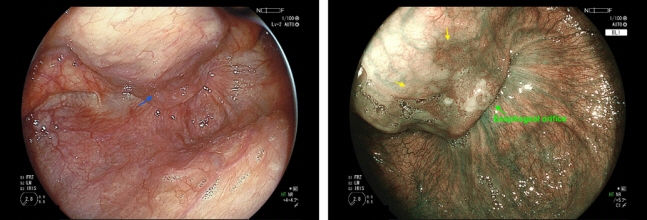
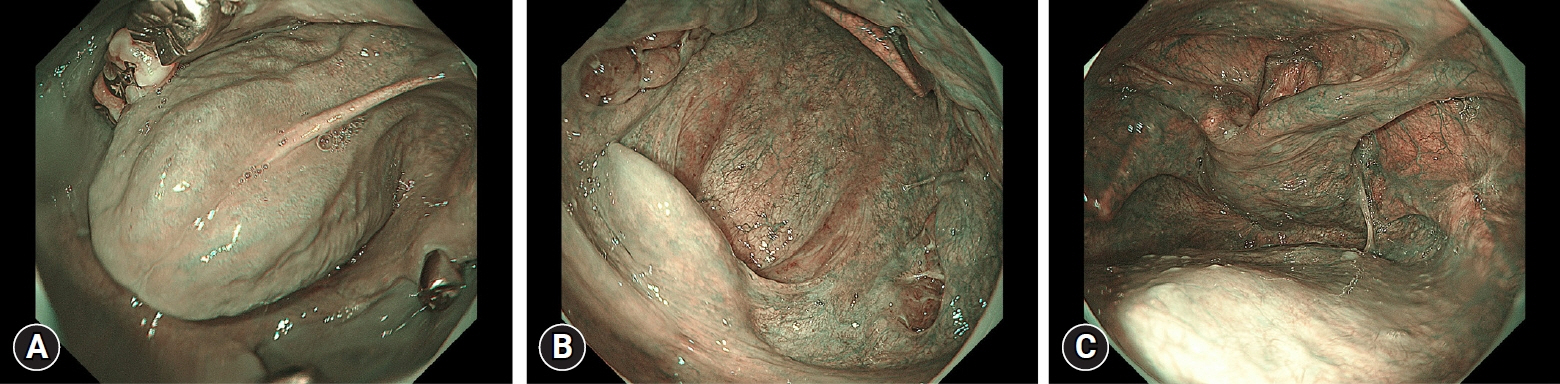
- The literature pertaining to surveillance following treatment for esophageal squamous cell carcinoma (SCC) was reviewed and summarized, encompassing the current status and future perspectives. Analysis of the standardized mortality and incidence ratios for these cancers indicates an elevated risk of cancer in the oral cavity, pharynx, larynx, and lungs among patients with esophageal SCC compared to the general population. To enhance the efficacy of surveillance for these metachronous cancers, risk stratification is needed. Various factors, including multiple Lugol-voiding lesions, multiple foci of dilated vascular areas, young age, and high mean corpuscular volume, have been identified as predictors of metachronous SCCs. Current practice involves stratifying the risk of metachronous esophageal and head/neck SCCs based on the presence of multiple Lugol-voiding lesions. Endoscopic surveillance, scheduled 6–12 months post-endoscopic resection, has demonstrated effectiveness, with over 90% of metachronous esophageal SCCs treatable through minimally invasive modalities. Narrow-band imaging emerges as the preferred surveillance method for esophageal and head/neck SCC based on comparative studies of various imaging techniques. Innovative approaches, such as artificial intelligence-assisted detection systems and radiofrequency ablation of high-risk background mucosa, may improve outcomes in patients following endoscopic resection.
Keyword
Figure
Reference
-
1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.2. Lagergren J, Smyth E, Cunningham D, et al. Oesophageal cancer. Lancet. 2017; 390:2383–2396.3. Yamashina T, Ishihara R, Nagai K, et al. Long-term outcome and metastatic risk after endoscopic resection of superficial esophageal squamous cell carcinoma. Am J Gastroenterol. 2013; 108:544–551.4. Kato K, Ito Y, Nozaki I, et al. Parallel-group controlled trial of surgery versus chemoradiotherapy in patients with stage I esophageal squamous cell carcinoma. Gastroenterology. 2021; 161:1878–1886.5. Ishihara R, Arima M, Iizuka T, et al. Endoscopic submucosal dissection/endoscopic mucosal resection guidelines for esophageal cancer. Dig Endosc. 2020; 32:452–493.6. Kitagawa Y, Ishihara R, Ishikawa H, et al. Esophageal cancer practice guidelines 2022 edited by the Japan Esophageal Society: Part 1. Esophagus. 2023; 20:343–372.7. Iwai N, Dohi O, Yamada S, et al. Prognostic risk factors associated with esophageal squamous cell carcinoma patients undergoing endoscopic submucosal dissection: a multi-center cohort study. Surg Endosc. 2022; 36:2279–2289.8. Ishihara R, Tanaka H, Iishi H, et al. Long-term outcome of esophageal mucosal squamous cell carcinoma without lymphovascular involvement after endoscopic resection. Cancer. 2008; 112:2166–2172.9. Slaughter DP, Southwick HW, Smejkal W. Field cancerization in oral stratified squamous epithelium: clinical implications of multicentric origin. Cancer. 1953; 6:963–968.10. Yokoyama A, Ohmori T, Muramatsu T, et al. Cancer screening of upper aerodigestive tract in Japanese alcoholics with reference to drinking and smoking habits and aldehyde dehydrogenase-2 genotype. Int J Cancer. 1996; 68:313–316.11. Dresler CM, León ME, Straif K, et al. Reversal of risk upon quitting smoking. Lancet. 2006; 368:348–349.12. Chuang SC, Hashibe M, Scelo G, et al. Risk of second primary cancer among esophageal cancer patients: a pooled analysis of 13 cancer registries. Cancer Epidemiol Biomarkers Prev. 2008; 17:1543–1549.13. Chen SC, Teng CJ, Hu YW, et al. Secondary primary malignancy risk among patients with esophageal cancer in Taiwan: a nationwide population-based study. PLoS One. 2015; 10:e0116384.14. Matsubara T, Yamada K, Nakagawa A. Risk of second primary malignancy after esophagectomy for squamous cell carcinoma of the thoracic esophagus. J Clin Oncol. 2003; 21:4336–4341.15. Delgado-Rodríguez M, Llorca J. Bias. J Epidemiol Community Health. 2004; 58:635–641.16. dos Santos SI. Cancer epidemiology: principles and methods. International Agency for Research on Cancer;1999.17. Ohmori M, Ishihara R, Morishima T, et al. Excessive risk of second-cancer incidence and cancer mortality in patients with esophageal cancer. J Gastroenterol. 2021; 56:434–441.18. Kato M, Ishihara R, Hamada K, et al. Endoscopic surveillance of head and neck cancer in patients with esophageal squamous cell carcinoma. Endosc Int Open. 2016; 4:E752–E755.19. Katada C, Yokoyama T, Yano T, et al. Alcohol consumption and multiple dysplastic lesions increase risk of squamous cell carcinoma in the esophagus, head, and neck. Gastroenterology. 2016; 151:860–869.20. Kondo H, Fukuda H, Ono H, et al. Sodium thiosulfate solution spray for relief of irritation caused by Lugol's stain in chromoendoscopy. Gastrointest Endosc. 2001; 53:199–202.21. Matsuno K, Ishihara R, Nakagawa K, et al. Endoscopic findings corresponding to multiple Lugol-voiding lesions in the esophageal background mucosa. J Gastroenterol Hepatol. 2019; 34:390–396.22. Kawakami Y, Ishihara R, Matsuno K, et al. Multiple foci of dilated vessels as a new predictor of metachronous esophageal cancer. Dig Endosc. 2024; 36:421–427.23. Azuma Y, Dohi O, Naito Y, et al. Blue laser imaging identifies endoscopic findings corresponding to metachronous esophageal squamous cell carcinoma. Esophagus. 2022; 19:278–286.24. Maekawa A, Ishihara R, Iwatsubo T, et al. High incidence of head and neck cancers after endoscopic resection for esophageal cancer in younger patients. J Gastroenterol. 2020; 55:401–407.25. Katada C, Yokoyama T, Yano T, et al. Association between macrocytosis and metachronous squamous cell carcinoma of the esophagus after endoscopic resection in men with early esophageal squamous cell carcinoma. Esophagus. 2020; 17:149–158.26. Kagemoto K, Urabe Y, Miwata T, et al. ADH1B and ALDH2 are associated with metachronous SCC after endoscopic submucosal dissection of esophageal squamous cell carcinoma. Cancer Med. 2016; 5:1397–1404.27. Matsueda K, Ishihara R, Morishima T, et al. Impact of endoscopic surveillance on mortality of metachronous esophageal and head and neck cancer after esophageal endoscopic resection. J Gastroenterol Hepatol. 2022; 37:2098–2104.28. Jiang D, Li X, Wang H, et al. A retrospective study of endoscopic resection for 368 patients with early esophageal squamous cell carcinoma or precancerous lesions. Surg Endosc. 2017; 31:2122–2130.29. Oda I, Shimizu Y, Yoshio T, et al. Long-term outcome of endoscopic resection for intramucosal esophageal squamous cell cancer: a secondary analysis of the Japan Esophageal Cohort study. Endoscopy. 2020; 52:967–975.30. Suzuki Y, Kikuchi D, Hoteya S, et al. Effectiveness of chemoradiotherapy for metachronous esophageal squamous cell carcinoma. Digestion. 2021; 102:622–629.31. Hsu MH, Wang WL, Chen TH, et al. Long-term outcomes of endoscopic submucosal dissection for superficial esophageal squamous cell carcinoma in Taiwan. BMC Gastroenterol. 2021; 21:308.32. Shinozaki T, Katada C, Shiga K, et al. Effectiveness of planned surveillance for detecting second primary head and neck cancers after endoscopic resection of esophageal squamous cell carcinoma. Jpn J Clin Oncol. 2020; 50:1162–1167.33. Muto M, Minashi K, Yano T, et al. Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: a multicenter randomized controlled trial. J Clin Oncol. 2010; 28:1566–1572.34. Kawai T, Takagi Y, Yamamoto K, et al. Narrow-band imaging on screening of esophageal lesions using an ultrathin transnasal endoscopy. J Gastroenterol Hepatol. 2012; 27 Suppl 3:34–39.35. Ono S, Kawada K, Dohi O, et al. Linked color imaging focused on neoplasm detection in the upper gastrointestinal tract: a randomized trial. Ann Intern Med. 2021; 174:18–24.36. Kawada K, Arima M, Miyahara R, et al. Effect of adding magnifying BLI, magnifying NBI, and iodine staining to white light imaging in diagnosis of early esophageal cancer. Endosc Int Open. 2021; 9:E1877–E1885.37. Ogata Y, Hatta W, Koike T, et al. Blue light imaging and linked color imaging as a screening mode for esophageal squamous cell carcinoma in high-risk patients: multicenter randomized trial. Dig Endosc. 2023; 35:835–844.38. Dubuc J, Legoux JL, Winnock M, et al. Endoscopic screening for esophageal squamous-cell carcinoma in high-risk patients: a prospective study conducted in 62 French endoscopy centers. Endoscopy. 2006; 38:690–695.39. Ide E, Maluf-Filho F, Chaves DM, et al. Narrow-band imaging without magnification for detecting early esophageal squamous cell carcinoma. World J Gastroenterol. 2011; 17:4408–4413.40. Yokoyama A, Ichimasa K, Ishiguro T, et al. Is it proper to use non-magnified narrow-band imaging for esophageal neoplasia screening? Japanese single-center, prospective study. Dig Endosc. 2012; 24:412–418.41. Gruner M, Denis A, Masliah C, et al. Narrow-band imaging versus Lugol chromoendoscopy for esophageal squamous cell cancer screening in normal endoscopic practice: randomized controlled trial. Endoscopy. 2021; 53:674–682.42. Nagami Y, Tominaga K, Machida H, et al. Usefulness of non-magnifying narrow-band imaging in screening of early esophageal squamous cell carcinoma: a prospective comparative study using propensity score matching. Am J Gastroenterol. 2014; 109:845–854.43. Iwatsubo T, Ishihara R, Yamasaki Y, et al. Narrow band imaging under less-air condition improves the visibility of superficial esophageal squamous cell carcinoma. BMC Gastroenterol. 2020; 20:389.44. Yamasaki Y, Ishihara R, Hanaoka N, et al. Pethidine hydrochloride is a better sedation method for pharyngeal observation by transoral endoscopy compared with no sedation and midazolam. Dig Endosc. 2017; 29:39–48.45. Iwatsubo T, Ishihara R, Nakagawa K, et al. Pharyngeal observation via transoral endoscopy using a lip cover-type mouthpiece. J Gastroenterol Hepatol. 2019; 34:1384–1389.46. Ohmori M, Ishihara R, Aoyama K, et al. Endoscopic detection and differentiation of esophageal lesions using a deep neural network. Gastrointest Endosc. 2020; 91:301–309.47. Ishihara R, Takeuchi Y, Chatani R, et al. Prospective evaluation of narrow-band imaging endoscopy for screening of esophageal squamous mucosal high-grade neoplasia in experienced and less experienced endoscopists. Dis Esophagus. 2010; 23:480–486.48. Luo H, Xu G, Li C, et al. Real-time artificial intelligence for detection of upper gastrointestinal cancer by endoscopy: a multicentre, case-control, diagnostic study. Lancet Oncol. 2019; 20:1645–1654.49. Waki K, Ishihara R, Kato Y, et al. Usefulness of an artificial intelligence system for the detection of esophageal squamous cell carcinoma evaluated with videos simulating overlooking situation. Dig Endosc. 2021; 33:1101–1109.50. Chen Z, Dou L, Liu Y, et al. Combination of endoscopic resection and radiofrequency ablation for the treatment of esophageal squamous cell neoplasia with multiple lugol-voiding lesions. Front Oncol. 2021; 11:786015.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Clinical Management of Esophageal Squamous Dysplasia
- Endoscopic Treatment for Esophageal Cancer
- Metachronous Cancer Occurring after Endoscopic Resection of Superficial Esophageal Cancer
- Endoscopic Submucosal Dissection for Esophageal Squamous Cell Carcinoma
- Cutaneous Metastasis of Esophageal Squamous Cell Carcinoma Mimicking Benign Soft Tissue Tumor