Diabetes Metab J.
2024 Sep;48(5):847-863. 10.4093/dmj.2024.0237.
Artificial Light at Night and Type 2 Diabetes Mellitus
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University Changwon Hospital, Gyeongsang National University College of Medicine, Changwon, Korea
- 2Department of Epidemiology, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, Little Rock, AR, USA
- 3Winthrop P. Rockefeller Cancer Institute, University of Arkansas for Medical Sciences, Little Rock, AR, USA
- 4Epidemiology Branch, National Institute of Environmental Health Sciences, Research Triangle Park, NC, USA
- 5Division of Intramural Research, National Institute on Minority Health and Health Disparities, National Institutes of Health, Bethesda, MD, USA
- KMID: 2558996
- DOI: http://doi.org/10.4093/dmj.2024.0237
Abstract
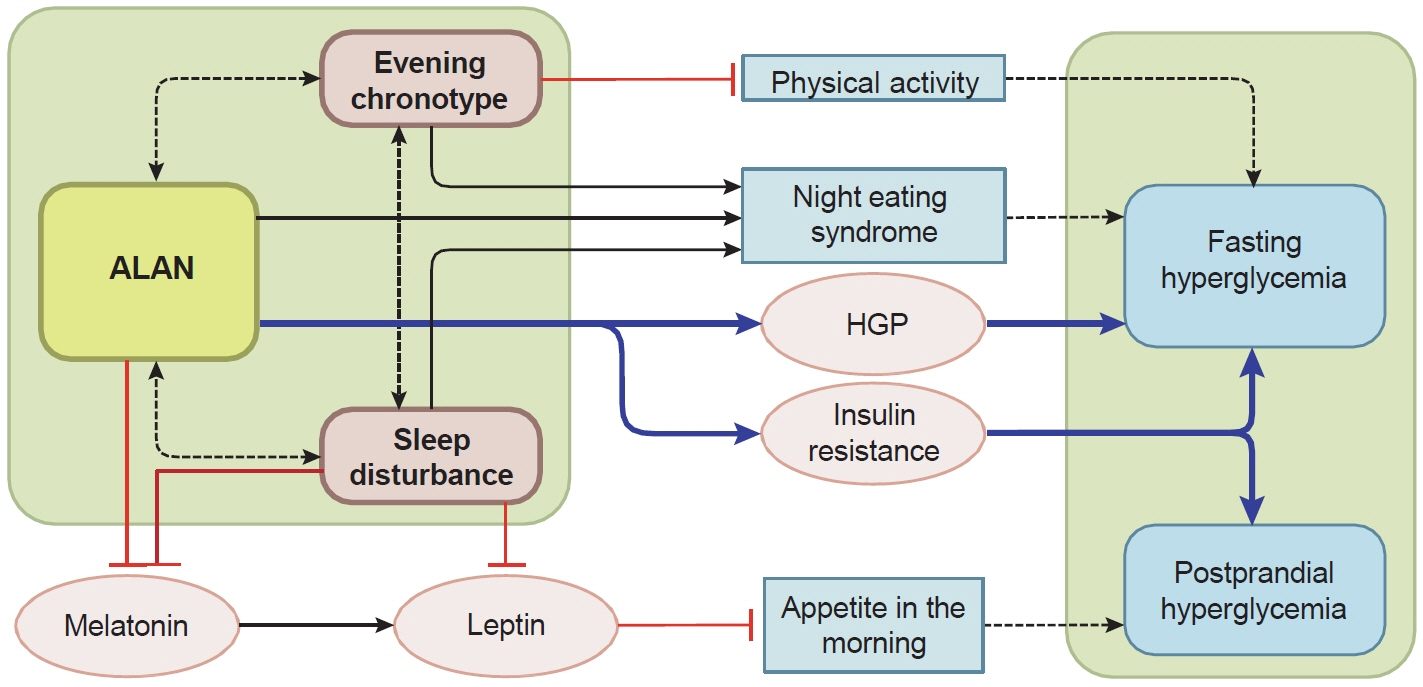
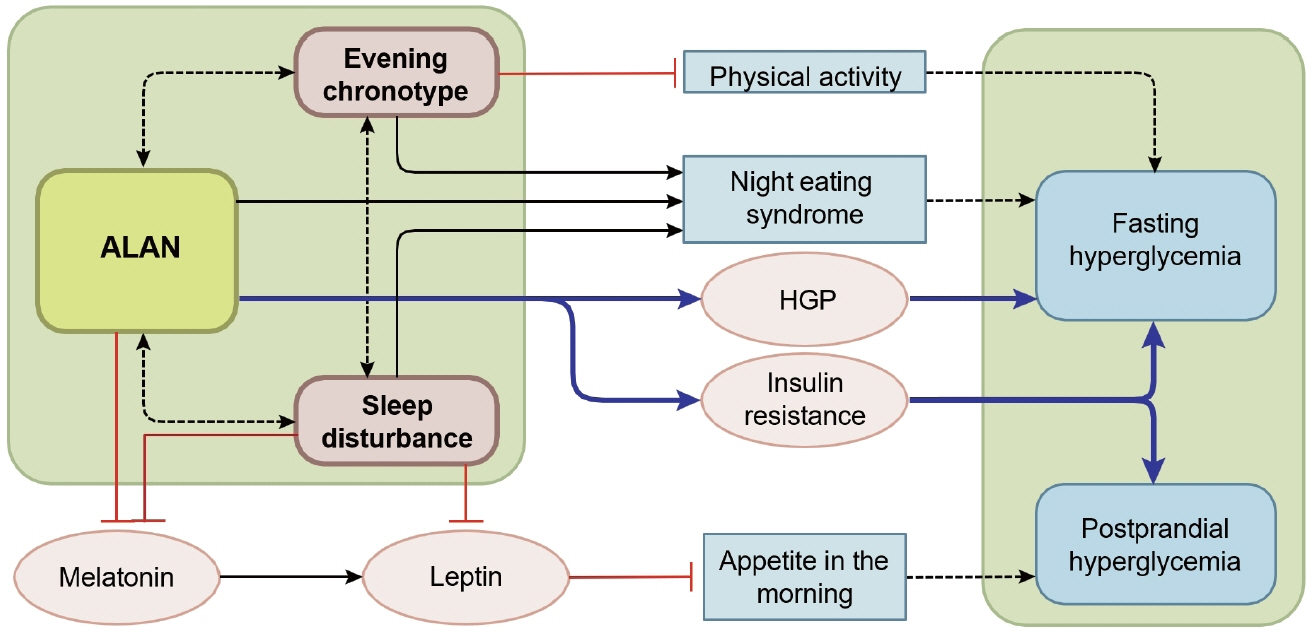
- The widespread and pervasive use of artificial light at night (ALAN) in our modern 24-hour society has emerged as a substantial disruptor of natural circadian rhythms, potentially leading to a rise in unhealthy lifestyle-related behaviors (e.g., poor sleep; shift work). This phenomenon has been associated with an increased risk of type 2 diabetes mellitus (T2DM), which is a pressing global public health concern. However, to date, reviews summarizing associations between ALAN and T2DM have primarily focused on the limited characteristics of exposure (e.g., intensity) to ALAN. This literature review extends beyond prior reviews by consolidating recent studies from 2000 to 2024 regarding associations between both indoor and outdoor ALAN exposure and the incidence or prevalence of T2DM. We also described potential biological mechanisms through which ALAN modulates glucose metabolism. Furthermore, we outlined knowledge gaps and investigated how various ALAN characteristics beyond only light intensity (including light type, timing, duration, wavelength, and individual sensitivity) influence T2DM risk. Recognizing the detrimental impact of ALAN on sleep health and the behavioral correlates of physical activity and dietary patterns, we additionally summarized studies investigating the potential mediating role of each component in the relationship between ALAN and glucose metabolism. Lastly, we proposed implications of chronotherapies and chrononutrition for diabetes management in the context of ALAN exposure.
Keyword
Figure
Reference
-
1. Lim DC, Najafi A, Afifi L, Bassetti C, Buysse DJ, Han F, et al. The need to promote sleep health in public health agendas across the globe. Lancet Public Health. 2023; 8:e820–6.
Article2. Willoughby AR, Alikhani I, Karsikas M, Chua XY, Chee MW. Country differences in nocturnal sleep variability: observations from a large-scale, long-term sleep wearable study. Sleep Med. 2023; 110:155–65.
Article3. Caraballo C, Mahajan S, Valero-Elizondo J, Massey D, Lu Y, Roy B, et al. Evaluation of temporal trends in racial and ethnic disparities in sleep duration among US adults, 2004-2018. JAMA Netw Open. 2022; 5:e226385.
Article4. Ouyang JQ, Davies S, Dominoni D. Hormonally mediated effects of artificial light at night on behavior and fitness: linking endocrine mechanisms with function. J Exp Biol. 2018; 221(Pt 6):jeb156893.
Article5. Perez Vega C, Zielinska-Dabkowska KM, Schroer S, Jechow A, Holker F. A systematic review for establishing relevant environmental parameters for urban lighting: translating research into practice. Sustainability. 2022; 14:1107.
Article6. Bonnefond A, Tassi P, Roge J, Muzet A. A critical review of techniques aiming at enhancing and sustaining worker’s alertness during the night shift. Ind Health. 2004; 42:1–14.
Article7. Gradisar M, Wolfson AR, Harvey AG, Hale L, Rosenberg R, Czeisler CA. The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 Sleep in America poll. J Clin Sleep Med. 2013; 9:1291–9.
Article8. Navara KJ, Nelson RJ. The dark side of light at night: physiological, epidemiological, and ecological consequences. J Pineal Res. 2007; 43:215–24.
Article9. Catalano F, De Vito F, Cassano V, Fiorentino TV, Sciacqua A, Hribal ML. Circadian clock desynchronization and insulin resistance. Int J Environ Res Public Health. 2022; 20:29.
Article10. Borniger JC, Maurya SK, Periasamy M, Nelson RJ. Acute dim light at night increases body mass, alters metabolism, and shifts core body temperature circadian rhythms. Chronobiol Int. 2014; 31:917–25.
Article11. Obayashi K, Saeki K, Iwamoto J, Okamoto N, Tomioka K, Nezu S, et al. Exposure to light at night, nocturnal urinary melatonin excretion, and obesity/dyslipidemia in the elderly: a cross-sectional analysis of the HEIJO-KYO study. J Clin Endocrinol Metab. 2013; 98:337–44.
Article12. Park YM, White AJ, Jackson CL, Weinberg CR, Sandler DP. Association of exposure to artificial light at night while sleeping with risk of obesity in women. JAMA Intern Med. 2019; 179:1061–71.
Article13. Davis S, Mirick DK, Stevens RG. Night shift work, light at night, and risk of breast cancer. J Natl Cancer Inst. 2001; 93:1557–62.
Article14. Muscogiuri G, Poggiogalle E, Barrea L, Tarsitano MG, Garifalos F, Liccardi A, et al. Exposure to artificial light at night: a common link for obesity and cancer? Eur J Cancer. 2022; 173:263–75.
Article15. IARC Monographs Vol 124 group. Carcinogenicity of night shift work. Lancet Oncol. 2019; 20:1058–9.16. Palomar-Cros A, Espinosa A, Bara S, de Miguel AS, Valentin A, Cirach M, et al. Exposure to artificial light-at-night and cardiometabolic health: an urban perspective from the Catalan GCAT cohort study. ISEE Conf Abstr. 2022; 2022:P0267.
Article17. Vetter C, Dashti HS, Lane JM, Anderson SG, Schernhammer ES, Rutter MK, et al. Night shift work, genetic risk, and type 2 diabetes in the UK Biobank. Diabetes Care. 2018; 41:762–9.
Article18. Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011; 8:e1001141.
Article19. Manodpitipong A, Saetung S, Nimitphong H, Siwasaranond N, Wongphan T, Sornsiriwong C, et al. Night-shift work is associated with poorer glycaemic control in patients with type 2 diabetes. J Sleep Res. 2017; 26:764–72.
Article20. Falchi F, Cinzano P, Duriscoe D, Kyba CC, Elvidge CD, Baugh K, et al. The new world atlas of artificial night sky brightness. Sci Adv. 2016; 2:e1600377.
Article21. Cinzano P, Falchi F, Elvidge CD. The first world atlas of the artificial night sky brightness. Mon Not R Astron Soc. 2001; 328:689–707.
Article22. Wang T, Kaida N, Kaida K. Effects of outdoor artificial light at night on human health and behavior: a literature review. Environ Pollut. 2023; 323:121321.
Article23. Sanchez de Miguel A, Kyba CCM, Zamorano J, Gallego J, Gaston KJ. The nature of the diffuse light near cities detected in nighttime satellite imagery. Sci Rep. 2020; 10:7829.
Article24. Sanchez de Miguel A, Bennie J, Rosenfeld E, Dzurjak S, Gaston KJ. First estimation of global trends in nocturnal power emissions reveals acceleration of light pollution. Remote Sens. 2021; 13:3311.
Article25. Holker F, Moss T, Griefahn B, Kloas W, Voigt CC, Henckel D, et al. The dark side of light: a transdisciplinary research agenda for light pollution policy. Ecol Soc. 2010; 15:13.26. Simons AL, Yin X, Longcore T. High correlation but high scale-dependent variance between satellite measured night lights and terrestrial exposure. Environ Res Commun. 2020; 2:021006.
Article27. Kyba CC, Kuester T, Sanchez de Miguel A, Baugh K, Jechow A, Holker F, et al. Artificially lit surface of earth at night increasing in radiance and extent. Sci Adv. 2017; 3:e1701528.
Article28. Kyba C, Garz S, Kuechly H, De Miguel AS, Zamorano J, Fischer J, et al. High-resolution imagery of earth at night: new sources, opportunities and challenges. Remote Sens. 2015; 7:1–23.
Article29. Zheng R, Xin Z, Li M, Wang T, Xu M, Lu J, et al. Outdoor light at night in relation to glucose homoeostasis and diabetes in Chinese adults: a national and cross-sectional study of 98,658 participants from 162 study sites. Diabetologia. 2023; 66:336–45.
Article30. Xu Z, Jin J, Yang T, Wang Y, Huang J, Pan X, et al. Outdoor light at night, genetic predisposition and type 2 diabetes mellitus: a prospective cohort study. Environ Res. 2023; 219:115157.
Article31. Sorensen TB, Wilson R, Gregson J, Shankar B, Dangour AD, Kinra S. Is night-time light intensity associated with cardiovascular disease risk factors among adults in early-stage urbanisation in South India?: a cross-sectional study of the Andhra Pradesh Children and Parents Study. BMJ Open. 2020; 10:e036213.
Article32. Klepeis NE, Nelson WC, Ott WR, Robinson JP, Tsang AM, Switzer P, et al. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Expo Anal Environ Epidemiol. 2001; 11:231–52.
Article33. Huss A, van Wel L, Bogaards L, Vrijkotte T, Wolf L, Hoek G, et al. Shedding some light in the dark: a comparison of personal measurements with satellite-based estimates of exposure to light at night among children in the Netherlands. Environ Health Perspect. 2019; 127:67001.34. Vizcaino M, Buman M, DesRoches T, Wharton C. From TVs to tablets: the relation between device-specific screen time and health-related behaviors and characteristics. BMC Public Health. 2020; 20:1295.
Article35. Mander S, Alam F, Lovreglio R, Ooi M. How to measure light pollution: a systematic review of methods and applications. Sustain Cities Soc. 2023; 92:104465.36. Obayashi K, Saeki K, Iwamoto J, Ikada Y, Kurumatani N. Independent associations of exposure to evening light and nocturnal urinary melatonin excretion with diabetes in the elderly. Chronobiol Int. 2014; 31:394–400.
Article37. Obayashi K, Yamagami Y, Kurumatani N, Saeki K. Bedroom lighting environment and incident diabetes mellitus: a longitudinal study of the HEIJO-KYO cohort. Sleep Med. 2020; 65:1–3.
Article38. Xu YX, Yu Y, Huang Y, Wan YH, Su PY, Tao FB, et al. Exposure to bedroom light pollution and cardiometabolic risk: a cohort study from Chinese young adults. Environ Pollut. 2022; 294:118628.
Article39. Windred DP, Burns AC, Rutter MK, Ching Yeung CH, Lane JM, Xiao Q, et al. Personal light exposure patterns and incidence of type 2 diabetes: analysis of 13 million hours of light sensor data and 670,000 person-years of prospective observation. Lancet Reg Health Eur. 2024; 42:100943.
Article40. Kim M, Vu TH, Maas MB, Braun RI, Wolf MS, Roenneberg T, et al. Light at night in older age is associated with obesity, diabetes, and hypertension. Sleep. 2023; 46:zsac130.
Article41. Mason IC, Grimaldi D, Reid KJ, Warlick CD, Malkani RG, Abbott SM, et al. Light exposure during sleep impairs cardiometabolic function. Proc Natl Acad Sci U S A. 2022; 119:e2113290119.
Article42. Grimaldi D, Reid K, Mason I, Warlick C, Malkani R, Abbott S, et al. Overnight light exposure acutely increases heart rate during sleep and decreases insulin sensitivity the following day. Sleep. 2021; 44(Supplement 2):A6.43. Albreiki MS, Middleton B, Hampton SM. A single night light exposure acutely alters hormonal and metabolic responses in healthy participants. Endocr Connect. 2017; 6:100–10.
Article44. Cheung IN, Zee PC, Shalman D, Malkani RG, Kang J, Reid KJ. Morning and evening blue-enriched light exposure alters metabolic function in normal weight adults. PLoS One. 2016; 11:e0155601.
Article45. Chamorro R, Wilms B, Holst A, Rohl C, Molle M, Knaak A, et al. Acute mild dim light at night slightly modifies sleep but does not affect glucose homeostasis in healthy men. Sleep Med. 2021; 84:158–64.
Article46. Harmsen JF, Wefers J, Doligkeit D, Schlangen L, Dautzenberg B, Rense P, et al. The influence of bright and dim light on substrate metabolism, energy expenditure and thermoregulation in insulin-resistant individuals depends on time of day. Diabetologia. 2022; 65:721–32.
Article47. Lee DY, Jung I, Park SY, Yu JH, Seo JA, Kim KJ, et al. Attention to innate circadian rhythm and the impact of its disruption on diabetes. Diabetes Metab J. 2024; 48:37–52.
Article48. Fonken LK, Nelson RJ. The effects of light at night on circadian clocks and metabolism. Endocr Rev. 2014; 35:648–70.
Article49. Schwartz WJ, Tavakoli-Nezhad M, Lambert CM, Weaver DR, de la Iglesia HO. Distinct patterns of Period gene expression in the suprachiasmatic nucleus underlie circadian clock photoentrainment by advances or delays. Proc Natl Acad Sci U S A. 2011; 108:17219–24.50. Bonmati-Carrion MA, Arguelles-Prieto R, Martinez-Madrid MJ, Reiter R, Hardeland R, Rol MA, et al. Protecting the melatonin rhythm through circadian healthy light exposure. Int J Mol Sci. 2014; 15:23448–500.
Article51. Pandi-Perumal SR, Smits M, Spence W, Srinivasan V, Cardinali DP, Lowe AD, et al. Dim light melatonin onset (DLMO): a tool for the analysis of circadian phase in human sleep and chronobiological disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2007; 31:1–11.
Article52. Stenvers DJ, Scheer FA, Schrauwen P, la Fleur SE, Kalsbeek A. Circadian clocks and insulin resistance. Nat Rev Endocrinol. 2019; 15:75–89.
Article53. Garaulet M, Qian J, Florez JC, Arendt J, Saxena R, Scheer FA. Melatonin effects on glucose metabolism: time to unlock the controversy. Trends Endocrinol Metab. 2020; 31:192–204.
Article54. Cho Y, Ryu SH, Lee BR, Kim KH, Lee E, Choi J. Effects of artificial light at night on human health: a literature review of observational and experimental studies applied to exposure assessment. Chronobiol Int. 2015; 32:1294–310.
Article55. Haim A, Zubidat AE. Artificial light at night: melatonin as a mediator between the environment and epigenome. Philos Trans R Soc Lond B Biol Sci. 2015; 370:20140121.
Article56. Gilbert ER, Liu D. Epigenetics: the missing link to understanding β-cell dysfunction in the pathogenesis of type 2 diabetes. Epigenetics. 2012; 7:841–52.
Article57. Delpino FM, Figueiredo LM, Nunes BP. Effects of melatonin supplementation on diabetes: a systematic review and meta-analysis of randomized clinical trials. Clin Nutr. 2021; 40:4595–605.
Article58. Ostadmohammadi V, Soleimani A, Bahmani F, Aghadavod E, Ramezani R, Reiter RJ, et al. The effects of melatonin supplementation on parameters of mental health, glycemic control, markers of cardiometabolic risk, and oxidative stress in diabetic hemodialysis patients: a randomized, double-blind, placebo-controlled trial. J Ren Nutr. 2020; 30:242–50.
Article59. Peschke E, Bahr I, Muhlbauer E. Melatonin and pancreatic islets: interrelationships between melatonin, insulin and glucagon. Int J Mol Sci. 2013; 14:6981–7015.
Article60. Qian J, Block GD, Colwell CS, Matveyenko AV. Consequences of exposure to light at night on the pancreatic islet circadian clock and function in rats. Diabetes. 2013; 62:3469–78.
Article61. Qian J, Yeh B, Rakshit K, Colwell CS, Matveyenko AV. Circadian disruption and diet-induced obesity synergize to promote development of β-cell failure and diabetes in male rats. Endocrinology. 2015; 156:4426–36.
Article62. Pechanova O, Paulis L, Simko F. Peripheral and central effects of melatonin on blood pressure regulation. Int J Mol Sci. 2014; 15:17920–37.63. Meng JJ, Shen JW, Li G, Ouyang CJ, Hu JX, Li ZS, et al. Light modulates glucose metabolism by a retina-hypothalamus-brown adipose tissue axis. Cell. 2023; 186:398–412.
Article64. Opperhuizen AL, Stenvers DJ, Jansen RD, Foppen E, Fliers E, Kalsbeek A. Light at night acutely impairs glucose tolerance in a time-, intensity- and wavelength-dependent manner in rats. Diabetologia. 2017; 60:1333–43.
Article65. Elovainio M, Komulainen K, Lipsanen J, Partonen T, Pesonen AK, Pulkki-Raback L, et al. Long-term cumulative light exposure from the natural environment and sleep: a cohort study. J Sleep Res. 2022; 31:e13511.
Article66. Green A, Cohen-Zion M, Haim A, Dagan Y. Comparing the response to acute and chronic exposure to short wavelength lighting emitted from computer screens. Chronobiol Int. 2018; 35:90–100.
Article67. Chang AM, Scheer FA, Czeisler CA. The human circadian system adapts to prior photic history. J Physiol. 2011; 589(Pt 5)(Pt 5):1095–102.
Article68. Brainard GC, Hanifin JP, Greeson JM, Byrne B, Glickman G, Gerner E, et al. Action spectrum for melatonin regulation in humans: evidence for a novel circadian photoreceptor. J Neurosci. 2001; 21:6405–12.
Article69. Brainard GC, Sliney D, Hanifin JP, Glickman G, Byrne B, Greeson JM, et al. Sensitivity of the human circadian system to short-wavelength (420-nm) light. J Biol Rhythms. 2008; 23:379–86.
Article70. Bauer M, Glenn T, Monteith S, Gottlieb JF, Ritter PS, Geddes J, et al. The potential influence of LED lighting on mental illness. World J Biol Psychiatry. 2018; 19:59–73.
Article71. Nagai N, Ayaki M, Yanagawa T, Hattori A, Negishi K, Mori T, et al. Suppression of blue light at night ameliorates metabolic abnormalities by controlling circadian rhythms. Invest Ophthalmol Vis Sci. 2019; 60:3786–93.
Article72. Ayaki M, Hattori A, Maruyama Y, Nakano M, Yoshimura M, Kitazawa M, et al. Protective effect of blue-light shield eyewear for adults against light pollution from self-luminous devices used at night. Chronobiol Int. 2016; 33:134–9.
Article73. Allen AE, Hazelhoff EM, Martial FP, Cajochen C, Lucas RJ. Exploiting metamerism to regulate the impact of a visual display on alertness and melatonin suppression independent of visual appearance. Sleep. 2018; 41:zsy100.
Article74. Brown TM, Brainard GC, Cajochen C, Czeisler CA, Hanifin JP, Lockley SW, et al. Recommendations for daytime, evening, and nighttime indoor light exposure to best support physiology, sleep, and wakefulness in healthy adults. PLoS Biol. 2022; 20:e3001571.
Article75. Phillips AJ, Vidafar P, Burns AC, McGlashan EM, Anderson C, Rajaratnam SM, et al. High sensitivity and interindividual variability in the response of the human circadian system to evening light. Proc Natl Acad Sci U S A. 2019; 116:12019–24.
Article76. Cain SW, McGlashan EM, Vidafar P, Mustafovska J, Curran SP, Wang X, et al. Evening home lighting adversely impacts the circadian system and sleep. Sci Rep. 2020; 10:19110.
Article77. Duffy JF, Zeitzer JM, Czeisler CA. Decreased sensitivity to phase-delaying effects of moderate intensity light in older subjects. Neurobiol Aging. 2007; 28:799–807.
Article78. Gabel V, Reichert CF, Maire M, Schmidt C, Schlangen LJ, Kolodyazhniy V, et al. Differential impact in young and older individuals of blue-enriched white light on circadian physiology and alertness during sustained wakefulness. Sci Rep. 2017; 7:7620.
Article79. Khalsa SB, Jewett ME, Cajochen C, Czeisler CA. A phase response curve to single bright light pulses in human subjects. J Physiol. 2003; 549(Pt 3):945–52.
Article80. Morris CJ, Yang JN, Garcia JI, Myers S, Bozzi I, Wang W, et al. Endogenous circadian system and circadian misalignment impact glucose tolerance via separate mechanisms in humans. Proc Natl Acad Sci U S A. 2015; 112:E2225–34.
Article81. Phipps-Nelson J, Redman JR, Dijk DJ, Rajaratnam SM. Daytime exposure to bright light, as compared to dim light, decreases sleepiness and improves psychomotor vigilance performance. Sleep. 2003; 26:695–700.
Article82. Cyr M, Artenie DZ, Al Bikaii A, Borsook D, Olson JA. The effect of evening light on circadian-related outcomes: a systematic review. Sleep Med Rev. 2022; 64:101660.
Article83. Chang AM, Santhi N, St Hilaire M, Gronfier C, Bradstreet DS, Duffy JF, et al. Human responses to bright light of different durations. J Physiol. 2012; 590:3103–12.
Article84. McIntyre IM, Norman TR, Burrows GD, Armstrong SM. Quantal melatonin suppression by exposure to low intensity light in man. Life Sci. 1989; 45:327–32.
Article85. Xiao Q, Lyu Y, Zhou M, Lu J, Zhang K, Wang J, et al. Artificial light at night and social vulnerability: an environmental justice analysis in the U.S. 2012-2019. Environ Int. 2023; 178:108096.
Article86. Sweeney MR, Nichols HB, Jones RR, Olshan AF, Keil AP, Engel LS, et al. Exposure to indoor light at night in relation to multiple dimensions of sleep health: findings from the Sister Study. Sleep. 2024; 47:zsad100.
Article87. Xiao Q, Gee G, Jones RR, Jia P, James P, Hale L. Cross-sectional association between outdoor artificial light at night and sleep duration in middle-to-older aged adults: the NIH-AARP Diet and Health Study. Environ Res. 2020; 180:108823.
Article88. Xu YX, Zhang JH, Tao FB, Sun Y. Association between exposure to light at night (LAN) and sleep problems: a systematic review and meta-analysis of observational studies. Sci Total Environ. 2023; 857(Pt 1):159303.
Article89. Heo JY, Kim K, Fava M, Mischoulon D, Papakostas GI, Kim MJ, et al. Effects of smartphone use with and without blue light at night in healthy adults: a randomized, double-blind, cross-over, placebo-controlled comparison. J Psychiatr Res. 2017; 87:61–70.
Article90. Chen GC, Liu MM, Chen LH, Xu JY, Hidayat K, Li FR, et al. Daytime napping and risk of type 2 diabetes: a meta-analysis of prospective studies. Sleep Breath. 2018; 22:815–24.
Article91. McWhorter KL, Park YM, Gaston SA, Fang KB, Sandler DP, Jackson CL. Multiple sleep dimensions and type 2 diabetes risk among women in the Sister Study: differences by race/ethnicity. BMJ Open Diabetes Res Care. 2019; 7:e000652.
Article92. Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010; 33:414–20.93. Lee SWH, Ng KY, Chin WK. The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: a systematic review and meta-analysis. Sleep Med Rev. 2017; 31:91–101.
Article94. Klingenberg L, Chaput JP, Holmback U, Visby T, Jennum P, Nikolic M, et al. Acute sleep restriction reduces insulin sensitivity in adolescent boys. Sleep. 2013; 36:1085–90.
Article95. Li Y, Gao X, Winkelman JW, Cespedes EM, Jackson CL, Walters AS, et al. Association between sleeping difficulty and type 2 diabetes in women. Diabetologia. 2016; 59:719–27.
Article96. Buxton OM, Cain SW, O’Connor SP, Porter JH, Duffy JF, Wang W, et al. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med. 2012; 4:129ra43.
Article97. Yuan RK, Zitting KM, Duffy JF, Vujovic N, Wang W, Quan SF, et al. Chronic sleep restriction while minimizing circadian disruption does not adversely affect glucose tolerance. Front Physiol. 2021; 12:764737.
Article98. Leproult R, Holmback U, Van Cauter E. Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes. 2014; 63:1860–9.
Article99. Gil-Lozano M, Hunter PM, Behan LA, Gladanac B, Casper RF, Brubaker PL. Short-term sleep deprivation with nocturnal light exposure alters time-dependent glucagon-like peptide-1 and insulin secretion in male volunteers. Am J Physiol Endocrinol Metab. 2016; 310:E41–50.
Article100. Albrecht U. Timing to perfection: the biology of central and peripheral circadian clocks. Neuron. 2012; 74:246–60.
Article101. Barkley JE, Lepp A. Mobile phone use among college students is a sedentary leisure behavior which may interfere with exercise. Comput Human Behav. 2016; 56:29–33.
Article102. Atkinson G, Fullick S, Grindey C, Maclaren D. Exercise, energy balance and the shift worker. Sports Med. 2008; 38:671–85.
Article103. Fonken LK, Workman JL, Walton JC, Weil ZM, Morris JS, Haim A, et al. Light at night increases body mass by shifting the time of food intake. Proc Natl Acad Sci U S A. 2010; 107:18664–9.
Article104. Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring). 2011; 19:1374–81.
Article105. Baron KG, Reid KJ, Horn LV, Zee PC. Contribution of evening macronutrient intake to total caloric intake and body mass index. Appetite. 2013; 60:246–51.
Article106. Fonken LK, Melendez-Fernandez OH, Weil ZM, Nelson RJ. Exercise attenuates the metabolic effects of dim light at night. Physiol Behav. 2014; 124:33–6.
Article107. Touitou Y, Reinberg A, Touitou D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: health impacts and mechanisms of circadian disruption. Life Sci. 2017; 173:94–106.
Article108. Lunn RM, Blask DE, Coogan AN, Figueiro MG, Gorman MR, Hall JE, et al. Health consequences of electric lighting practices in the modern world: a report on the National Toxicology Program’s workshop on shift work at night, artificial light at night, and circadian disruption. Sci Total Environ. 2017; 607-608:1073–84.
Article109. Fujimoto R, Ohta Y, Masuda K, Taguchi A, Akiyama M, Yamamoto K, et al. Metabolic state switches between morning and evening in association with circadian clock in people without diabetes. J Diabetes Investig. 2022; 13:1496–505.
Article110. Cailotto C, Lei J, van der Vliet J, van Heijningen C, van Eden CG, Kalsbeek A, et al. Effects of nocturnal light on (clock) gene expression in peripheral organs: a role for the autonomic innervation of the liver. PLoS One. 2009; 4:e5650.
Article111. Peng F, Li X, Xiao F, Zhao R, Sun Z. Circadian clock, diurnal glucose metabolic rhythm, and dawn phenomenon. Trends Neurosci. 2022; 45:471–82.
Article112. Versteeg RI, Stenvers DJ, Visintainer D, Linnenbank A, Tanck MW, Zwanenburg G, et al. Acute effects of morning light on plasma glucose and triglycerides in healthy men and men with type 2 diabetes. J Biol Rhythms. 2017; 32:130–42.
Article113. Adeghate E, Lotfy M, D’Souza C, Alseiari SM, Alsaadi AA, Qahtan SA. Hypocretin/orexin modulates body weight and the metabolism of glucose and insulin. Diabetes Metab Res Rev. 2020; 36:e3229.
Article114. Tsuneki H, Wada T, Sasaoka T. Role of orexin in the central regulation of glucose and energy homeostasis. Endocr J. 2012; 59:365–74.
Article115. Kalsbeek A, Scheer FA, Perreau-Lenz S, La Fleur SE, Yi CX, Fliers E, et al. Circadian disruption and SCN control of energy metabolism. FEBS Lett. 2011; 585:1412–26.
Article116. Lopez-Prieto RS, Romo-Romo A, Gomez-Aviles P, Sharma-Sharma S, Costilla-Orozco X, Galan-Ramirez GA, et al. Time matters: an insight into the relationship between chrononutrition and diabetes. Rev Invest Clin. 2024; 76:080–090.117. Franzago M, Alessandrelli E, Notarangelo S, Stuppia L, Vitacolonna E. Chrono-nutrition: circadian rhythm and personalized nutrition. Int J Mol Sci. 2023; 24:2571.
Article118. Heber D, Li Z, Ordovas J. Precision nutrition. Amsterdam: Academic Press; 2023. Chapter 3, The use of chrono nutrition in precision nutrition; p43-60 [cited 2024 Aug 28]. Available from: https://www.sciencedirect.com/science/article/abs/pii/B9780443153150000146.119. Kashyap S, Bala R, Behl T. Understanding the concept of chronotherapeutics in the management of diabetes mellitus. Curr Diabetes Rev. 2021; 17:e221020187106.
Article120. Amiama-Roig A, Verdugo-Sivianes EM, Carnero A, Blanco JR. Chronotherapy: circadian rhythms and their influence in cancer therapy. Cancers (Basel). 2022; 14:5071.
Article121. Turk D, Scherer N, Selzer D, Dings C, Hanke N, Dallmann R, et al. Significant impact of time-of-day variation on metformin pharmacokinetics. Diabetologia. 2023; 66:1024–34.
Article122. Meule A, Roeser K, Randler C, Kubler A. Skipping breakfast: morningness-eveningness preference is differentially related to state and trait food cravings. Eat Weight Disord. 2012; 17:e304–8.123. Nelson RJ, Chbeir S. Dark matters: effects of light at night on metabolism. Proc Nutr Soc. 2018; 77:223–9.
Article124. Allison KC, Spaeth A, Hopkins CM. Sleep and eating disorders. Curr Psychiatry Rep. 2016; 18:92.
Article125. Riccobono G, Iannitelli A, Pompili A, Iorio C, Stratta P, Rossi R, et al. Night eating syndrome, circadian rhythms and seasonality: a study in a population of Italian university students. Riv Psichiatr. 2020; 55:47–52.126. Martin JS, Hebert M, Ledoux E, Gaudreault M, Laberge L. Relationship of chronotype to sleep, light exposure, and work-related fatigue in student workers. Chronobiol Int. 2012; 29:295–304.
Article127. Blume C, Garbazza C, Spitschan M. Effects of light on human circadian rhythms, sleep and mood. Somnologie (Berl). 2019; 23:147–56.
Article128. Albreiki MS, Shamlan GH, BaHammam AS, Alruwaili NW, Middleton B, Hampton SM. Acute impact of light at night and exogenous melatonin on subjective appetite and plasma leptin. Front Nutr. 2022; 9:1079453.
Article129. Kelesidis T, Kelesidis I, Chou S, Mantzoros CS. Narrative review: the role of leptin in human physiology: emerging clinical applications. Ann Intern Med. 2010; 152:93–100.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Dim Artificial Light at Night (dALAN) Exposure during Sleep on Human Fatigue
- Artificial Pancreas: A Concise Review
- A Case of Insulinoma Associated with Type 2 Diabetes Mellitus
- Progressive Decline of beta-cell Function in Type 2 Diabetes Mellitus
- Genetic Diseases Associated with Diabetes Mellitus