Arch Hand Microsurg.
2024 Sep;29(3):154-162. 10.12790/ahm.24.0028.
Intra-articular fracture reduction: a comparative observational study of clinical results after the surgical treatment of distal radius fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, Inseong Medical Foundation Hallym Hospital, Incheon, Korea
- 2Department of Orthopedic Surgery, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2558739
- DOI: http://doi.org/10.12790/ahm.24.0028
Abstract
- Purpose
This study compared the outcomes of intra-articular fracture reduction for distal radius fractures.
Methods
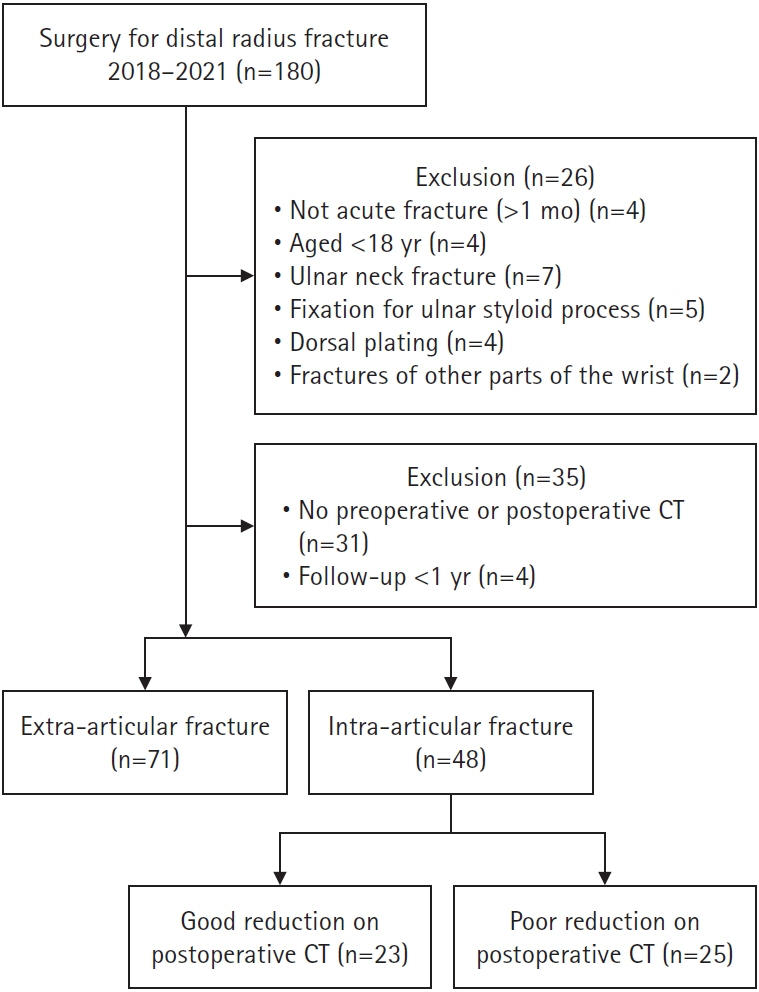
Among 180 patients who underwent open reduction and plate fixation, the exclusion criteria were as follows: non-acute fracture (>1 month), an accompanying ulnar neck fracture, a distal ulnar fracture requiring fixation, fixation through the dorsal approach, other accompanying hand fractures, the absence of preoperative or postoperative computed tomography (CT), and follow-up for <1 year. Intra-articular fractures were evaluated through CT. Forty-eight patients with intra-articular fractures were studied. Displaced intra-articular fractures were defined as: (1) articular step-off ≥1 mm, (2) fracture gap ≥2 mm, or (3) gross incongruence. Reduction was classified as good (n=23) or poor (n=25) based on postoperative CT. The pain visual analogue scale (pVAS), the quick Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire, and range of motion of the wrist joint were compared between both groups.
Results
No significant between-group differences were found in the preoperative demographic data and the postoperative pVAS and quick DASH scores (pVAS: 0.6 vs. 0.8 and quick DASH: 9.4 vs. 10.2 in the good vs. poor reduction groups, respectively). However, the flexion-extension arc was significantly restricted in the poor reduction group (162° in the good reduction group vs. 146° in the poor reduction group, p<0.001).
Conclusion
The reduction of the articular surface was not related to pain and functional results at the mid-term follow-up after the surgical treatment of intra-articular distal radius fractures. However, insufficient fracture reduction affected the postoperative range of motion.
Keyword
Figure
Reference
-
References
1. Rundgren J, Bojan A, Mellstrand Navarro C, Enocson A. Epidemiology, classification, treatment and mortality of distal radius fractures in adults: an observational study of 23,394 fractures from the national Swedish fracture register. BMC Musculoskelet Disord. 2020; 21:88.
Article2. Koo OT, Tan DM, Chong AK. Distal radius fractures: an epidemiological review. Orthop Surg. 2013; 5:209–13.
Article3. Müller ME, Schneider R, Willenegger H. Manual of internal fixation: techniques recommended by the AO-ASIF group. 3rd ed. Heidelberg: Springer Science & Business Media;2013.4. Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986; 68:647–59.
Article5. Thiart M, Ikram A, Lamberts RP. How well can step-off and gap distances be reduced when treating intra-articular distal radius fractures with fragment specific fixation when using fluoroscopy. Orthop Traumatol Surg Res. 2016; 102:1001–4.
Article6. Edwards CC, Haraszti CJ, McGillivary GR, Gutow AP. Intra-articular distal radius fractures: arthroscopic assessment of radiographically assisted reduction. J Hand Surg Am. 2001; 26:1036–41.7. Giannoudis PV, Tzioupis C, Papathanassopoulos A, Obakponovwe O, Roberts C. Articular step-off and risk of post-traumatic osteoarthritis. Evidence today. Injury. 2010; 41:986–95.
Article8. Gruber G, Zacherl M, Giessauf C, et al. Quality of life after volar plate fixation of articular fractures of the distal part of the radius. J Bone Joint Surg Am. 2010; 92:1170–8.
Article9. Van Son MA, De Vries J, Roukema JA, Den Oudsten BL. Health status and (health-related) quality of life during the recovery of distal radius fractures: a systematic review. Qual Life Res. 2013; 22:2399–416.
Article10. Lameijer CM, Ten Duis HJ, Dusseldorp IV, Dijkstra PU, van der Sluis CK. Prevalence of posttraumatic arthritis and the association with outcome measures following distal radius fractures in non-osteoporotic patients: a systematic review. Arch Orthop Trauma Surg. 2017; 137:1499–513.
Article11. Doi K, Hattori Y, Otsuka K, Abe Y, Yamamoto H. Intra-articular fractures of the distal aspect of the radius: arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am. 1999; 81:1093–110.12. Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg Am. 1991; 16:375–84.
Article13. Kodama N, Takemura Y, Ueba H, Imai S, Matsusue Y. Acceptable parameters for alignment of distal radius fracture with conservative treatment in elderly patients. J Orthop Sci. 2014; 19:292–7.14. Park MJ, Koh KH, Lee KW, Lee YJ, Lee HI. Patient-perceived outcomes after nonoperative treatment of distal radius fracture in older adults. Orthopedics. 2021; 44:e190–6.
Article15. Forward DP, Davis TR, Sithole JS. Do young patients with malunited fractures of the distal radius inevitably develop symptomatic post-traumatic osteoarthritis? J Bone Joint Surg Br. 2008; 90:629–37.
Article16. Lutz M, Arora R, Krappinger D, Wambacher M, Rieger M, Pechlaner S. Arthritis predicting factors in distal intraarticular radius fractures. Arch Orthop Trauma Surg. 2011; 131:1121–6.
Article17. Ryu JY, Cooney WP, Askew LJ, An KN, Chao EY. Functional ranges of motion of the wrist joint. J Hand Surg Am. 1991; 16:409–19.
Article18. Brigstocke G, Hearnden A, Holt CA, Whatling G. The functional range of movement of the human wrist. J Hand Surg Eur Vol. 2013; 38:554–6.
Article19. Kim SJ, Lee BG, Lee CH, Choi WS, Kim JH, Lee KH. Comparison of ceiling effects between two patient-rating scores and a physician-rating score in the assessment of outcome after the surgical treatment of distal radial fractures. Bone Joint J. 2015; 97-B:1651–6.20. Lameijer CM, Ten Duis HJ, Vroling D, Hartlief MT, El Moumni M, van der Sluis CK. Prevalence of posttraumatic arthritis following distal radius fractures in non-osteoporotic patients and the association with radiological measurements, clinician and patient-reported outcomes. Arch Orthop Trauma Surg. 2018; 138:1699–712.
Article21. Tariq H, Collins K, Tait D, Dunn J, Altaf S, Porter S. Factors associated with joint contractures in adults: a systematic review with narrative synthesis. Disabil Rehabil. 2023; 45:1755–72.
Article22. Baratz ME, Des Jardins Jd, Anderson DD, Imbriglia JE. Displaced intra-articular fractures of the distal radius: the effect of fracture displacement on contact stresses in a cadaver model. J Hand Surg Am. 1996; 21:183–8.23. Song HS, Yoon HM. Pathophysiology of stiff elbow. Clin Shoulder Elb. 2010; 13:286–92.
Article24. Karnezis IA, Panagiotopoulos E, Tyllianakis M, Megas P, Lambiris E. Correlation between radiological parameters and patient-rated wrist dysfunction following fractures of the distal radius. Injury. 2005; 36:1435–9.25. Lutz M, Rudisch A, Kralinger F, et al. Sagittal wrist motion of carpal bones following intraarticular fractures of the distal radius. J Hand Surg Br. 2005; 30:282–7.
Article26. Berner SH, Willis FB. Dynamic splinting in wrist extension following distal radius fractures. J Orthop Surg Res. 2010; 5:53.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of the distal radius fractures with open reduction and internal fixation
- Clinical Study of Intra-articular Fracture of Distal Radius
- Clinical Results after Percutaneous Surgical Treatment of Intra-articular Fracture of the Distal Radius
- Radiologic Reduction Loss after Surgical Treatment of Distal Radius Fracture
- Treatment of Intra-articular Fractures of the Distal Radius using Wrist Arthroscopy