Ewha Med J.
2024 Jul;47(3):e37. 10.12771/emj.2024.e37.
Epidemiology and management of infectious spondylitis in Korea: a narrative review
- Affiliations
-
- 1Department of Infectious Diseases, Chonnam National University Hospital, Gwangju, Korea
- 2Department of Infectious Diseases, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2558574
- DOI: http://doi.org/10.12771/emj.2024.e37
Abstract
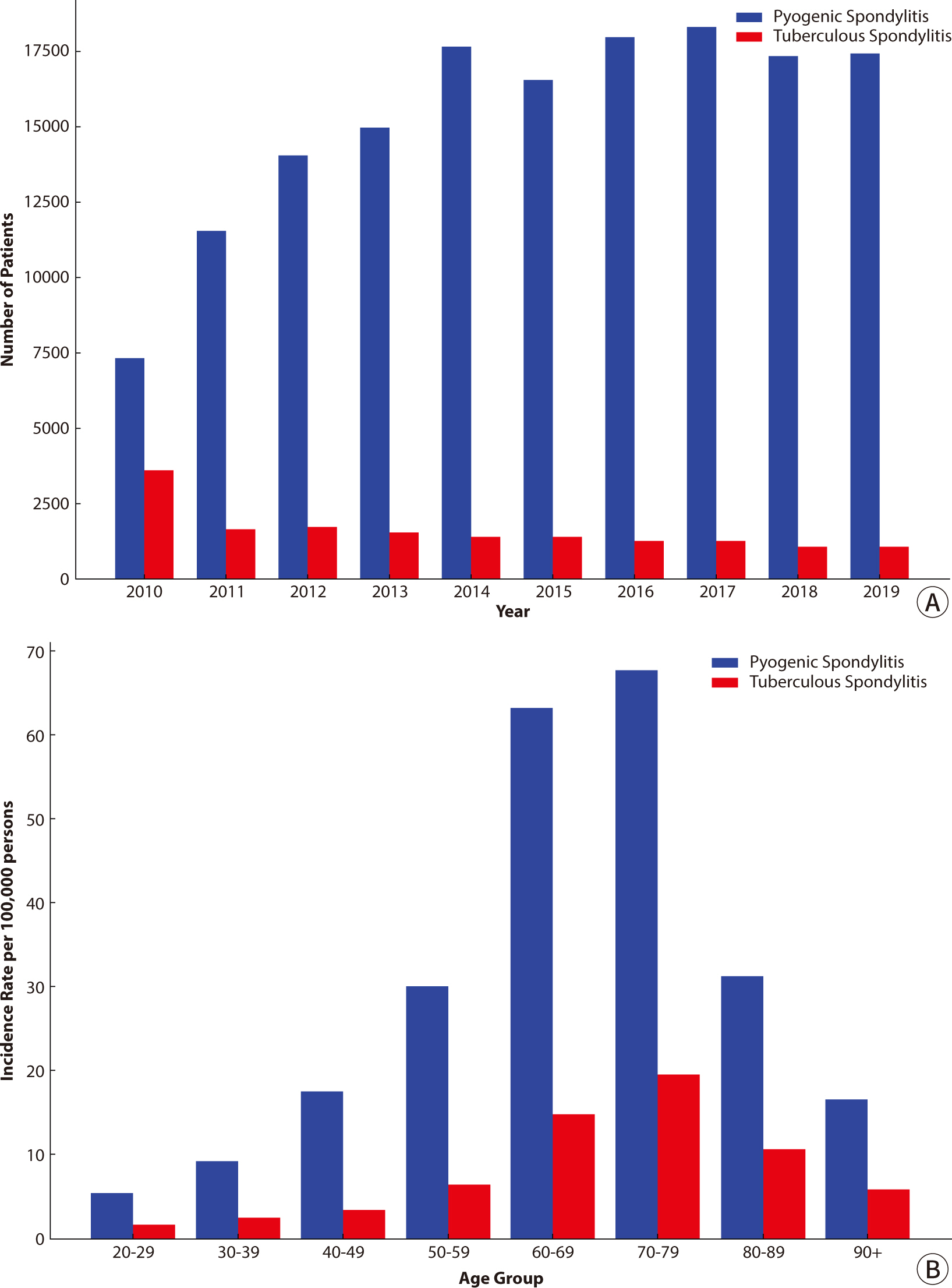
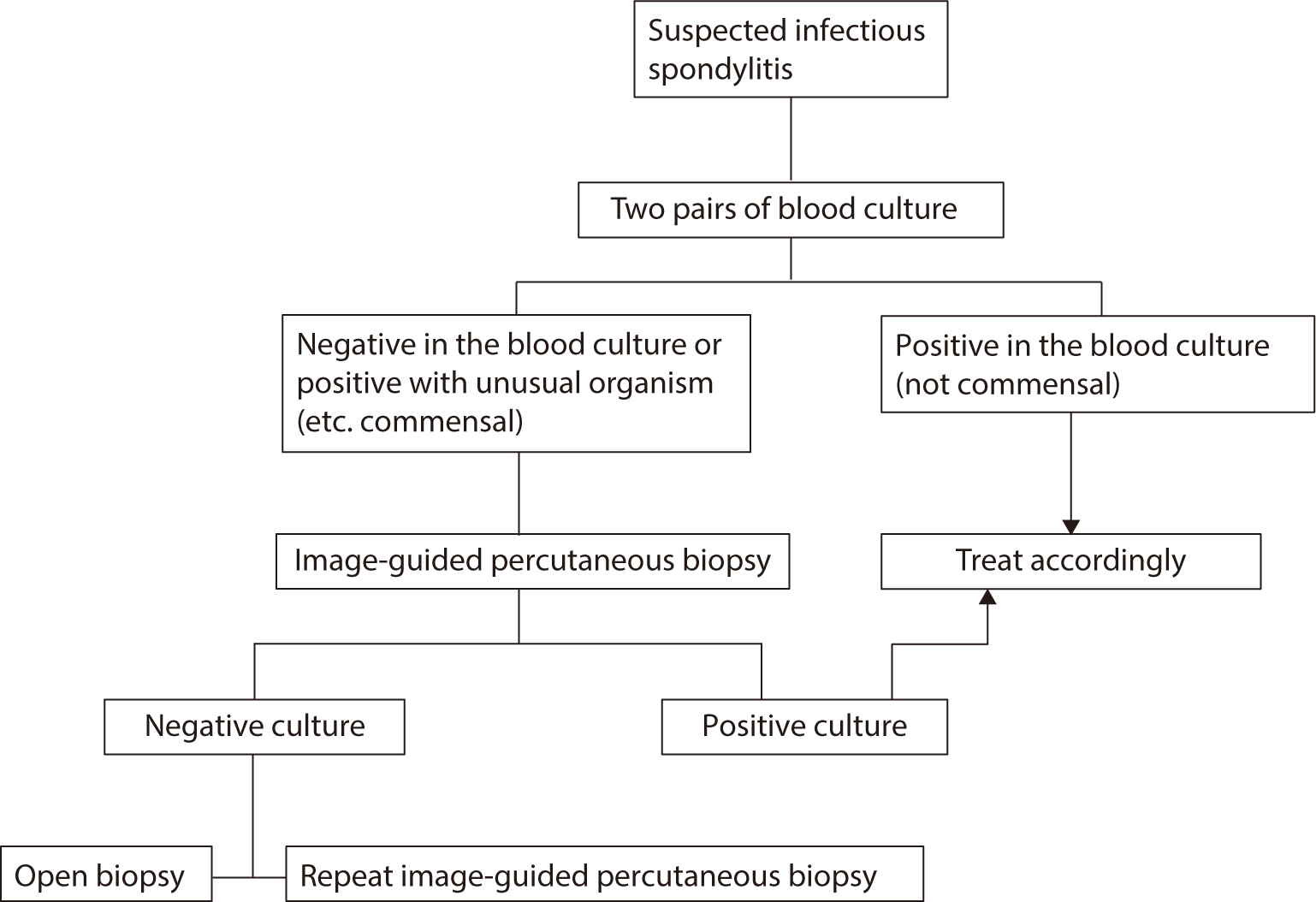
- Infectious spondylitis, an infection of the vertebral body, intervertebral disc, or paraspinal tissues, poses diagnostic and therapeutic challenges. This review examines the clinical approach and management of infectious spondylitis in Korea. The incidence of pyogenic spondylitis has increased, primarily due to the aging population, more frequent use of invasive procedures, and higher prevalence of immunocompromising conditions. Conversely, tuberculous spondylitis has declined, reflecting shifts in population demographics and medical practices. Staphylococcus aureus remains the predominant causative agent in pyogenic cases, while Mycobacterium tuberculosis is the primary pathogen in tuberculous spondylitis. The diagnosis is contingent upon clinical suspicion, inflammatory markers, imaging studies, and microbiological identification. MRI is the preferred imaging modality, offering high sensitivity and specificity. Blood cultures and tissue biopsy are instrumental in isolating the causative organism and determining its antibiotic susceptibility. Treatment involves antimicrobial therapy, spinal immobilization, and vigilant monitoring for complications. Surgical intervention may be necessary in cases involving neurological deficits, abscesses, or spinal instability. The prognosis for infectious spondylitis varies. Long-term complications, including chronic pain, neurological deficits, and spinal deformities, may arise and can meaningfully impact quality of life. Mortality is considerable and is influenced by comorbidities and disease severity. The risk of recurrence, particularly within the first year after treatment, is a concern. This review underscores the importance of ongoing research and education in refining diagnostic and treatment strategies for infectious spondylitis. As this condition becomes more common, these efforts offer hope for improving patient care and reducing the burden of this severe spinal infection.
Figure
Reference
-
References
1. Canale ST, Beaty JH. Campbell's operative orthopaedics. 11th ed. Philadelphia: Mosby;2008.2. Sapico FL, Montgomerie JZ. Pyogenic vertebral osteomyelitis: report of nine cases and review of the literature. Clin Infect Dis. 1979; 1(5):754–776. DOI: 10.1093/clinids/1.5.754. PMID: 542761.3. Kim CJ, Song KH, Jeon JH, Park WB, Park SW, Kim HB, et al. A comparative study of pyogenic and tuberculous spondylodiscitis. Spine. 2010; 35(21):E1096–E1100. DOI: 10.1097/BRS.0b013e3181e04dd3. PMID: 20838270.4. Lee Y, Kim BJ, Kim SH, Lee SH, Kim WH, Jin SW. Comparative analysis of spontaneous infectious spondylitis: pyogenic versus tuberculous. J Korean Neurosurg Soc. 2018; 61(1):81–88. DOI: 10.3340/jkns.2016.1212.005. PMID: 29354239. PMCID: PMC5769839.5. Kim YJ, Hong JB, Kim YS, Yi J, Choi JM, Sohn S. Change of pyogenic and tuberculous spondylitis between 2007 and 2016 year: a nationwide study. J Korean Neurosurg Soc. 2020; 63(6):784–793. DOI: 10.3340/jkns.2020.0013. PMID: 32623840. PMCID: PMC7671771.6. Son HJ, Kim M, Kim DH, Kang CN. Incidence and treatment trends of infectious spondylodiscitis in South Korea: a nationwide population-based study. PLoS One. 2023; 18(6):e0287846. DOI: 10.1371/journal.pone.0287846. PMID: 37384614. PMCID: PMC10309630.7. Moon YJ, Kim DY, Song KJ, Kim YJ, Lee KB. Relationship between percutaneous procedures and lumbar infections based on data from The National Health Insurance Review & Assessment Service of Korea. Clin Spine Surg. 2016; 29(1):E55–E60. DOI: 10.1097/BSD.0000000000000095. PMID: 24870119.8. Noh SH, Zhang HY, Lee SH, Choi JK, Chin DK. Changes in trends of spondylitis in Korea based on a nationwide database. Yonsei Med J. 2019; 60(5):487–489. DOI: 10.3349/ymj.2019.60.5.487. PMID: 31016913. PMCID: PMC6479126.9. Kim YI, Kim SE, Jang HC, Jung SI, Song SK, Park KH. Analysis of the clinical characteristics and prognostic factors of infectious spondylitis. Infect Chemother. 2011; 43(1):48–54. DOI: 10.3947/ic.2011.43.1.48.10. Kang SJ, Jang HC, Jung SI, Choe PG, Park WB, Kim CJ, et al. Clinical characteristics and risk factors of pyogenic spondylitis caused by gram-negative bacteria. PLoS One. 2015; 10(5):e0127126. DOI: 10.1371/journal.pone.0127126. PMID: 25978839. PMCID: PMC4433234.11. Kim CJ, Kim UJ, Kim HB, Park SW, Oh M, Park KH, et al. Vertebral osteomyelitis caused by non-tuberculous mycobacteria: predisposing conditions and clinical characteristics of six cases and a review of 63 cases in the literature. Infect Dis. 2016; 48(7):509–516. DOI: 10.3109/23744235.2016.1158418. PMID: 27002256.12. Lee JY, Jeon Y, Ahn MY, Ann HW, Jung IY, Jung W, et al. An imported case of Brucella melitensis infection in South Korea. Infect Chemother. 2018; 50(2):149–152. DOI: 10.3947/ic.2018.50.2.149. PMID: 29968983. PMCID: PMC6031603.13. Kim NJ. Microbiologic diagnosis of pyogenic spondylitis. Infect Chemother. 2021; 53(2):238–246. DOI: 10.3947/ic.2021.0054. PMID: 34216118. PMCID: PMC8258299.14. Park KH, Cho OH, Jung M, Suk KS, Lee JH, Park JS, et al. Clinical characteristics and outcomes of hematogenous vertebral osteomyelitis caused by gram-negative bacteria. J Infect. 2014; 69(1):42–50. DOI: 10.1016/j.jinf.2014.02.009. PMID: 24561018.15. Kim UJ, Bae JY, Kim SE, Kim CJ, Kang SJ, Jang HC, et al. Comparison of pyogenic postoperative and native vertebral osteomyelitis. Spine J. 2019; 19(5):880–887. DOI: 10.1016/j.spinee.2018.11.012. PMID: 30500465.16. Kim DY, Kim UJ, Yu Y, Kim SE, Kang SJ, Jun KI, et al. Microbial etiology of pyogenic vertebral osteomyelitis according to patient characteristics. Open Forum Infect Dis. 2020; 7(6):ofaa176. DOI: 10.1093/ofid/ofaa176. PMID: 32523973. PMCID: PMC7270706.17. Schirmer P, Renault CA, Holodniy M. Is spinal tuberculosis contagious? Int J Infect Dis. 2010; 14(8):E659–E666. DOI: 10.1016/j.ijid.2009.11.009. PMID: 20181507.18. Kim CJ, Kim EJ, Song KH, Choe PG, Park WB, Bang JH, et al. Comparison of characteristics of culture-negative pyogenic spondylitis and tuberculous spondylitis: a retrospective study. BMC Infect Dis. 2016; 16(1):560. DOI: 10.1186/s12879-016-1897-0. PMID: 27733126. PMCID: PMC5060001.19. Min J, Kim HW, Kim JS. Tuberculosis: Republic of Korea, 2021. Tuberc Respir Dis. 2023; 86(1):67–69. DOI: 10.4046/trd.2022.0111. PMID: 36281544. PMCID: PMC9816490.20. Berbari EF, Kanj SS, Kowalski TJ, Darouiche RO, Widmer AF, Schmitt SK, et al. 2015 Infectious Diseases Society of America (IDSA) clinical practice guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults. Clin Infect Dis. 2015; 61(6):e26–e46. DOI: 10.1093/cid/civ482. PMID: 26229122.21. Lener S, Hartmann S, Barbagallo GMV, Certo F, Thomé C, Tschugg A. Management of spinal infection: a review of the literature. Acta Neurochir. 2018; 160(3):487–496. DOI: 10.1007/s00701-018-3467-2. PMID: 29356895. PMCID: PMC5807463.22. Ryu S, Kim YJ, Lee S, Ryu J, Park S, Hong JU. Pathophysiology and MRI findings of infectious spondylitis and the differential diagnosis. J Korean Soc Radiol. 2021; 82(6):1413–1440. DOI: 10.3348/jksr.2021.0138. PMID: 36238882. PMCID: PMC9431966.23. Lee IS, Lee JS, Kim SJ, Jun S, Suh KT. Fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography imaging in pyogenic and tuberculous spondylitis: preliminary study. J Comput Assist Tomogr. 2009; 33(4):587–592. DOI: 10.1097/RCT.0b013e318187fef8. PMID: 19638856.24. Jeon I, Kong E. Application of simultaneous 18F-FDG PET/MRI for evaluating residual lesion in pyogenic spine infection: a case report. Infect Chemother. 2020; 52(4):626–633. DOI: 10.3947/ic.2020.52.4.626. PMID: 32757501. PMCID: PMC7779991.25. Bae JY, Kim CJ, Kim UJ, Song KH, Kim ES, Kang SJ, et al. Concordance of results of blood and tissue cultures from patients with pyogenic spondylitis: a retrospective cohort study. Clin Microbiol Infect. 2018; 24(3):279–282. DOI: 10.1016/j.cmi.2017.07.005. PMID: 28698035.26. Herren C, Jung N, Pishnamaz M, Breuninger M, Siewe J, Sobottke R. Spondylodiscitis: diagnosis and treatment options. Dtsch Arztebl Int. 2017; 114(51-52):875–882. DOI: 10.3238/arztebl.2017.0875. PMID: 29321098. PMCID: PMC5769318.27. Cho KS. Tuberculosis control in the Republic of Korea. Epidemiol Health. 2018; 40:e2018036. DOI: 10.4178/epih.e2018036. PMID: 30081621. PMCID: PMC6335497.28. Lee CM, Lee Y, Kang SJ, Kang CK, Choe PG, Song KH, et al. Positivity rates of mycobacterial culture in patients with tuberculous spondylitis according to methods and sites of biopsies: an analysis of 206 cases. Int J Infect Dis. 2022; 121:161–165. DOI: 10.1016/j.ijid.2022.05.021. PMID: 35568362.29. McNamara AL, Dickerson EC, Gomez-Hassan DM, Cinti SK, Srinivasan A. Yield of image-guided needle biopsy for infectious discitis: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2017; 38(10):2021–2027. DOI: 10.3174/ajnr.A5337. PMID: 28882866. PMCID: PMC7963615.30. Kim CJ, Kang SJ, Choe PG, Park WB, Jang HC, Jung SI, et al. Which tissues are best for microbiological diagnosis in patients with pyogenic vertebral osteomyelitis undergoing needle biopsy? Clin Microbiol Infect. 2015; 21(10):931–935. DOI: 10.1016/j.cmi.2015.06.021. PMID: 26119720.31. Maamari J, Tande AJ, Diehn F, Tai DBG, Berbari EF. Diagnosis of vertebral osteomyelitis. J Bone Joint Infect. 2022; 7(1):23–32. DOI: 10.5194/jbji-7-23-2022. PMID: 35136714. PMCID: PMC8814828.32. Zimmerli W. Clinical practice: vertebral osteomyelitis. N Engl J Med. 2010; 362(11):1022–1029. DOI: 10.1056/NEJMcp0910753. PMID: 20237348.33. Kasalak Ö, Adams HJA, Jutte PC, Overbosch J, Dierckx RAJO, Wouthuyzen-Bakker M, et al. Culture yield of repeat percutaneous image-guided biopsy after a negative initial biopsy in suspected spondylodiscitis: a systematic review. Skeletal Radiol. 2018; 47(10):1327–1335. DOI: 10.1007/s00256-018-3006-5. PMID: 29915936. PMCID: PMC6105158.34. Yeh KJ, Husseini JS, Hemke R, Nelson SB, Chang CY. CT-guided discitis-osteomyelitis biopsies with negative microbiology: how many days should we wait before repeating the biopsy? Skeletal Radiol. 2020; 49(4):619–623. DOI: 10.1007/s00256-019-03344-4. PMID: 31760457.35. Lee YD, Jeon YH, Kim YH, Ha KY, Hur JW, Ryu KS, et al. Clinical characteristics and outcomes of patients with culture-negative pyogenic spondylitis according to empiric glycopeptide use. Infect Chemother. 2019; 51(3):274–283. DOI: 10.3947/ic.2019.51.3.274. PMID: 31583861. PMCID: PMC6779574.36. Park KH, Kim DY, Lee YM, Lee MS, Kang KC, Lee JH, et al. Selection of an appropriate empiric antibiotic regimen in hematogenous vertebral osteomyelitis. PLoS One. 2019; 14(2):e0211888. DOI: 10.1371/journal.pone.0211888. PMID: 30735536. PMCID: PMC6368303.37. The Korean Society for Chemotherapy, The Korean Society of Infectious Diseases, The Korean Orthopaedic Association. Clinical guidelines for the antimicrobial treatment of bone and joint infections in Korea. Infect Chemother. 2014; 46(2):125–138. DOI: 10.3947/ic.2014.46.2.125. PMID: 25024877. PMCID: PMC4091374.38. Bernard L, Dinh A, Ghout I, Simo D, Zeller V, Issartel B, et al. Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: an open-label, non-inferiority, randomised, controlled trial. Lancet. 2015; 385(9971):875–882. DOI: 10.1016/S0140-6736(14)61233-2. PMID: 25468170.39. Yoon SH, Chung SK, Kim KJ, Kim HJ, Jin YJ, Kim HB. Pyogenic vertebral osteomyelitis: identification of microorganism and laboratory markers used to predict clinical outcome. Eur Spine J. 2010; 19(4):575–582. DOI: 10.1007/s00586-009-1216-1. PMID: 19937064. PMCID: PMC2899831.40. Pandita A, Madhuripan N, Pandita S, Hurtado RM. Challenges and controversies in the treatment of spinal tuberculosis. J Clin Tuberc Other Mycobact Dis. 2020; 19:100151. DOI: 10.1016/j.jctube.2020.100151. PMID: 32154388. PMCID: PMC7058908.41. An HS, Seldomridge JA. Spinal infections: diagnostic tests and imaging studies. Clin Orthop Relat Res. 2006; 444:27–33. DOI: 10.1097/01.blo.0000203452.36522.97. PMID: 16523124.42. Grados F, Lescure FX, Senneville E, Flipo RM, Schmit JL, Fardellone P. Suggestions for managing pyogenic (non-tuberculous) discitis in adults. Joint Bone Spine. 2007; 74(2):133–139. DOI: 10.1016/j.jbspin.2006.11.002. PMID: 17337352.43. Kowalski TJ, Layton KF, Berbari EF, Steckelberg JM, Huddleston PM, Wald JT, et al. Follow-up MR imaging in patients with pyogenic spine infections: lack of correlation with clinical features. AJNR Am J Neuroradiol. 2007; 28(4):693–699.44. Long B, Carlson J, Montrief T, Koyfman A. High risk and low prevalence diseases: spinal epidural abscess. Am J Emerg Med. 2022; 53:168–172. DOI: 10.1016/j.ajem.2022.01.008. PMID: 35063888.45. Frederickson B, Yuan H, Olans R. Management and outcome of pyogenic vertebral osteomyelitis. Clin Orthop Relat Res. 1978(131):160–167. DOI: 10.1097/00003086-197803000-00022.46. Jiménez-Mejías ME, de Dios Colmenero J, Sánchez-Lora FJ, Palomino-Nicás J, Reguera JM, García de la Heras J, et al. Postoperative spondylodiskitis: etiology, clinical findings, prognosis, and comparison with nonoperative pyogenic spondylodiskitis. Clin Infect Dis. 1999; 29(2):339–345. DOI: 10.1086/520212. PMID: 10476739.47. Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum. 2009; 39(1):10–17. DOI: 10.1016/j.semarthrit.2008.03.002. PMID: 18550153.48. Akiyama T, Chikuda H, Yasunaga H, Horiguchi H, Fushimi K, Saita K. Incidence and risk factors for mortality of vertebral osteomyelitis: a retrospective analysis using the Japanese diagnosis procedure combination database. BMJ Open. 2013; 3(3):e002412. DOI: 10.1136/bmjopen-2012-002412. PMID: 23533214. PMCID: PMC3612742.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Streptococcus Spondylitis Concomitant Infectious Endocarditis: A Case Report
- Comparison of Pyogenic and Tuberculous Spondylitis
- Reverse Latissimus Dorsi Muscle Flap for an Extensive Soft Tissue Defect Accompanied by Infectious Spondylitis
- CT Evaluation of Sacroiliitis' Differentiation of Infectious Sacroiliitis versus Ankylosing Spondylitis
- Preoperative Gadolinium-enhanced Magnetic Resonance Images on Infectious Spondylitis