J Korean Med Sci.
2024 Sep;39(35):e241. 10.3346/jkms.2024.39.e241.
Impact of Preanesthetic Blood Pressure Deviations on 30-Day Postoperative Mortality in Non-Cardiac Surgery Patients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Asan Medical Center, Brain Korea 21 Project, University of Ulsan College of Medicine, Seoul, Korea
- 2Cancer Data Science Laboratory, National Cancer Institute, National Institutes of Health, Bethesda, MD, USA
- 3Biomedical Engineering Research Center, Biosignal Analysis & Perioperative Outcome Research (BAPOR) Laboratory, Asan Institute for Lifesciences, Seoul, Korea
- KMID: 2559194
- DOI: http://doi.org/10.3346/jkms.2024.39.e241
Abstract
- Background
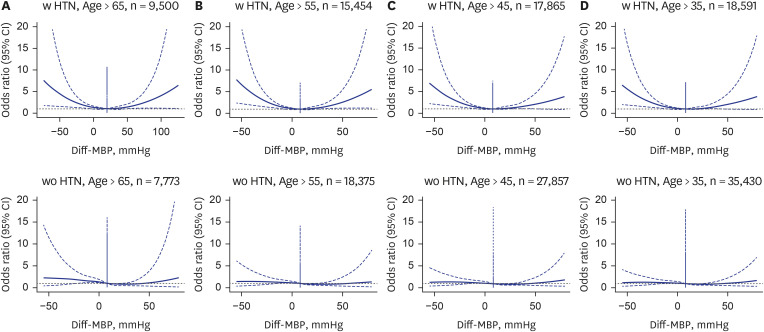
Blood pressure readings taken before anesthesia often influence the decision to delay or cancel elective surgeries. However, the implications of these specific blood pressure values, especially how they compare to baseline, on postoperative in-hospital 30-day mortality remain underexplored. This research aimed to examine the effect of discrepancies between the baseline blood pressure evaluated in the ward a day before surgery, and the blood pressure observed just before the administration of anesthesia, on the postoperative mortality risks.
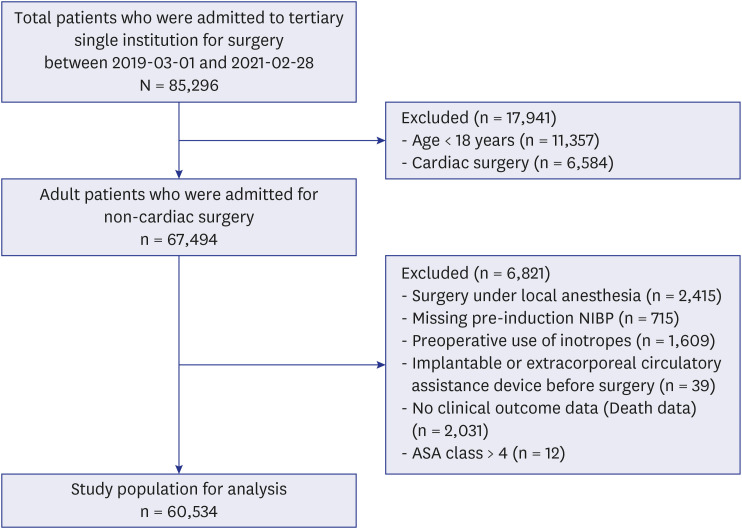
Methods
The study encompassed 60,534 adults scheduled for non-cardiac surgeries at a tertiary care center in Seoul, Korea. Baseline blood pressure was calculated as the mean of the blood pressure readings taken within 24 hours prior to surgery. The preanesthetic blood pressure was the blood pressure measured right before the administration of anesthesia. We focused on in-hospital 30-day mortality as the primary outcome.
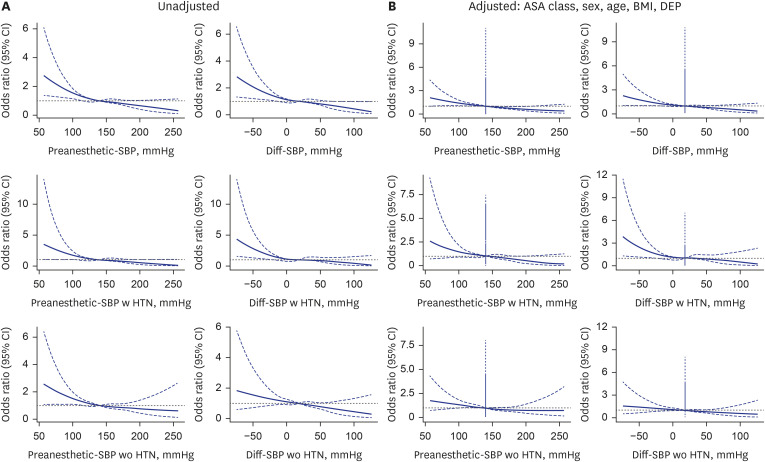
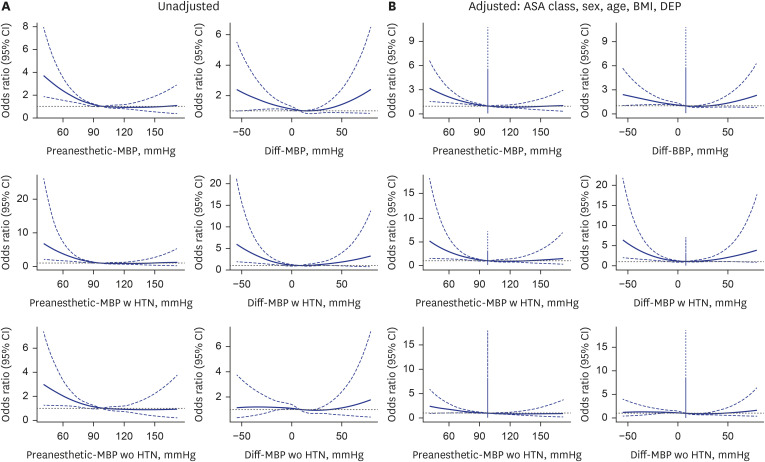
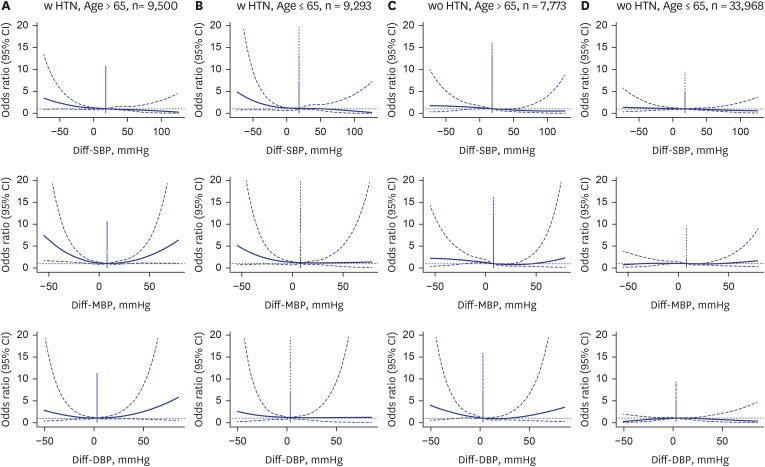
Results
Our research revealed that a lower preanesthetic systolic or mean blood pressure that deviates by 20 mmHg or more from baseline significantly increased the risk of 30-day mortality. This association was particularly pronounced in individuals with a history of hypertension and those aged 65 and above. Higher preanesthetic blood pressure was not significantly associated with an increased risk of 30-day mortality.
Conclusion
We found that a lower preanesthetic blood pressure compared to baseline significantly increased the 30-day postoperative mortality risk, whereas a higher preanesthetic blood pressure did not. Our study emphasizes the critical importance of accounting for variations in both baseline and preanesthetic blood pressure when assessing surgical risks and outcomes.
Keyword
Figure
Reference
-
1. Sanders RD, Hughes F, Shaw A, Thompson A, Bader A, Hoeft A, et al. Perioperative Quality Initiative consensus statement on preoperative blood pressure, risk and outcomes for elective surgery. Br J Anaesth. 2019; 122(5):552–562. PMID: 30916006.2. Wax DB, Porter SB, Lin HM, Hossain S, Reich DL. Association of preanesthesia hypertension with adverse outcomes. J Cardiothorac Vasc Anesth. 2010; 24(6):927–930. PMID: 20817562.3. Abdelmalak BB, Abd-Elsayed AA, Dalton JE, Abdelmalak JB, Lawrence JP, Doyle DJ, et al. The association between preinduction arterial blood pressure and postoperative cardiovascular, renal, and neurologic morbidity, and in-hospital mortality in elective noncardiac surgery: an observational study. J Hypertens. 2018; 36(11):2251–2259. PMID: 30044311.4. Sear JW. Perioperative control of hypertension: when will it adversely affect perioperative outcome? Curr Hypertens Rep. 2008; 10(6):480–487. PMID: 18959836.5. Howell SJ, Sear YM, Yeates D, Goldacre M, Sear JW, Foëx P. Hypertension, admission blood pressure and perioperative cardiovascular risk. Anaesthesia. 1996; 51(11):1000–1004. PMID: 8943587.6. Howell SJ, Sear YM, Yeates D, Goldacre M, Sear JW, Foëx P. Risk factors for cardiovascular death after elective surgery under general anaesthesia. Br J Anaesth. 1998; 80(1):14–19. PMID: 9505771.7. Goldman L, Caldera DL. Risks of general anesthesia and elective operation in the hypertensive patient. Anesthesiology. 1979; 50(4):285–292. PMID: 434530.8. Aronson S, Boisvert D, Lapp W. Isolated systolic hypertension is associated with adverse outcomes from coronary artery bypass grafting surgery. Anesth Analg. 2002; 94(5):1079–1084. PMID: 11973166.9. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991; 265(24):3255–3264. PMID: 2046107.10. Rutan GH, McDonald RH, Kuller LH. A historical perspective of elevated systolic vs diastolic blood pressure from an epidemiological and clinical trial viewpoint. J Clin Epidemiol. 1989; 42(7):663–673. PMID: 2668449.11. Nikolov NM, Fontes ML, White WD, Aronson S, Bar-Yosef S, Gaca JG, et al. Pulse pressure and long-term survival after coronary artery bypass graft surgery. Anesth Analg. 2010; 110(2):335–340. PMID: 19996138.12. Vaccarino V, Holford TR, Krumholz HM. Pulse pressure and risk for myocardial infarction and heart failure in the elderly. J Am Coll Cardiol. 2000; 36(1):130–138. PMID: 10898424.13. Asopa A, Jidge S, Schermerhorn ML, Hess PE, Matyal R, Subramaniam B. Preoperative pulse pressure and major perioperative adverse cardiovascular outcomes after lower extremity vascular bypass surgery. Anesth Analg. 2012; 114(6):1177–1181. PMID: 21821518.14. Mazzeffi M, Flynn B, Bodian C, Bronheim D. Preoperative arterial pulse pressure has no apparent association with perioperative mortality after lower extremity arterial bypass. Anesth Analg. 2012; 114(6):1170–1176. PMID: 21642608.15. Cheung CC, Martyn A, Campbell N, Frost S, Gilbert K, Michota F, et al. Predictors of intraoperative hypotension and bradycardia. Am J Med. 2015; 128(5):532–538. PMID: 25541033.16. Venkatesan S, Myles PR, Manning HJ, Mozid AM, Andersson C, Jørgensen ME, et al. Cohort study of preoperative blood pressure and risk of 30-day mortality after elective non-cardiac surgery. Br J Anaesth. 2017; 119(1):65–77. PMID: 28633374.17. Howell SJ, Sear JW, Foëx P. Hypertension, hypertensive heart disease and perioperative cardiac risk. Br J Anaesth. 2004; 92(4):570–583. PMID: 15013960.18. Drummond JC, Blake JL, Patel PM, Clopton P, Schulteis G. An observational study of the influence of “white-coat hypertension” on day-of-surgery blood pressure determinations. J Neurosurg Anesthesiol. 2013; 25(2):154–161. PMID: 23211641.19. Schonberger RB, Burg MM, Holt N, Lukens CL, Dai F, Brandt C. The relationship between preoperative and primary care blood pressure among veterans presenting from home for surgery: is there evidence for anesthesiologist-initiated blood pressure referral? Anesth Analg. 2012; 114(1):205–214. PMID: 22075017.20. van Klei WA, van Waes JA, Pasma W, Kappen TH, van Wolfswinkel L, Peelen LM, et al. Relationship between preoperative evaluation blood pressure and preinduction blood pressure: a cohort study in patients undergoing general anesthesia. Anesth Analg. 2017; 124(2):431–437. PMID: 27755054.21. Kim WS, Byeon GJ, Song BJ, Lee HJ. Availability of preoperative anxiety scale as a predictive factor for hemodynamic changes during induction of anesthesia. Korean J Anesthesiol. 2010; 58(4):328–333. PMID: 20508787.22. Casadei B, Abuzeid H. Is there a strong rationale for deferring elective surgery in patients with poorly controlled hypertension? J Hypertens. 2005; 23(1):19–22. PMID: 15643117.23. Dix P, Howell S. Survey of cancellation rate of hypertensive patients undergoing anaesthesia and elective surgery. Br J Anaesth. 2001; 86(6):789–793. PMID: 11573584.24. Morrissey S, Alun-Jones T, Leighton S. Why are operations cancelled? BMJ. 1989; 299(6702):778. PMID: 2508921.25. Marcucci M, Painter TW, Conen D, Lomivorotov V, Sessler DI, Chan MTV, et al. Hypotension-avoidance versus hypertension-avoidance strategies in noncardiac surgery : an international randomized controlled trial. Ann Intern Med. 2023; 176(5):605–614. PMID: 37094336.26. Hackett NJ, De Oliveira GS, Jain UK, Kim JY. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg. 2015; 18:184–190. PMID: 25937154.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Hymn and Sutra-Chanting on the Preanesthetic Patient Anxiety in the Operating Room
- Association Between the Red Blood Cell Distribution Width and 30-Day Mortality in Intensive Care Patients Undergoing Cardiac Surgery: A Retrospective Observational Study Based on the Medical Information Mart for Intensive Care-IV Database
- The impact of preoperative coronavirus disease 19 infection on early postoperative mortality during the vaccination era: a nationwide retrospective cohort study
- Risk Assessment of Mortality Following Intraoperative Cardiac Arrest Using POSSUM and P-POSSUM in Adults Undergoing Non-Cardiac Surgery
- The Effect of Intraoperative Adjustable Suture Strabismus Surgery in Adult Strabismus Patients