Ann Hepatobiliary Pancreat Surg.
2024 Aug;28(3):350-357. 10.14701/ahbps.24-021.
Does perioperative hydrocortisone or indomethacin improve pancreatoduodenectomy outcomes? A triple arm, randomized placebo-controlled trial
- Affiliations
-
- 1Department of Surgical Gastroenterology, Asian Institute of Gastroenterology, Hyderabad, India
- KMID: 2558655
- DOI: http://doi.org/10.14701/ahbps.24-021
Abstract
- Backgrounds/Aims
This trial evaluated whether anti-inflammatory agents hydrocortisone (H) and indomethacin (I) could reduce major complications after pancreatoduodenectomy (PD).
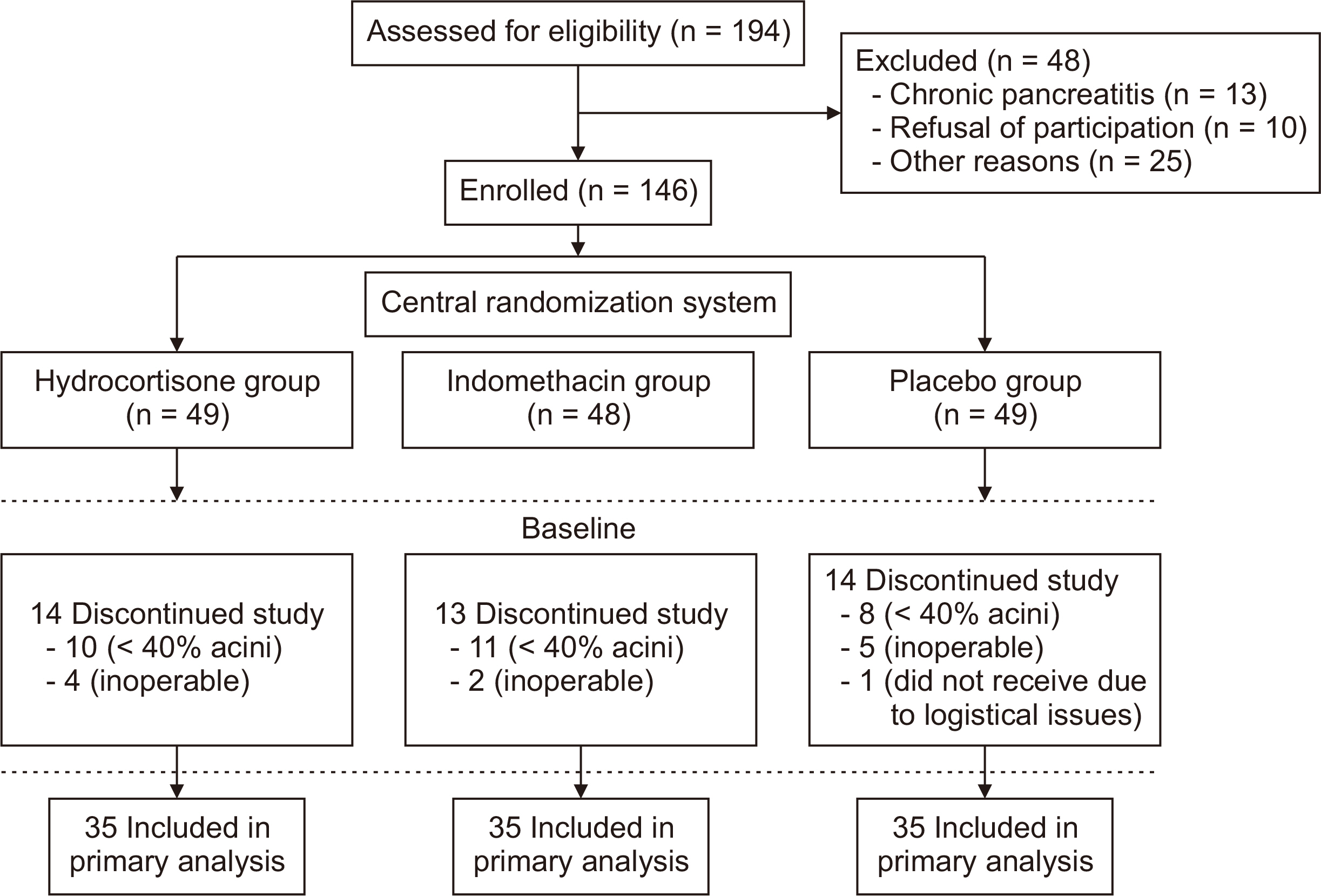
Methods
Between June 2018 and June 2020, 105 patients undergoing PD with > 40% of acini on the intraoperative frozen section were randomized into three groups (35 patients per group): 1) intravenous H 100 mg 8 hourly, 2) rectal I suppository 100 mg 12 hourly, and 3) placebo (P) from postoperative day (POD) 0–2. Participants, investigators, and outcome assessors were blinded. The primary outcome was major complications (Clavien–Dindo grades 3–5). Secondary outcomes were overall complications (Clavien–Dindo grades 1–5), Clinically relevant postoperative pancreatic fistula (CR-POPF), delayed gastric emptying (DGE), postpancreatectomy hemorrhage (PPH), surgical site infections (SSI), length of stay, POD-3 serum amylase, readmission rate, and mortality.
Results
Major complications were comparable (8.6%, 5.7%, and 8.6% in groups H, I, and P, respectively). However, overall complications were significantly lower in group H than in group P (45.7% vs. 80.0%, p = 0.006). CR-POPF (14.3% vs. 25.7%, p = 0.371), PPH (8.6% vs. 14.3%, p = 0.710), DGE (8.6% vs. 22.9%, p = 0.188), and SSI (14.3% vs. 25.7%, p = 0.371) were comparable between groups H and P. Major complications and overall complications in group I were 5.7% and 60.0%, respectively, which were comparable to those in groups P and H. CR-POPF rates in groups H, I, and P were 14.3%, 17.1%, and 25.7%, respectively, which was comparable.
Conclusions
H and I did not decrease major complications in PD.
Figure
Reference
-
References
1. Braga M, Capretti G, Pecorelli N, Balzano G, Doglioni C, Ariotti R, et al. 2011; A prognostic score to predict major complications after pancreaticoduodenectomy. Ann Surg. 254:702–707. discussion 707–708. DOI: 10.1097/SLA.0b013e31823598fb. PMID: 22042466.2. Kennedy EP, Yeo CJ. 2011; Dunking pancreaticojejunostomy versus duct- to-mucosa anastomosis. J Hepatobiliary Pancreat Sci. 18:769–774. DOI: 10.1007/s00534-011-0429-y. PMID: 21845376.3. Cameron JL, He J. 2015; Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg. 220:530–536. DOI: 10.1016/j.jamcollsurg.2014.12.031. PMID: 25724606.4. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. 2005; Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 138:8–13. DOI: 10.1016/j.surg.2005.05.001. PMID: 16003309.5. Räty S, Sand J, Lantto E, Nordback I. 2006; Postoperative acute pancreatitis as a major determinant of postoperative delayed gastric emptying after pancreaticoduodenectomy. J Gastrointest Surg. 10:1131–1139. DOI: 10.1016/j.gassur.2006.05.012. PMID: 16966032.6. Kleespies A, Albertsmeier M, Obeidat F, Seeliger H, Jauch KW, Bruns CJ. 2008; The challenge of pancreatic anastomosis. Langenbecks Arch Surg. 393:459–471. DOI: 10.1007/s00423-008-0324-4. PMID: 18379817.7. Chen H, Wang C, Shen Z, Wang W, Weng Y, Ying X, et al. 2023; Post-pancreatectomy acute pancreatitis after pancreaticoduodenectomy: a distinct clinical entity. Ann Surg. 278:e278–e283. DOI: 10.1097/SLA.0000000000005605. PMID: 35848748.8. Marchegiani G, Barreto SG, Bannone E, Sarr M, Vollmer CM, Connor S, et al. 2022; Postpancreatectomy acute pancreatitis (PPAP): definition and grading from the International Study Group for Pancreatic Surgery (ISGPS). Ann Surg. 275:663–672. DOI: 10.1097/SLA.0000000000005226. PMID: 34596077.9. Chui JN, Yang AJ, Nahm CB, Connor S, Gill AJ, Samra JS, et al. 2023; Clinical validation of the international study group of pancreatic surgery (ISGPS) definition for post-pancreatectomy acute pancreatitis. HPB (Oxford). 25:704–710. DOI: 10.1016/j.hpb.2023.01.014. PMID: 36934027.10. Laaninen M, Bläuer M, Vasama K, Jin H, Räty S, Sand J, et al. 2012; The risk for immediate postoperative complications after pancreaticoduodenectomy is increased by high frequency of acinar cells and decreased by prevalent fibrosis of the cut edge of pancreas. Pancreas. 41:957–961. DOI: 10.1097/MPA.0b013e3182480b81. PMID: 22699198.11. Laaninen M, Sand J, Nordback I, Vasama K, Laukkarinen J. 2016; Perioperative hydrocortisone reduces major complications after pancreaticoduodenectomy: a randomized controlled trial. Ann Surg. 264:696–702. DOI: 10.1097/SLA.0000000000001883. PMID: 27429037.12. Antila A, Siiki A, Sand J, Laukkarinen J. 2019; Perioperative hydrocortisone treatment reduces postoperative pancreatic fistula rate after open distal pancreatectomy. A randomized placebo-controlled trial. Pancreatology. 19:786–792. DOI: 10.1016/j.pan.2019.05.457. PMID: 31153781.13. Laaninen M, Bläuer M, Sand J, Nordback I, Laukkarinen J. 2014; Difference in early activation of NF-κB and MCP-1 in acinar-cell-rich versus fibrotic human pancreas exposed to surgical trauma and hypoxia. Gastroenterol Res Pract. 2014:460363. DOI: 10.1155/2014/460363. PMID: 25147563. PMCID: PMC4131420.14. Elmunzer BJ, Scheiman JM, Lehman GA, Chak A, Mosler P, Higgins PD, et al. 2012; A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med. 366:1414–1422. DOI: 10.1056/NEJMoa1111103. PMID: 22494121. PMCID: PMC3339271.15. Dindo D, Demartines N, Clavien PA. 2004; Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–213. DOI: 10.1097/01.sla.0000133083.54934.ae. PMID: 15273542. PMCID: PMC1360123.16. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. 2017; The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 161:584–591. DOI: 10.1016/j.surg.2016.11.014. PMID: 28040257.17. Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. 2007; Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 142:20–25. DOI: 10.1016/j.surg.2007.02.001. PMID: 17629996.18. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. 2007; Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 142:761–768. DOI: 10.1016/j.surg.2007.05.005. PMID: 17981197.19. Tarvainen T, Sirén J, Kokkola A, Sallinen V. 2020; Effect of hydrocortisone vs pasireotide on pancreatic surgery complications in patients with high risk of pancreatic fistula: a randomized clinical trial. JAMA Surg. 155:291–298. DOI: 10.1001/jamasurg.2019.6019. PMID: 32022887. PMCID: PMC7042940.20. Kriger AG, Gorin DS, Kaldarov AR, Galkin GV. [Prevention of pancreatic fistula after pancreatoduodenectomy]. Khirurgiia (Mosk). 2020; (11):61–65. Russian. DOI: 10.17116/hirurgia202011161. PMID: 33210509.21. Cecire J, Adams K, Pham H, Pang T, Burnett D. 2022; Pharmacological prevention of post-operative pancreatitis: systematic review and meta-analysis of randomized controlled trials on animal studies. ANZ J Surg. 92:1338–1346. DOI: 10.1111/ans.17417. PMID: 34936178.22. Levenick JM, Gordon SR, Fadden LL, Levy LC, Rockacy MJ, Hyder SM, et al. 2016; Rectal indomethacin does not prevent post-ERCP pancreatitis in consecutive patients. Gastroenterology. 150:911–917. quiz e19DOI: 10.1053/j.gastro.2015.12.040. PMID: 26775631. PMCID: PMC4808426.23. Sandini M, Ruscic KJ, Ferrone CR, Warshaw AL, Qadan M, Eikermann M, et al. 2018; Intraoperative dexamethasone decreases infectious complications after pancreaticoduodenectomy and is associated with long-term survival in pancreatic cancer. Ann Surg Oncol. 25:4020–4026. DOI: 10.1245/s10434-018-6827-5. PMID: 30298316.24. Bressan AK, Isherwood S, Bathe OF, Dixon E, Sutherland FR, Ball CG. 2022; Preoperative single-dose methylprednisolone prevents surgical site infections after major liver resection: a randomized controlled trial. Ann Surg. 275:281–287. DOI: 10.1097/SLA.0000000000004720. PMID: 33351452.25. Fernández-del Castillo C, Morales-Oyarvide V, McGrath D, Wargo JA, Ferrone CR, Thayer SP, et al. 2012; Evolution of the Whipple procedure at the Massachusetts General Hospital. Surgery. 152(3 Suppl 1):S56–S63. DOI: 10.1016/j.surg.2012.05.022. PMID: 22770961. PMCID: PMC3806095.26. Dawra R, Sah RP, Dudeja V, Rishi L, Talukdar R, Garg P, et al. 2011; Intra-acinar trypsinogen activation mediates early stages of pancreatic injury but not inflammation in mice with acute pancreatitis. Gastroenterology. 141:2210–2217.e2. DOI: 10.1053/j.gastro.2011.08.033. PMID: 21875495. PMCID: PMC3587766.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preventive efficacy of hydrocortisone enema for radiation proctitis in rectal cancer patients undergoing short-course radiotherapy: a phase II randomized placebo-controlled clinical trial
- Perioperative duloxetine as part of a multimodal analgesia regime reduces postoperative pain in lumbar canal stenosis surgery: a randomized, triple blind, and placebo-controlled trial
- Short-term outcomes of oropharyngeal administration of colostrum in preterm neonates: a double-blind placebocontrolled randomized trial
- Efficacy of Roflumilast in Bronchiectasis Patients with Frequent Exacerbations: A Double-Blinded, Randomized, Placebo-Controlled Pilot Clinical Trial
- Rosiglitazone for Active Ulcerative Colitis: A Randomized Placebo-Controlled Trial