J Korean Med Sci.
2024 Aug;39(31):e243. 10.3346/jkms.2024.39.e243.
COVID-19 and Neurodevelopmental Delays in Early Childhood: A Longitudinal Analysis of Developmental Outcomes in Korean Children
- Affiliations
-
- 1Public Health Research Institute, National Medical Center, Seoul, Korea
- 2Department of Pediatrics, National Medical Center, Seoul, Korea
- 3Department of Pediatrics, Seoul National University Hospital, Seoul, Korea
- 4Department of Preventive Medicine, Konkuk University College of Medicine, Chungju, Korea
- 5National Emergency Medical Center, National Medical Center, Seoul, Korea
- 6Department of Population Health, NYU Grossman School of Medicine, New York, NY, USA
- 7Center for Public Health Data Analytics, National Medical Center, Seoul, Korea
- KMID: 2558526
- DOI: http://doi.org/10.3346/jkms.2024.39.e243
Abstract
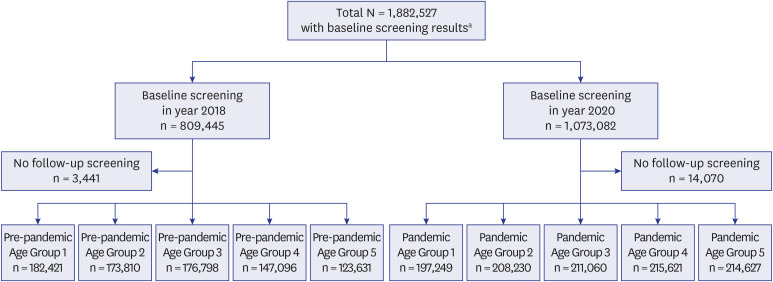
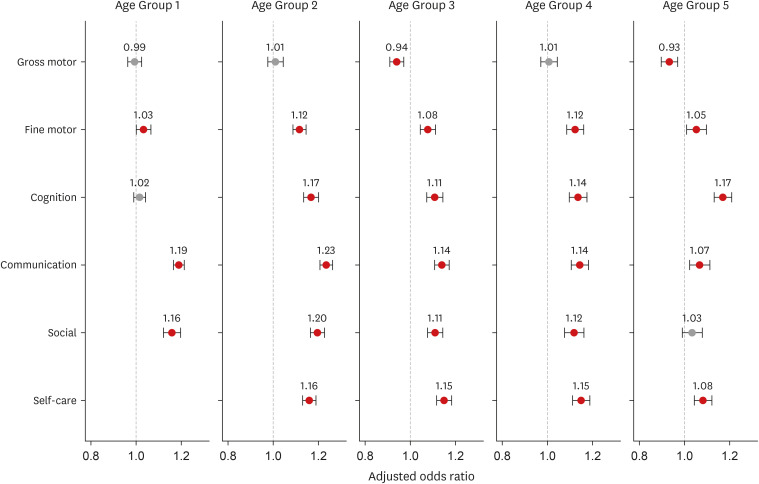
- This study employed a longitudinal analysis to evaluate the association between the coronavirus disease 2019 pandemic and neurodevelopment by analyzing over 1.8 million children from the Korean Developmental Screening Test for Infants and Children included in South Korea’s National Health Screening Program. We compared the developmental outcomes in five age groups—9–17 months, 18–29 months, 30–41 months, 42–53 months, and 54–65 months—between the pre-pandemic (2018–2019) and pandemic (2020–2021) periods. Significant increases in potential developmental delays were observed during the pandemic in communication, cognitive, social interaction, self-care, and fine motor skills across most age groups. All five age groups experienced notable disruptions in communication and fine motor skills. Children from socioeconomically disadvantaged backgrounds faced higher risks across all domains. These findings highlight the need for targeted interventions and continuous monitoring to support the developmental needs of children affected by pandemic-related disruptions.
Keyword
Figure
Reference
-
1. Yoshikawa H, Wuermli AJ, Britto PR, Dreyer B, Leckman JF, Lye SJ, et al. Effects of the global coronavirus disease-2019 pandemic on early childhood development: short- and long-term risks and mitigating program and policy actions. J Pediatr. 2020; 223:188–193. PMID: 32439312.2. Fan Y, Wang H, Wu Q, Zhou X, Zhou Y, Wang B, et al. SARS pandemic exposure impaired early childhood development in China. Sci Rep. 2021; 11(1):8694. PMID: 33888748.3. Araújo LA, Veloso CF, Souza MC, Azevedo JM, Tarro G. The potential impact of the COVID-19 pandemic on child growth and development: a systematic review. J Pediatr (Rio J). 2021; 97(4):369–377. PMID: 32980318.4. Hessami K, Norooznezhad AH, Monteiro S, Barrozo ER, Abdolmaleki AS, Arian SE, et al. COVID-19 pandemic and infant neurodevelopmental impairment: a systematic review and meta-analysis. JAMA Netw Open. 2022; 5(10):e2238941. PMID: 36306133.5. Sato K, Fukai T, Fujisawa KK, Nakamuro M. Association between the COVID-19 pandemic and early childhood development. JAMA Pediatr. 2023; 177(9):930–938. PMID: 37428500.6. Giesbrecht GF, Lebel C, Dennis CL, Silang K, Xie EB, Tough S, et al. Risk for developmental delay among infants born during the COVID-19 pandemic. J Dev Behav Pediatr. 2023; 44(6):e412–e420. PMID: 37491731.7. Ferrari E, Palandri L, Lucaccioni L, Talucci G, Passini E, Trevisani V, et al. The kids are alright (?). Infants’ development and COVID-19 pandemic: a cross-sectional study. Int J Public Health. 2022; 67:1604804. PMID: 35795098.8. Nevo E. The effect of the COVID-19 pandemic on low SES kindergarteners’ language abilities. Early Child Educ J. 2023; 52(3):1–11.9. Tau GZ, Peterson BS. Normal development of brain circuits. Neuropsychopharmacology. 2010; 35(1):147–168. PMID: 19794405.10. Herschkowitz N. Neurological bases of behavioral development in infancy. Brain Dev. 2000; 22(7):411–416. PMID: 11102724.11. Kral A, Sharma A. Developmental neuroplasticity after cochlear implantation. Trends Neurosci. 2012; 35(2):111–122. PMID: 22104561.12. Kral A, Dorman MF, Wilson BS. Neuronal development of hearing and language: cochlear implants and critical periods. Annu Rev Neurosci. 2019; 42(1):47–65. PMID: 30699049.13. Shin DW, Cho B, Guallar E. Korean National Health Insurance Database. JAMA Intern Med. 2016; 176(1):138.14. Kim D, Choe YJ, Durrani BA, Kim E, Byeon J, Eun BL. Korean Developmental Screening Test for Infants and Children (K-DST): development, applications, and implications for future early childhood development interventions. Clin Exp Pediatr. 2023; 66(7):288–293. PMID: 36550771.15. Kim M, Jung W, Kim SY, Park JH, Shin DW. The Korea National Disability Registration System. Epidemiol Health. 2023; 45:e2023053. PMID: 37189275.16. Ballinger GA. Using generalized estimating equations for longitudinal data analysis. Organ Res Methods. 2004; 7(2):127–150.17. Lee KS, Choi YY, Kim YS, Kim Y, Kim MH, Lee N. Association between the COVID-19 pandemic and childhood development aged 30 to 36 months in South Korea, based on the National health screening program for infants and children database. BMC Public Health. 2024; 24(1):989. PMID: 38594741.18. Friedmann N, Rusou D. Critical period for first language: the crucial role of language input during the first year of life. Curr Opin Neurobiol. 2015; 35:27–34. PMID: 26111432.19. Redcay E, Haist F, Courchesne E. Functional neuroimaging of speech perception during a pivotal period in language acquisition. Dev Sci. 2008; 11(2):237–252. PMID: 18333980.20. Gao W, Alcauter S, Elton A, Hernandez-Castillo CR, Smith JK, Ramirez J, et al. Functional network development during the first year: relative sequence and socioeconomic correlations. Cereb Cortex. 2015; 25(9):2919–2928. PMID: 24812084.21. Andersen SL. Trajectories of brain development: point of vulnerability or window of opportunity? Neurosci Biobehav Rev. 2003; 27(1-2):3–18. PMID: 12732219.22. González M, Loose T, Liz M, Pérez M, Rodríguez-Vinçon JI, Tomás-Llerena C, et al. School readiness losses during the COVID-19 outbreak. A comparison of two cohorts of young children. Child Dev. 2022; 93(4):910–924. PMID: 35194777.23. Blanta M, Karathanasi A, Tzonichaki I. The impact of the COVID-19 pandemic on children’s occupations. Hong Kong J Occup Ther. 2023; 36(2):69–83. PMID: 38027048.24. Anderson V, Spencer-Smith M, Wood A. Do children really recover better? Neurobehavioural plasticity after early brain insult. Brain. 2011; 134(Pt 8):2197–2221. PMID: 21784775.25. Martin KC, Ketchabaw WT, Turkeltaub PE. Plasticity of the language system in children and adults. Handb Clin Neurol. 2022; 184:397–414. PMID: 35034751.26. Tooley UA, Bassett DS, Mackey AP. Environmental influences on the pace of brain development. Nat Rev Neurosci. 2021; 22(6):372–384. PMID: 33911229.27. Geweniger A, Barth M, Haddad AD, Högl H, Insan S, Mund A, et al. Impact of the COVID-19 pandemic on mental health outcomes of healthy children, children with special health care needs and their caregivers-results of a cross-sectional study. Front Pediatr. 2022; 10:759066. PMID: 35223688.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neurological Examination after the Newborn Period until 3 Years of Age
- Cognitive outcomes in late childhood and adolescence of neonatal hypoxic-ischemic encephalopathy
- The Seoul Infant Developmental Screening Test
- Analysis of Risk Factors in Children with Suspected Developmental Delays on the Denver Developmental Screening Test
- COVID-19 and diabetes in children