J Korean Med Sci.
2024 Aug;39(32):e229. 10.3346/jkms.2024.39.e229.
Long-Term Outcomes of Gamma Knife Radiosurgery for Cerebral Cavernous Malformations: 10 Years and Beyond
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Neurosurgery, Pusan National University Hospital, Busan, Korea
- 3Department of Neurosurgery, Chungnam National University Sejong Hospital, Sejong, Korea
- 4Department of Neurosurgery, Gachon University Gil Medical Center, Incheon, Korea
- 5Department of Neurosurgery, Soonchunhyang University Seoul Hospital, Seoul, Korea
- 6Department of Internal Medicine, College of Medicine, Chung-Ang University, Seoul, Korea
- 7Department of Neurosurgery, Cancer Research Institute and Ischemic/Hypoxic Disease Institute, Seoul National University College of Medicine, Seoul, Korea
- 8Advanced Institute of Convergence Technology, Seoul National University, Suwon, Korea
- KMID: 2558529
- DOI: http://doi.org/10.3346/jkms.2024.39.e229
Abstract
- Background
We aimed to evaluate long-term outcomes of gamma knife radiosurgery (GKS) for cerebral cavernous malformations (CCMs).
Methods
Among the 233 CCM patients who underwent GKS, 79 adult patients (96 lesions) followed for over 10 years were included and analyzed retrospectively. Annual hemorrhage rate (AHR) was analyzed the entire cohort of 233 patients and the subset of 79 enrolled patients by dividing lesions into overall CCM lesions and brainstem lesions. AHR, neurologic outcome, adverse radiation effect (ARE), and changes of lesions in magnetic resonance imaging (MRI) were compared before and after GKS. Cox-regression analysis was performed to identify risk factors for hemorrhage following GKS.
Results
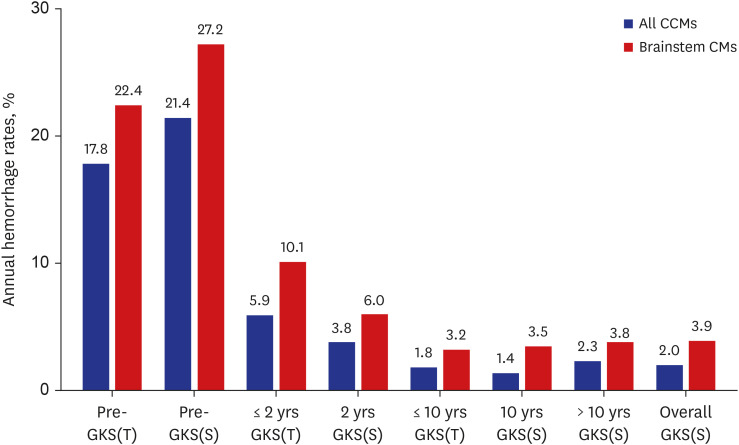
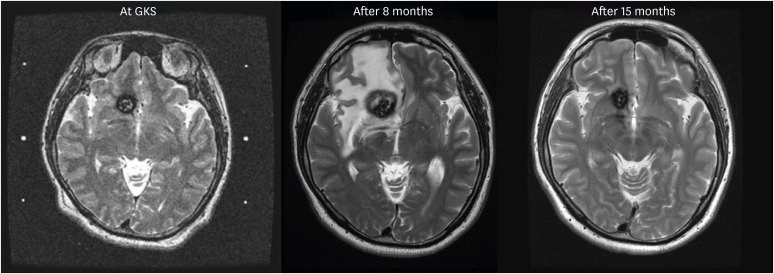
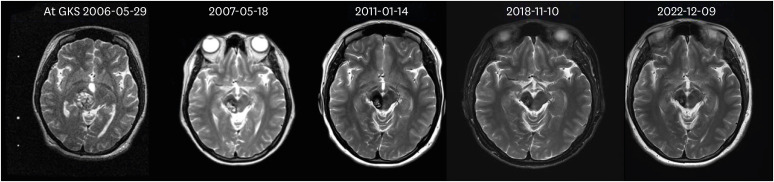
Mean follow-up duration of 79 enrolled patients was 14 years (range, 10–23 years). The AHR of all CCMs for entire cohort at each time point was 17.8% (pre-GKS), 5.9% (≤ 2 years post-GKS), 1.8% (≤ 10 years post-GKS). The AHR of all CCM for 79 enrolled patients was 21.4% (pre-GKS), 3.8% (2 years post-GKS), 1.4% (10 years post-GKS), and 2.3% (> 10 years post-GKS). The AHR of brainstem cavernous malformation (CM) for entire cohort at each time point was 22.4% (pre-GKS), 10.1% (≤ 2 years post-GKS), 3.2% (≤ 10 years post-GKS). The AHR of brainstem CM for 79 enrolled patients was 27.2% (pre-GKS), 5.8% (2 years post-GKS), 3.4% (10 years post-GKS), and 3.5% (> 10 years post-GKS). Out of the 79 enrolled patients, 35 presented with focal neurologic deficits at the initial clinical visit. Among these patients, 74.3% showed recovery at the last follow-up. Symptomatic ARE occurred in five (6.4%) patients. No mortality occurred. Most lesions were decreased in size at the last follow-up MRI. Previous hemorrhage history (hazard ratio [HR], 8.38; 95% confidence interval [CI], 1.07–65.88; P = 0.043), and brainstem location (HR, 3.10; 95% CI, 1.26–7.64; P = 0.014) were significant risk factors for hemorrhage event.
Conclusion
GKS for CCM showed favorable long-term outcomes. GKS should be considered for CCM, especially when it has a previous hemorrhage history and brainstem location.
Keyword
Figure
Reference
-
1. Zabramski JM, Wascher TM, Spetzler RF, Johnson B, Golfinos J, Drayer BP, et al. The natural history of familial cavernous malformations: results of an ongoing study. J Neurosurg. 1994; 80(3):422–432. PMID: 8113854.2. Batra S, Lin D, Recinos PF, Zhang J, Rigamonti D. Cavernous malformations: natural history, diagnosis and treatment. Nat Rev Neurol. 2009; 5(12):659–670. PMID: 19953116.3. Robinson JR Jr, Awad IA, Magdinec M, Paranandi L. Factors predisposing to clinical disability in patients with cavernous malformations of the brain. Neurosurgery. 1993; 32(5):730–736. PMID: 8492847.4. Kondziolka D, Lunsford LD, Flickinger JC, Kestle JR. Reduction of hemorrhage risk after stereotactic radiosurgery for cavernous malformations. J Neurosurg. 1995; 83(5):825–831. PMID: 7472550.5. Mouchtouris N, Chalouhi N, Chitale A, Starke RM, Tjoumakaris SI, Rosenwasser RH, et al. Management of cerebral cavernous malformations: from diagnosis to treatment. Sci World J. 2015; 2015:808314.6. Hasegawa T, McInerney J, Kondziolka D, Lee JY, Flickinger JC, Lunsford LD. Long-term results after stereotactic radiosurgery for patients with cavernous malformations. Neurosurgery. 2002; 50(6):1190–1197. PMID: 12015835.7. Kim DG, Choe WJ, Paek SH, Chung HT, Kim IH, Han DH. Radiosurgery of intracranial cavernous malformations. Acta Neurochir (Wien). 2002; 144(9):869–878. PMID: 12376768.8. Kida Y, Hasegawa T. Radiosurgery for cavernous malformations: results of long-term follow-up. In : Proceedings of Radiosurgery: 6th International Stereotactic Radiosurgery Society Meeting; 2003 June; Kyoto, Japan. Basel, Switzerland: KARGER;2004.9. Liscák R, Vladyka V, Simonová G, Vymazal J, Novotny J Jr. Gamma knife surgery of brain cavernous hemangiomas. J Neurosurg. 2005; 102(Suppl):207–213.10. Liu KD, Chung WY, Wu HM, Shiau CY, Wang LW, Guo WY, et al. Gamma knife surgery for cavernous hemangiomas: an analysis of 125 patients. J Neurosurg. 2005; 102(Suppl):81–86.11. Kida Y, Hasegawa T, Iwai Y, Shuto T, Satoh M, Kondoh T, et al. Radiosurgery for symptomatic cavernous malformations: a multi-institutional retrospective study in Japan. Surg Neurol Int. 2015; 6(Suppl 5):S249–S257. PMID: 26005588.12. López-Serrano R, Martínez NE, Kusak ME, Quirós A, Martínez R. Significant hemorrhage rate reduction after Gamma Knife radiosurgery in symptomatic cavernous malformations: long-term outcome in 95 case series and literature review. Stereotact Funct Neurosurg. 2017; 95(6):369–378. PMID: 29131117.13. Lee CC, Wang WH, Yang HC, Lin CJ, Wu HM, Lin YY, et al. Gamma Knife radiosurgery for cerebral cavernous malformation. Sci Rep. 2019; 9(1):19743. PMID: 31874979.14. Monaco EA, Khan AA, Niranjan A, Kano H, Grandhi R, Kondziolka D, et al. Stereotactic radiosurgery for the treatment of symptomatic brainstem cavernous malformations. Neurosurg Focus. 2010; 29(3):E11.15. Lee CC, Pan DH, Chung WY, Liu KD, Yang HC, Wu HM, et al. Brainstem cavernous malformations: the role of Gamma Knife surgery. J Neurosurg. 2012; 117(Suppl):164–169. PMID: 23205805.16. Fuetsch M, El Majdoub F, Hoevels M, Müller RP, Sturm V, Maarouf M. Stereotactic LINAC radiosurgery for the treatment of brainstem cavernomas. Strahlenther Onkol. 2012; 188(4):311–316. PMID: 22314579.17. Park SH, Hwang SK. Gamma knife radiosurgery for symptomatic brainstem intra-axial cavernous malformations. World Neurosurg. 2013; 80(6):e261–e266. PMID: 23010066.18. Kim BS, Yeon JY, Kim JS, Hong SC, Lee JI. Gamma knife radiosurgery of the symptomatic brain stem cavernous angioma with low marginal dose. Clin Neurol Neurosurg. 2014; 126:110–114. PMID: 25238102.19. Liu HB, Wang Y, Yang S, Gong FL, Xu YY, Wang W. Gamma knife radiosurgery for brainstem cavernous malformations. Clin Neurol Neurosurg. 2016; 151:55–60. PMID: 27794267.20. Park K, Kim JW, Chung HT, Paek SH, Kim DG. Long-term outcome of Gamma Knife radiosurgery for symptomatic brainstem cavernous malformation. World Neurosurg. 2018; 116:e1054–e1059. PMID: 29864574.21. Kondziolka D, Lunsford LD, Kestle JR. The natural history of cerebral cavernous malformations. J Neurosurg. 1995; 83(5):820–824. PMID: 7472549.22. García-Pérez D, Panero I, Lagares A, González P. De novo cavernous malformation associated with a pre-existing developmental venous anomaly: could magnetic resonance findings predict evolution? Clin Neuroradiol. 2020; 30(1):181–184. PMID: 31152189.23. Cox EM, Bambakidis NC, Cohen ML. Pathology of cavernous malformations. Handb Clin Neurol. 2017; 143:267–277. PMID: 28552149.24. Barker FG 2nd, Amin-Hanjani S, Butler WE, Lyons S, Ojemann RG, Chapman PH, et al. Temporal clustering of hemorrhages from untreated cavernous malformations of the central nervous system. Neurosurgery. 2001; 49(1):15–24. PMID: 11440436.25. Torgerson DJ, Torgerson CJ. The limitations of before and after designs. Designing Randomised Trials in Health, Education and the Social Sciences. London, UK: Palgrave Macmillan UK;2008. p. 9–16.26. Washington CW, McCoy KE, Zipfel GJ. Update on the natural history of cavernous malformations and factors predicting aggressive clinical presentation. Neurosurg Focus. 2010; 29(3):E7.27. Del Curling O Jr, Kelly DL Jr, Elster AD, Craven TE. An analysis of the natural history of cavernous angiomas. J Neurosurg. 1991; 75(5):702–708. PMID: 1919691.28. Taslimi S, Modabbernia A, Amin-Hanjani S, Barker FG 2nd, Macdonald RL. Natural history of cavernous malformation: systematic review and meta-analysis of 25 studies. Neurology. 2016; 86(21):1984–1991. PMID: 27164680.29. Ganz JC, Reda WA, Abdelkarim K. Adverse radiation effects after Gamma Knife Surgery in relation to dose and volume. Acta Neurochir (Wien). 2009; 151(1):9–19. PMID: 19129961.30. Shin SS, Murdoch G, Hamilton RL, Faraji AH, Kano H, Zwagerman NT, et al. Pathological response of cavernous malformations following radiosurgery. J Neurosurg. 2015; 123(4):938–944. PMID: 26090838.31. Gewirtz RJ, Steinberg GK, Crowley R, Levy RP. Pathological changes in surgically resected angiographically occult vascular malformations after radiation. Neurosurgery. 1998; 42(4):738–742. PMID: 9574637.32. Cheng L, Ma L, Ren H, Zhao H, Pang Y, Wang Y, et al. Alterations in the expression of vascular endothelial growth factor in the rat brain following gamma knife surgery. Mol Med Rep. 2014; 10(5):2263–2270. PMID: 25176344.33. Jung KH, Chu K, Jeong SW, Park HK, Bae HJ, Yoon BW. Cerebral cavernous malformations with dynamic and progressive course: correlation study with vascular endothelial growth factor. Arch Neurol. 2003; 60(11):1613–1618. PMID: 14623736.34. Pinedo HM. The role of VEGF in oncology: effects on hemostasis and thrombosis. Pathophysiol Haemost Thromb. 2003; 33(Suppl 1):11–12. PMID: 12954991.35. Clatterbuck RE, Moriarity JL, Elmaci I, Lee RR, Breiter SN, Rigamonti D. Dynamic nature of cavernous malformations: a prospective magnetic resonance imaging study with volumetric analysis. J Neurosurg. 2000; 93(6):981–986. PMID: 11117871.36. Nikoubashman O, Di Rocco F, Davagnanam I, Mankad K, Zerah M, Wiesmann M. Prospective hemorrhage rates of cerebral cavernous malformations in children and adolescents based on MRI appearance. AJNR Am J Neuroradiol. 2015; 36(11):2177–2183. PMID: 26272978.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiosurgery for Cavernous Malformations
- A Potential Risk of Radiation-Induced Cavernous Malformations Following Adjuvant Gamma Knife Radiosurgery for Mesial Temporal Lobe Epilepsy
- Recurrence of pediatric cerebral arteriovenous malformation after obliteration by radiosurgery: a case report
- Gamma Knife Radiosurgery for Pediatric Arteriovenous Malformations
- Radiosurgery for Cerebrovascular Disease