Arch Hand Microsurg.
2024 Sep;29(3):146-153. 10.12790/ahm.24.0029.
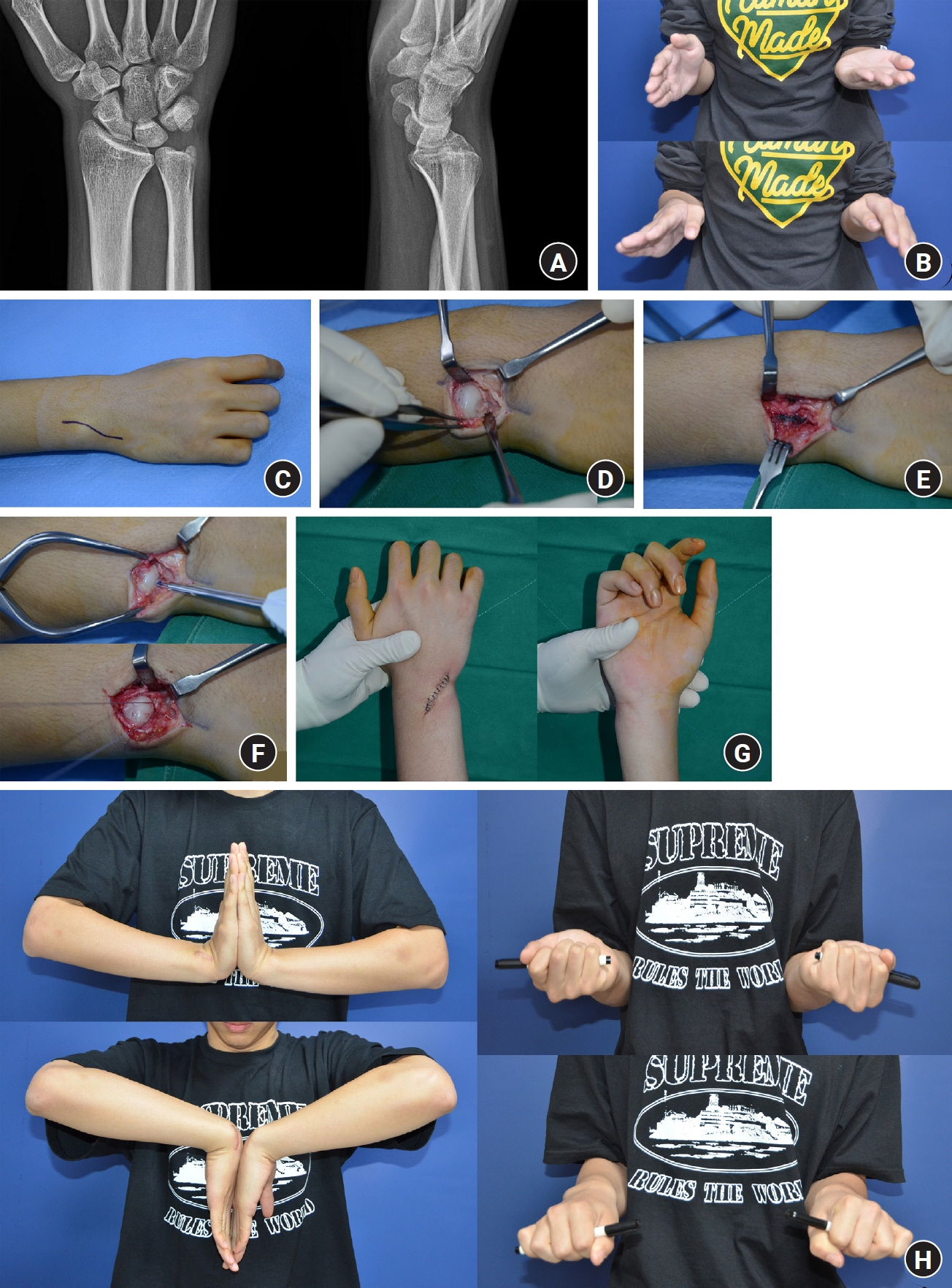
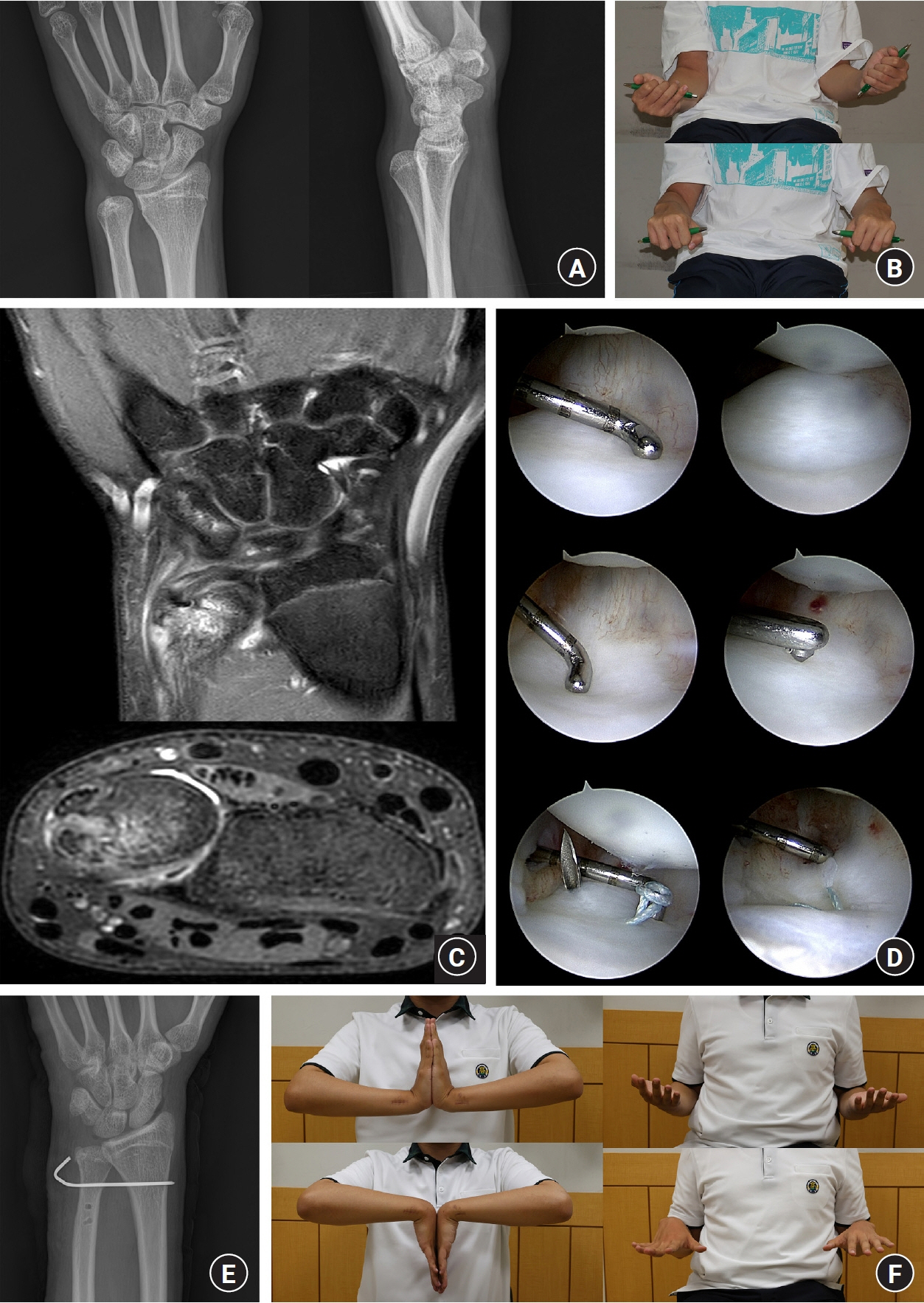
Traumatic posterior distal radioulnar joint instability treated with open versus arthroscopic methods: a retrospective cohort study
- Affiliations
-
- 1Department of Orthopedic Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 2Department of Orthopaedic Surgery, National Health Insurance Service Ilsan Hospital, Ilsan, Korea
- 3Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea
- 4Soo Hospital, Jeonju, Korea
- KMID: 2558738
- DOI: http://doi.org/10.12790/ahm.24.0029
Abstract
- Purpose
The distal radioulnar joint (DRUJ) at the wrist facilitates pronation and supination, and both bone structure and soft tissues contribute to its stability. This study analyzed the characteristics of patients with traumatic posterior DRUJ injuries and examined the clinical outcomes of open or arthroscopic treatment methods for these patients.
Methods
A retrospective cohort study was conducted on 14 patients with traumatic posterior DRUJ instability, excluding those with associated radius fractures. The study evaluated patient demographics, injury mechanisms, radiologic findings (DRUJ relationship in the coronal plane, sigmoid notch in the axial plane, the presence and location of an accompanying distal ulnar fracture, and ulnar variance in the opposite wrist), and clinical outcomes (visual analog scale, Disability of Arm, Shoulder, and Hand [DASH] score, and range of motion [ROM]). Patients were treated with either open repair or arthroscopic methods, and postoperative results were monitored over an average of 8.8 months.
Results
Ten patients had ulnar styloid fractures, with most occurring at the base or more proximally. The sigmoid notch was classified as the flat-face type in nine cases (64.3%) and the ski-slope type in five cases (35.7%). The clinical outcomes were favorable, with no significant differences between the open and arthroscopic groups regarding pain levels, DASH scores, and ROM.
Conclusion
Both treatment methods can achieve favorable clinical outcomes in managing traumatic posterior DRUJ instability.
Keyword
Figure
Reference
-
References
1. Mirghasemi AR, Lee DJ, Rahimi N, Rashidinia S, Elfar JC. Distal radioulnar joint instability. Geriatr Orthop Surg Rehabil. 2015; 6:225–9.
Article2. Stuart PR, Berger RA, Linscheid RL, An KN. The dorsopalmar stability of the distal radioulnar joint. J Hand Surg Am. 2000; 25:689–99.
Article3. Tolat AR, Stanley JK, Trail IA. A cadaveric study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg Br. 1996; 21:587–94.
Article4. Hagert E, Hagert CG. Understanding stability of the distal radioulnar joint through an understanding of its anatomy. Hand Clin. 2010; 26:459–66.
Article5. Khuyagbaatar B, Lee SJ, Bayarjargal U, Cheon M, Batbayar T, Kim YH. Contribution of a distal radioulnar joint stabilizer on forearm stability: a modeling study. Proc Inst Mech Eng H. 2021; 235:819–26.
Article6. He X, Chen F, Li J, Dong X, Zhang H, Guo L. MRI-related risk factors for distal radioulnar joint instability. Orthop Surg. 2023; 15:1289–97.7. Kihara H, Short WH, Werner FW, Fortino MD, Palmer AK. The stabilizing mechanism of the distal radioulnar joint during pronation and supination. J Hand Surg Am. 1995; 20:930–6.
Article8. Thomas BP, Sreekanth R. Distal radioulnar joint injuries. Indian J Orthop. 2012; 46:493–504.
Article9. Skalski MR, White EA, Patel DB, Schein AJ, RiveraMelo H, Matcuk GR Jr. The traumatized TFCC: an illustrated review of the anatomy and injury patterns of the triangular fibrocartilage complex. Curr Probl Diagn Radiol. 2016; 45:39–50.
Article10. Poppler LH, Moran SL. Acute distal radioulnar joint instability: evaluation and treatment. Hand Clin. 2020; 36:429–41.11. Scheer JH, Adolfsson LE. Patterns of triangular fibrocartilage complex (TFCC) injury associated with severely dorsally displaced extra-articular distal radius fractures. Injury. 2012; 43:926–32.12. Sammer DM, Chung KC. Management of the distal radioulnar joint and ulnar styloid fracture. Hand Clin. 2012; 28:199–206.
Article13. Kim JK, Yun YH, Kim DJ, Yun GU. Comparison of united and nonunited fractures of the ulnar styloid following volar-plate fixation of distal radius fractures. Injury. 2011; 42:371–5.
Article14. Zenke Y, Sakai A, Oshige T, Moritani S, Nakamura T. The effect of an associated ulnar styloid fracture on the outcome after fixation of a fracture of the distal radius. J Bone Joint Surg Br. 2009; 91:102–7.
Article15. Wijffels MM, Keizer J, Buijze GA, et al. Ulnar styloid process nonunion and outcome in patients with a distal radius fracture: a meta-analysis of comparative clinical trials. Injury. 2014; 45:1889–95.
Article16. Tsukuda Y, Kawamura D, Matsui Y, Iwasaki N. Morphological characteristics of the sigmoid notch of the distal radius affect the stress distribution patterns in the distal radioulnar joint. J Hand Surg Eur Vol. 2019; 44:496–502.
Article17. Jung HS, Park MJ, Won YS, Lee GY, Kim S, Lee JS. The correlation between shape of the sigmoid notch of the distal radius and the risk of triangular fibrocartilage complex foveal tear. Bone Joint J. 2020; 102-B:749–54.18. Tham SK, Bain GI. Sigmoid notch osseous reconstruction. Tech Hand Up Extrem Surg. 2007; 11:93–7.
Article19. Adams BD, Lawler E. Chronic instability of the distal radioulnar joint. J Am Acad Orthop Surg. 2007; 15:571–5.
Article20. Wallwork NA, Bain GI. Sigmoid notch osteoplasty for chronic volar instability of the distal radioulnar joint: a case report. J Hand Surg Am. 2001; 26:454–9.
Article21. O’Shaughnessy M, Shapiro LM, Schultz B, Retzky J, Finlay AK, Yao J. Morphology at the distal radioulnar joint: identifying the prevalence of reverse obliquity. J Wrist Surg. 2020; 9:417–24.
Article22. Ward LD, Ambrose CG, Masson MV, Levaro F. The role of the distal radioulnar ligaments, interosseous membrane, and joint capsule in distal radioulnar joint stability. J Hand Surg Am. 2000; 25:341–51.
Article23. Gofton WT, Gordon KD, Dunning CE, Johnson JA, King GJ. Comparison of distal radioulnar joint reconstructions using an active joint motion simulator. J Hand Surg Am. 2005; 30:733–42.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traumatic Triangular Fibrocartilage Complex Injuries and Instability of the Distal Radioulnar Joint
- Current Treatment of Triangular Fibrocartilage Complex Injuries
- The significance of distal radioulnar joint injury in distal radius fracture
- Anatomic Reconstruction of the Distal Radioulnar Ligament for Posttraumatic Distal Radioulnar Joint Instability
- Arthroscopic Repair of Triangular Fibrocartilage Complex Tear