Ewha Med J.
2024 Jul;47(3):e34. 10.12771/emj.2024.e34.
Status of and comprehensive preventive strategies for multidrug-resistant organisms in Korea: a focus on carbapenem-resistant Enterobacterales
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2558571
- DOI: http://doi.org/10.12771/emj.2024.e34
Abstract
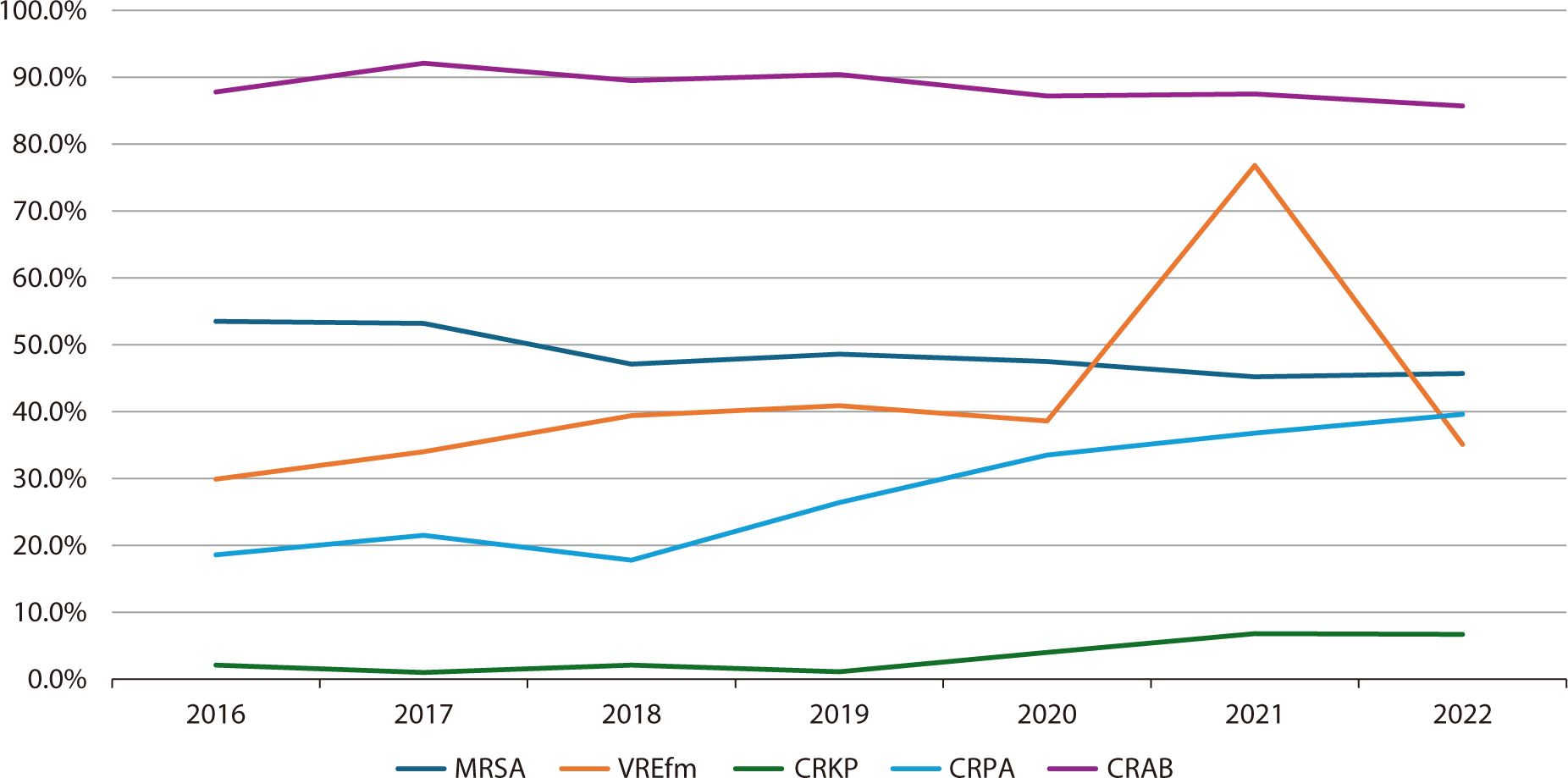
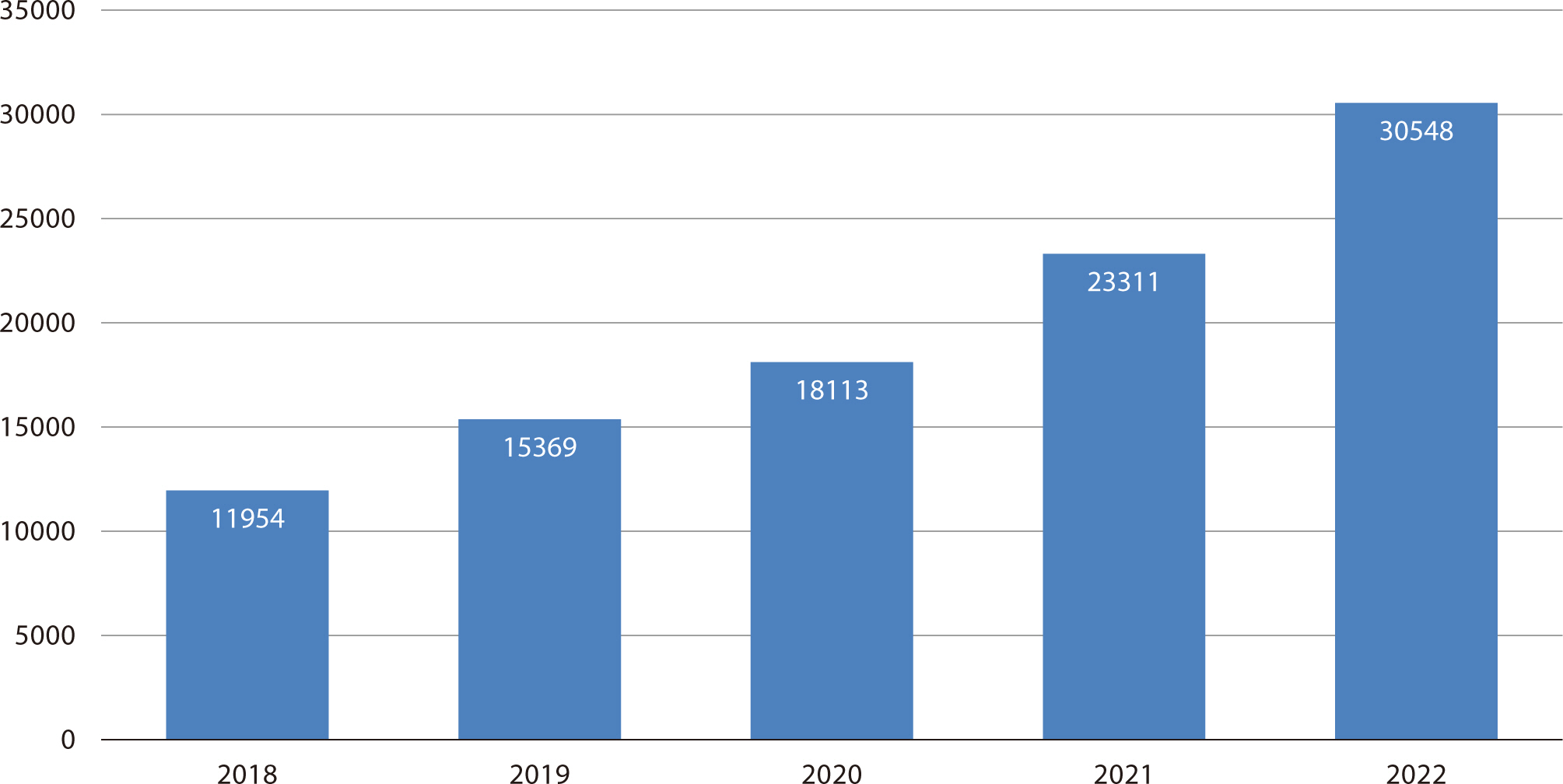
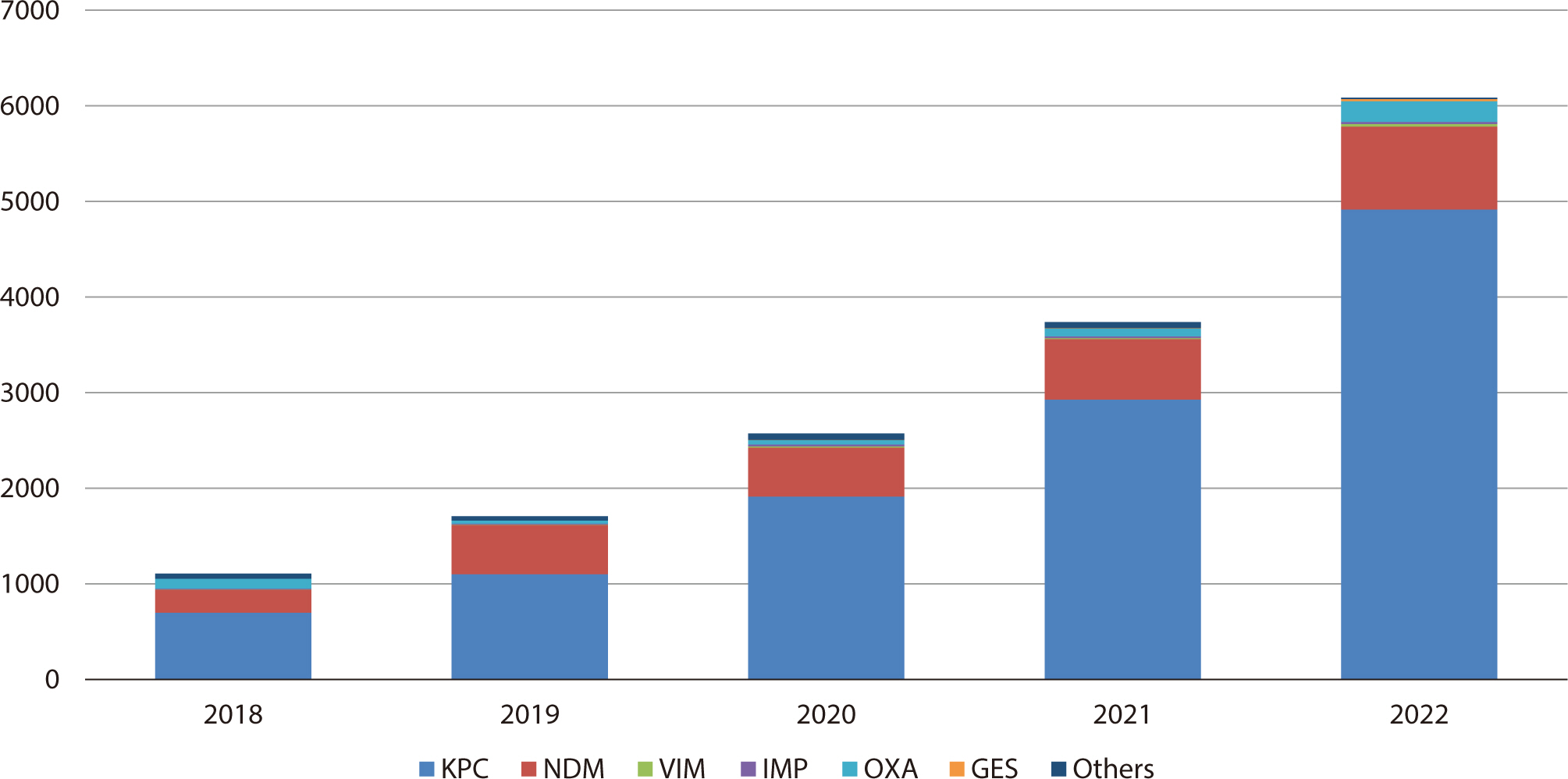
- The rise of multidrug-resistant organisms represents a serious global public health concern. In Korea, the increasing prevalence of carbapenem-resistant Enterobacterales (CRE) is particularly concerning due to the difficulties associated with treatment. Data from the Korea Global Antimicrobial Resistance Surveillance System indicate a yearly increase in CRE cases, with carbapenemase-producing Enterobacterales being the predominant type. The capacity of CRE to resist multiple broad-spectrum antibiotics leads to higher medical costs and mortality rates, underscoring the need for urgent action. Effective prevention is crucial to curbing CRE outbreaks and transmission. Antimicrobial stewardship programs (ASPs) play a key role and require commitment from healthcare professionals to minimize unnecessary antibiotic use, as well as from policymakers to ensure adherence to ASP guidelines. Given the complexity of CRE transmission, ASP efforts must be integrated with infection control strategies for maximum effectiveness. These strategies include adherence to standard and contact precautions, environmental disinfection, preemptive isolation, and comprehensive education and training for healthcare personnel. Additionally, surveillance testing for patients at high risk for CRE and the use of real-time diagnostic kits can facilitate early detection and reduce further transmission. Strategies for the prevention of CRE infection should be tailored to specific healthcare settings. Ongoing research is essential to update and refine infection control guidelines and effectively prevent CRE outbreaks.
Keyword
Figure
Reference
-
References
1. Perry J, Waglechner N, Wright G. The prehistory of antibiotic resistance. Cold Spring Harb Perspect Med. 2016; 6(6):a025197. DOI: 10.1101/cshperspect.a025197. PMID: 27252395. PMCID: PMC4888810.2. Serra-Burriel M, Keys M, Campillo-Artero C, Agodi A, Barchitta M, Gikas A, et al. Impact of multi-drug resistant bacteria on economic and clinical outcomes of healthcare-associated infections in adults: systematic review and meta-analysis. PLoS One. 2020; 15(1):e0227139. DOI: 10.1371/journal.pone.0227139. PMID: 31923281. PMCID: PMC6953842.3. Wellcome Collection. Antimicrobial resistance: tackling a crisis for the health and wealth of nations/the review on antimicrobial resistance, chaired by Jim O'Neill [Internet]. London (UK): Review on Antimicrobial Resistance;c2014. [cited 2024 May 14]. Available from: https://wellcomecollection.org/works/rdpck35v.4. Organisation for Economic Co-operation and Development [OECD]. Health at a glance 2023: OECD indicators [Internet]. Paris (FR): OECD;c2023. [cited 2024 May 14]. Available from:. DOI: 10.1787/7a7afb35-en.5. Kim D, Jeong SH. Current status of multidrug-resistant bacteria. J Korean Med Assoc. 2022; 65(8):468–477. DOI: 10.5124/jkma.2022.65.8.468.6. Kim D, Choi MH, Hong JS, Shin JH, Jeong SH. Current status and prospects of the National Antimicrobial Resistance Surveillance System, Kor-GLASS. Korean J Healthc Assoc Infect Control Prev. 2022; 27(2):96–103. DOI: 10.14192/kjicp.2022.27.2.96.7. Moore J, Gooday C, Soliman R, Dhatariya K. Reduction in the prevalence of methicillin-resistant Staphylococcus aureus in tissue and wound swab samples taken from outpatients attending a specialist diabetic foot clinic 2005–2021. Diabet Med. 2023; 40(10):e15081. DOI: 10.1111/dme.15081. PMID: 36883882.8. Kramer TS, Schröder C, Behnke M, Aghdassi SJ, Geffers C, Gastmeier P, et al. Decrease of methicillin resistance in Staphylococcus aureus in nosocomial infections in Germany: a prospective analysis over 10 years. J Infect. 2019; 78(3):215–219. DOI: 10.1016/j.jinf.2018.12.005. PMID: 30658080.9. Korea Disease Control and Prevention Agency. National Antimicrobial Resistance Surveillance in Korea 2021 annual report. Cheongju: Korea Disease Control and Prevention Agency;2022.10. Cantón R, Gijón D, Ruiz-Garbajosa P. Antimicrobial resistance in ICUs: an update in the light of the COVID-19 pandemic. Curr Opin Crit Care. 2020; 26(5):433–441. DOI: 10.1097/MCC.0000000000000755. PMID: 32739970.11. Lim J, Sim J, Lee H, Hyun J, Lee S, Park S. Characteristics of carbapenem-resistant Enterobacteriaceae (CRE) in the Republic of Korea, 2022. Public Health Wkly Rep. 2024; 17(4):115–127. DOI: 10.56786/PHWR.2024.17.4.1.12. Suay-García B, Pérez-Gracia MT. Present and future of carbapenem-resistant Enterobacteriaceae (CRE) infections. Antibiotics. 2019; 8(3):122. DOI: 10.3390/antibiotics8030122. PMID: 31430964. PMCID: PMC6784177.13. Kim MK, Joo S, Shin E, Kim J, Yoo J. Antimicrobial resistance and molecular characteristics of carbapenem-resistant Enterobacteriaceae isolated in the Republic of Korea, 2021. Public Health Wkly Rep. 2023; 16(18):541–559. DOI: 10.56786/PHWR.2023.16.18.1.14. Kim SH, Kim GR, Jeong J, Kim S, Shin JH. Prevalence and characteristics of carbapenemase-producing Enterobacteriaceae in three tertiary-care Korean university hospitals between 2017 and 2018. Jpn J Infect Dis. 2020; 73(6):431–436. DOI: 10.7883/yoken.JJID.2020.043. PMID: 32475870.15. Villanueva-Cotrina F, Condori DM, Gomez TO, Yactayo KM, Barron-Pastor H. First isolates of OXA-48-like carbapenemase-producing Enterobacteriaceae in a specialized cancer center. Infect Chemother. 2022; 54(4):765–773. DOI: 10.3947/ic.2022.0135. PMID: 36596684. PMCID: PMC9840961.16. Gasink LB, Edelstein PH, Lautenbach E, Synnestvedt M, Fishman NO. Risk factors and clinical impact of Klebsiella pneumoniae carbapenemase-producing K. pneumoniae. Infect Control Hosp Epidemiol. 2009; 30(12):1180–1185. DOI: 10.1086/648451. PMID: 19860564. PMCID: PMC2893218.17. Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol. 2008; 29(12):1099–1106. DOI: 10.1086/592412. PMID: 18973455.18. Tandan M, Thapa P, Maharjan P, Bhandari B. Impact of antimicrobial stewardship program on antimicrobial-resistance and prescribing in nursing homes: a systematic review and meta-analysis. J Glob Antimicrob Resist. 2022; 29:74–87. DOI: 10.1016/j.jgar.2022.02.002. PMID: 35158078.19. Choi H, Ahn H, Lee R, Cho SY, Lee DG. Bloodstream infections in patients with hematologic diseases: causative organisms and factors associated with resistance. Infect Chemother. 2022; 54(2):340–352. DOI: 10.3947/ic.2022.0069. PMID: 35794719. PMCID: PMC9259903.20. Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016; 62(10):e51–e77. DOI: 10.1093/cid/ciw118. PMID: 27080992. PMCID: PMC5006285.21. Cheong HS, Park KH, Kim B, Eun BW, Kim H, Kim YC, et al. Developing core elements and checklist items for implementing Antimicrobial Stewardship Programs in Korean General Hospitals: a modified Delphi survey. Infect Chemother. 2023; 55(1):59–68. DOI: 10.3947/ic.2022.0169. PMID: 36864763. PMCID: PMC10079444.22. Spellberg B, Srinivasan A, Chambers HF. New societal approaches to empowering antibiotic stewardship. JAMA. 2016; 315(12):1229–1230. DOI: 10.1001/jama.2016.1346. PMID: 26914942. PMCID: PMC5611826.23. Cheong HS, Park KH, Kim HB, Kim SW, Kim B, Moon C, et al. Core elements for implementing antimicrobial stewardship programs in Korean general hospitals. Infect Chemother. 2022; 54(4):637–673. DOI: 10.3947/ic.2022.0171. PMID: 36596679. PMCID: PMC9840955.24. Chen HY, Jean SS, Lee YL, Lu MC, Ko WC, Liu PY, et al. Carbapenem-resistant Enterobacterales in long-term care facilities: a global and narrative review. Front Cell Infect Microbiol. 2021; 11:601968. DOI: 10.3389/fcimb.2021.601968. PMID: 33968793. PMCID: PMC8102866.25. Pittet D, Allegranzi B, Sax H, Dharan S, Pessoa-Silva CL, Donaldson L, et al. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis. 2006; 6(10):641–652. DOI: 10.1016/S1473-3099(06)70600-4. PMID: 17008173.26. World Health Organization. Evidence of hand hygiene to reduce transmission and infections by multi-drug resistant organisms in healthcare settings [Internet]. Geneva (CH): World Health Organization;p. c2014. [cited 2024 May 14]. Available from: https://cdn.who.int/media/docs/default-source/integrated-health-services-%28ihs%29/infection-prevention-and-control/mdro-literature-review.pdf.27. Korea Disease Control and Prevention Agency. Healthcare associated infectious diseases management guideline, 2024 [Internet]. Cheongju (KR): Korea Disease Control and Prevention Agency;c2022. [cited 2024 May 14]. Available from: https://www.kdca.go.kr/board/board.es?mid=a20507020000&bid=0019.28. World Health Organization. Guidelines for the prevention and control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities [Internet]. Geneva (CH): World Health Organization;c2017. [cited 2024 May 14]. Available from: https://iris.who.int/handle/10665/259462.29. Boyce JM, Pittet D. Guideline for hand hygiene in health-care settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR Recomm Rep. 2002; 51(RR-16):1–45. DOI: 10.1086/503164. PMID: 12515399.30. Palmore TN, Henderson DK. Managing transmission of carbapenem-resistant enterobacteriaceae in healthcare settings: a view from the trenches. Clin Infect Dis. 2013; 57(11):1593–1599. DOI: 10.1093/cid/cit531. PMID: 23934166. PMCID: PMC3888298.31. Ben-David D, Maor Y, Keller N, Regev-Yochay G, Tal I, Shachar D, et al. Potential role of active surveillance in the control of a hospital-wide outbreak of carbapenem-resistant Klebsiella pneumoniae infection. Infect Control Hosp Epidemiol. 2010; 31(6):620–626. DOI: 10.1086/652528. PMID: 20370465.32. Lee KH. The value and clinical application of carbapenem-resistant Enterobacterales surveillance culture. Korean J Healthc Assoc Infect Control Prev. 2023; 28(2):185–191. DOI: 10.14192/kjicp.2023.28.2.185.33. Yao Y, Falgenhauer L, Rezazadeh Y, Falgenhauer J; the IncN Study Group, Imirzalioglu C, et al. Predominant transmission of KPC-2 carbapenemase in Germany by a unique IncN plasmid variant harboring a novel non-transposable element (NTE KPC -Y). Microbiol Spectr. 2024; 12(1):e02564–23. DOI: 10.1128/spectrum.02564-23. PMID: 38084979. PMCID: PMC10790570.34. Iovleva A, Doi Y. Carbapenem-resistant Enterobacteriaceae. Clin Lab Med. 2017; 37(2):303–315. DOI: 10.1016/j.cll.2017.01.005. PMID: 28457352. PMCID: PMC5412586.35. Kim CJ. Current status of antibiotic stewardship and the role of biomarkers in Antibiotic Stewardship Programs. Infect Chemother. 2022; 54(4):674–698. DOI: 10.3947/ic.2022.0172. PMID: 36596680. PMCID: PMC9840952.36. Gomides MDA, Fontes AMS, Silveira AOSM, Matoso DC, Ferreira AL, Sadoyama G. The importance of active surveillance of carbapenem-resistant Enterobacterales (CRE) in colonization rates in critically ill patients. PLoS One. 2022; 17(1):e0262554. DOI: 10.1371/journal.pone.0262554. PMID: 35051212. PMCID: PMC8775193.37. Kochar S, Sheard T, Sharma R, Hui A, Tolentino E, Allen G, et al. Success of an infection control program to reduce the spread of carbapenem-resistant Klebsiella pneumoniae. Infect Control Hosp Epidemiol. 2009; 30(5):447–452. DOI: 10.1086/596734. PMID: 19301985.38. Huang YT, Kuo YW, Lee NY, Tien N, Liao CH, Teng LJ, et al. Evaluating NG-test CARBA 5 multiplex immunochromatographic and Cepheid Xpert Carba-R assays among carbapenem-resistant Enterobacterales isolates associated with bloodstream infection. Microbiol Spectr. 2022; 10(1):e01728–21. DOI: 10.1128/spectrum.01728-21. PMID: 35019772. PMCID: PMC8754146.39. Li HH, He ZJ, Xie LM, Zhang JS, Xie TA, Fan SJ, et al. Evaluation of Xpert Carba-R assay for the detection of carbapenemase genes in gram-negative bacteria. Biomed Res Int. 2021; 2021:6614812. DOI: 10.1155/2021/6614812. PMID: 33928150. PMCID: PMC8049809.40. Centers for Disease Control and Prevention. Facility guidance for control of carbapenem-resistant Enterobacteriaceae (CRE): November 2015 update - CRE toolkit [Internet]. Atlanta (GA): Centers for Disease Control and Prevention;c2015. [cited 2024 May 14]. Available from: https://stacks.cdc.gov/view/cdc/79104.41. Kizny Gordon AE, Mathers AJ, Cheong EYL, Gottlieb T, Kotay S, Walker AS, et al. The hospital water environment as a reservoir for carbapenem-resistant organisms causing hospital-acquired infections: a systematic review of the literature. Clin Infect Dis. 2017; 64(10):1435–1444. DOI: 10.1093/cid/cix132. PMID: 28200000.42. Munoz-Price LS, Hayden MK, Lolans K, Won S, Calvert K, Lin M, et al. Successful control of an outbreak of Klebsiella pneumoniae carbapenemase: producing K. pneumoniae at a long-term acute care hospital. Infect Control Hosp Epidemiol. 2010; 31(4):341–347. DOI: 10.1086/651097. PMID: 20175685.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Identification and infection control of carbapenem-resistant Enterobacterales in intensive care units
- Changing Epidemiology of Multidrug-resistant Pathogens: A New Battle against Carbapenem-resistant Enterobacterales
- Strategies to combat Gram-negative bacterial resistance to conventional antibacterial drugs: a review
- Awareness on the spread of carbapenem-resistant Enterobacterales in animals as One Health
- Multidrug-resistant Organisms and Healthcare-associated Infections