Ann Surg Treat Res.
2024 Sep;107(3):178-185. 10.4174/astr.2024.107.3.178.
The outcomes of component separation technique versus no component separation technique in the repair of large ventral hernias and impact on quality of life: a multicenter retrospective cohort study
- Affiliations
-
- 1Department of General Surgery, Hınıs Şehit Yavuz Yürekseven State Hospital, Erzurum, Turkiye
- 2Department of General Surgery, Koç University School of Medicine, Istanbul, Turkiye
- 3Department of General Surgery, Sancaktepe Sehit Prof. Dr. Ilhan Varank Research and Education Hospital, Istanbul, Turkiye
- KMID: 2558992
- DOI: http://doi.org/10.4174/astr.2024.107.3.178
Abstract
- Purpose
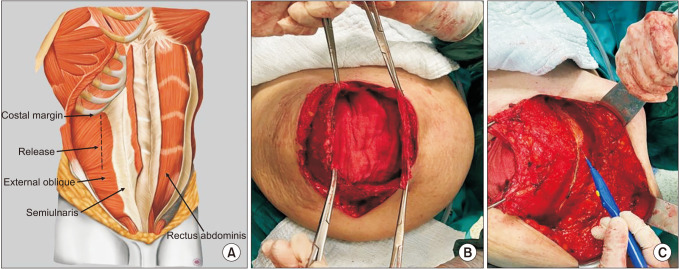
This study aimed to compare the results of patients who underwent anterior component separation techniques (ACST) and those who did not undergo component separation techniques (non-CST) in complicated ventral hernia repairs (VHRs) and to investigate the effect of these techniques on quality of life (QoL).
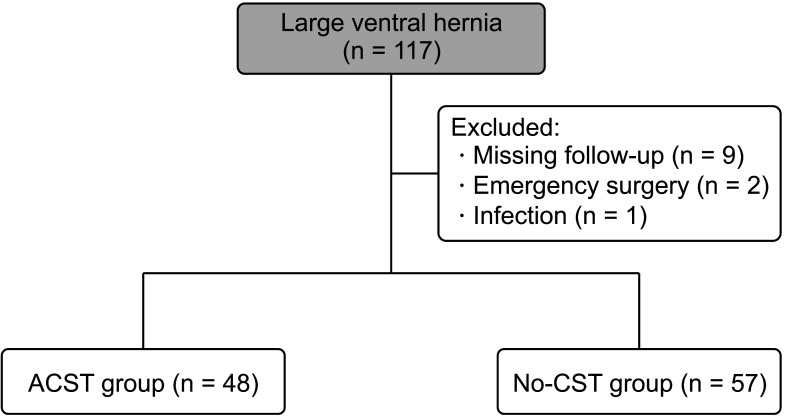
Methods
A total of 105 patients who were operated for large ventral hernias were retrospectively analyzed. The patients were divided into the ACST group (n = 48) and the non-CST group (n = 57). Demographic, intraoperative, and postoperative data were recorded. Postoperative follow-up was conducted at 2 and 4 weeks, and 6, 12, and 24 months. The primary and secondary outcomes and QoL were measured.
Results
The female ratio was higher in both groups (P = 0.512). There was no significant difference between age and body mass index between the groups (P = 0.705 and P = 0.803). The mean defect size and mesh size were similar between the groups (P = 0.775 and P = 0.245). The mean operation duration and amount of blood loss were similar between the groups (P = 0.801 and P = 0.142). There was no statistically significant difference in the median visual analog scale scores between the groups (P = 0.551). During follow-up, only 3 patients (6.3%) in the ACST group and 4 patients (7.0%) in the non-CST group had recurrence. There was no significant difference in the short- and long-term QoL between the groups.
Conclusion
The ACST is a feasible surgical option for patients with complicated VHRs. In addition, by improving QoL, the recurrence rate is similar to patients undergoing standard VHR.
Figure
Reference
-
1. Poulose BK, Shelton J, Phillips S, Moore D, Nealon W, Penson D, et al. Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia. 2012; 16:179–183. PMID: 21904861.2. Slater NJ, Montgomery A, Berrevoet F, Carbonell AM, Chang A, Franklin M, et al. Criteria for definition of a complex abdominal wall hernia. Hernia. 2014; 18:7–17. PMID: 24150721.3. Topcu R. Component separation technique in incisional hernias. Kafadar MT, Gok MA, editors. Hernia surgery. Akademisyen Kitabevi;2020. p. 159–179.4. Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004; 240:578–585. PMID: 15383785.5. den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW. Open surgical procedures for incisional hernias. Cochrane Database Syst Rev. 2008; 2008:CD006438. PMID: 18646155.6. Booth JH, Garvey PB, Baumann DP, Selber JC, Nguyen AT, Clemens MW, et al. Primary fascial closure with mesh reinforcement is superior to bridged mesh repair for abdominal wall reconstruction. J Am Coll Surg. 2013; 217:999–1009. PMID: 24083910.7. Holihan JL, Askenasy EP, Greenberg JA, Keith JN, Martindale RG, Roth JS, et al. Component separation vs. bridged repair for large ventral hernias: a multi-institutional risk-adjusted comparison, systematic review, and meta-analysis. Surg Infect (Larchmt). 2016; 17:17–26. PMID: 26375422.8. Ramirez OM, Ruas E, Dellon AL. “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg. 1990; 86:519–526. PMID: 2143588.9. Cobb WS, Warren JA, Ewing JA, Burnikel A, Merchant M, Carbonell AM. Open retromuscular mesh repair of complex incisional hernia: predictors of wound events and recurrence. J Am Coll Surg. 2015; 220:606–613. PMID: 25797746.10. Maloney SR, Schlosser KA, Prasad T, Kasten KR, Gersin KS, Colavita PD, et al. Twelve years of component separation technique in abdominal wall reconstruction. Surgery. 2019; 166:435–444. PMID: 31358348.11. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.12. Heniford BT, Lincourt AE, Walters AL, Colavita PD, Belyansky I, Kercher KW, et al. Carolinas Comfort Scale as a measure of hernia repair quality of life: a reappraisal utilizing 3788 international patients. Ann Surg. 2018; 267:171–176. PMID: 27655239.13. Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW. Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg. 2008; 206:638–644. PMID: 18387468.14. Cox TC, Huntington CR, Blair LJ, Prasad T, Lincourt AE, Heniford BT, et al. Predictive modeling for chronic pain after ventral hernia repair. Am J Surg. 2016; 212:501–510. PMID: 27443426.15. Colavita PD, Tsirline VB, Belyansky I, Walters AL, Lincourt AE, Sing RF, et al. Prospective, long-term comparison of quality of life in laparoscopic versus open ventral hernia repair. Ann Surg. 2012; 256:714–723. PMID: 23095614.16. Jensen KK, Arnesen RB, Christensen JK, Bisgaard T, Jørgensen LN. Large incisional hernias increase in size. J Surg Res. 2019; 244:160–165. PMID: 31295649.17. Shestak KC, Edington HJ, Johnson RR. The separation of anatomic components technique for the reconstruction of massive midline abdominal wall defects: anatomy, surgical technique, applications, and limitations revisited. Plast Reconstr Surg. 2000; 105:731–738. PMID: 10697187.18. Petersen S, Henke G, Zimmermann L, Aumann G, Hellmich G, Ludwig K. Ventral rectus fascia closure on top of mesh hernia repair in the sublay technique. Plast Reconstr Surg. 2004; 114:1754–1760. PMID: 15577345.19. Clarke JM. Incisional hernia repair by fascial component separation: results in 128 cases and evolution of technique. Am J Surg. 2010; 200:2–8. PMID: 20637331.20. Cornette B, De Bacquer D, Berrevoet F. Component separation technique for giant incisional hernia: a systematic review. Am J Surg. 2018; 215:719–726. PMID: 28811004.21. Mazzocchi M, Dessy LA, Ranno R, Carlesimo B, Rubino C. “Component separation” technique and panniculectomy for repair of incisional hernia. Am J Surg. 2011; 201:776–783. PMID: 20850707.22. Klima DA, Brintzenhoff RA, Tsirline VB, Belyansky I, Lincourt AE, Getz S, et al. Application of subcutaneous talc in hernia repair and wide subcutaneous dissection dramatically reduces seroma formation and postoperative wound complications. Am Surg. 2011; 77:888–894. PMID: 21944353.23. Giurgius M, Bendure L, Davenport DL, Roth JS. The endoscopic component separation technique for hernia repair results in reduced morbidity compared to the open component separation technique. Hernia. 2012; 16:47–51. PMID: 21833851.24. Krpata DM, Blatnik JA, Novitsky YW, Rosen MJ. Posterior and open anterior components separations: a comparative analysis. Am J Surg. 2012; 203:318–322. PMID: 22244073.25. Archer S, Pinto A, Vuik S, Bicknell C, Faiz O, Byrne B, et al. Surgery, complications, and quality of life: a longitudinal cohort study exploring the role of psychosocial factors. Ann Surg. 2019; 270:95–101. PMID: 29677027.26. Blair LJ, Cox TC, Huntington CR, Groene SA, Prasad T, Lincourt AE, et al. The effect of component separation technique on quality of life (QOL) and surgical outcomes in complex open ventral hernia repair (OVHR). Surg Endosc. 2017; 31:3539–3546. PMID: 28039655.27. Klima DA, Tsirline VB, Belyansky I, Dacey KT, Lincourt AE, Kercher KW, et al. Quality of life following component separation versus standard open ventral hernia repair for large hernias. Surg Innov. 2014; 21:147–154. PMID: 23843156.28. Köckerling F. Recurrent incisional hernia repair: an overview. Front Surg. 2019; 6:26. PMID: 31139632.29. Sailes FC, Walls J, Guelig D, Mirzabeigi M, Long WD, Crawford A, et al. Synthetic and biological mesh in component separation: a 10-year single institution review. Ann Plast Surg. 2010; 64:696–698. PMID: 20395790.