J Korean Med Sci.
2024 Aug;39(31):e222. 10.3346/jkms.2024.39.e222.
Trends in Triptan Usage in Korea: A Population-Based Cohort Study
- Affiliations
-
- 1Department of Neurology, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2558523
- DOI: http://doi.org/10.3346/jkms.2024.39.e222
Abstract
- Background
Migraine presents a significant global health problem that emphasizes the need for efficient acute treatment options. Triptans, introduced in the early 1990s, have substantially advanced migraine management owing to their effectiveness compared to that of traditional medications. However, data on triptan use in migraine management from Asian countries, where migraines tend to have milder symptoms than those in European and North American countries, are limited. This study aimed to identify the trends in triptan usage in Korea.
Methods
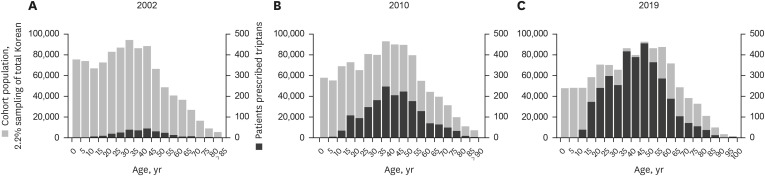
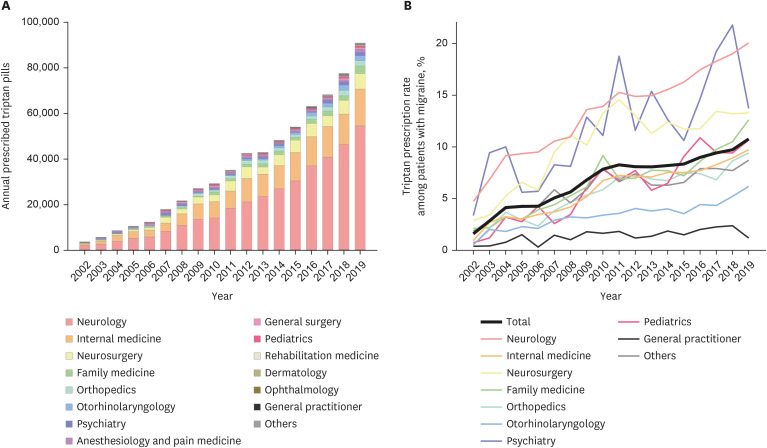
This retrospective cohort study used data from the Korean National Health Insurance Service-National Sample Cohort spanning from 2002 to 2019. Patients with migraine were identified using the International Classification of Diseases 10th revision codes, and triptan prescriptions were evaluated annually in terms of quantity, pills per patient, and associated costs. The distribution of triptan prescriptions across different medical specialties was also examined. Factors contributing to the odds of triptan use were analyzed using multivariable logistic regression.
Results
From 2002 to 2019, the total number of triptan tablets, prescriptions, and patients using triptans increased by 24.0, 17.1, and 13.6 times, respectively, with sumatriptan being the most frequently prescribed type of triptan. Additionally, the number of prescriptions and related costs have consistently increased despite stable pricing because of government regulation. By 2019, only approximately one-tenth of all patients with migraines had been prescribed triptans, although there was a notable increase in prescriptions over the study period. These prescription patterns varied according to the physician’s specialty. After adjusting for patient-specific factors including age and sex, the odds of prescribing triptans were higher for neurologists than for internal medicine physicians (odds ratio 2.875, P < 0.001), while they were lower for general practitioners (odds ratio 0.220, P < 0.001).
Conclusion
The findings revealed an increasing trend in triptan use among individuals with migraines in Korea, aligning with global usage patterns. Despite these increases, the overall prescription rate of triptans remains low, indicating potential underutilization and highlighting the need for improved migraine management strategies across all medical fields. Further efforts are necessary to optimize the use of triptans in treating migraines effectively.
Keyword
Figure
Reference
-
1. Steiner TJ, Stovner LJ, Jensen R, Uluduz D, Katsarava Z. Lifting The Burden: the Global Campaign against Headache. Migraine remains second among the world’s causes of disability, and first among young women: findings from GBD2019. J Headache Pain. 2020; 21(1):137. PMID: 33267788.2. Adams AM, Serrano D, Buse DC, Reed ML, Marske V, Fanning KM, et al. The impact of chronic migraine: the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2015; 35(7):563–578. PMID: 25304766.3. Ryvlin P, Skorobogatykh K, Negro A, Sanchez-De La Rosa R, Israel-Willner H, Sundal C, et al. Current clinical practice in disabling and chronic migraine in the primary care setting: results from the European My-LIFE anamnesis survey. BMC Neurol. 2021; 21(1):1. PMID: 33390161.4. Cady RJ, Shade CL, Cady RK. Advances in drug development for acute migraine. Drugs. 2012; 72(17):2187–2205. PMID: 23116251.5. Tfelt-Hansen P. Sumatriptan for the treatment of migraine attacks--a review of controlled clinical trials. Cephalalgia. 1993; 13(4):238–244. PMID: 8397070.6. Mayans L, Walling A. Acute migraine headache: treatment strategies. Am Fam Physician. 2018; 97(4):243–251. PMID: 29671521.7. Bigal ME, Krymchantowski AV, Ho T. Migraine in the triptan era: progresses achieved, lessons learned and future developments. Arq Neuropsiquiatr. 2009; 67(2B):559–569. PMID: 19623468.8. Xia Y, Kelton CM, Wigle PR, Heaton PC, Guo JJ. Twenty years of triptans in the United States Medicaid programs: utilization and reimbursement trends from 1993 to 2013. Cephalalgia. 2016; 36(14):1305–1315. PMID: 26848128.9. Davidsson OB, Olofsson IA, Kogelman LJ, Andersen MA, Rostgaard K, Hjalgrim H, et al. Twenty-five years of triptans - a nationwide population study. Cephalalgia. 2021; 41(8):894–904. PMID: 33583217.10. Venkataramani AS, O’Brien R, Whitehorn GL, Tsai AC. Economic influences on population health in the United States: toward policymaking driven by data and evidence. PLoS Med. 2020; 17(9):e1003319. PMID: 32877406.11. Takeshima T, Wan Q, Zhang Y, Komori M, Stretton S, Rajan N, et al. Prevalence, burden, and clinical management of migraine in China, Japan, and South Korea: a comprehensive review of the literature. J Headache Pain. 2019; 20(1):111. PMID: 31805851.12. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID: 26822938.13. Nguyen JL, Munshi K, Peasah SK, Swart EC, Kohli M, Henderson R, et al. Trends in utilization and costs of migraine medications, 2017-2020. J Headache Pain. 2022; 23(1):111. PMID: 36031609.14. Peng KP, Wang SJ. Epidemiology of headache disorders in the Asia-pacific region. Headache. 2014; 54(4):610–618. PMID: 24666014.15. Ciulla M, Marinelli L, Di Biase G, Cacciatore I, Santoleri F, Costantini A, et al. Healthcare systems across Europe and the US: the managed entry agreements experience. Healthcare (Basel). 2023; 11(3):447. PMID: 36767022.16. Statistics Korea. Consumer Price Survey (Index). Updated 2024. Accessed April 20, 2024. https://kostat.go.kr/ .17. Lee IH, Bloor K, Hewitt C, Maynard A. The effects of new pricing and copayment schemes for pharmaceuticals in South Korea. Health Policy. 2012; 104(1):40–49. PMID: 22000599.18. Kim BK, Chu MK, Yu SJ, Dell’Agnello G, Han JH, Cho SJ. Burden of migraine and unmet needs from the patients’ perspective: a survey across 11 specialized headache clinics in Korea. J Headache Pain. 2021; 22(1):45. PMID: 34030630.19. The Korean Headache Society. Updated 2023. Accessed April 20, 2024. https://headache.or.kr .20. The Korean Headache Society. The Guideline of Migraine Management in Korea. Seoul, Korea: The Korean Headache Society;2008.21. The Korean Headache Society. The Guideline for Preventive Medications in Episodic Migraine in Korea. Seoul, Korea: The Korean Headache Society;2019.22. Silberstein SD. Preventive treatment of migraine: an overview. Cephalalgia. 1997; 17(2):67–72. PMID: 9137840.23. Amiri P, Kazeminasab S, Nejadghaderi SA, Mohammadinasab R, Pourfathi H, Araj-Khodaei M, et al. Migraine: a review on its history, global epidemiology, risk factors, and comorbidities. Front Neurol. 2022; 12:800605. PMID: 35281991.24. Leroux E, Buchanan A, Lombard L, Loo LS, Bridge D, Rousseau B, et al. Evaluation of patients with insufficient efficacy and/or tolerability to triptans for the acute treatment of migraine: a systematic literature review. Adv Ther. 2020; 37(12):4765–4796. PMID: 32990921.25. Xu H, Han W, Wang J, Li M. Network meta-analysis of migraine disorder treatment by NSAIDs and triptans. J Headache Pain. 2016; 17(1):113. PMID: 27957624.26. Messali AJ, Yang M, Gillard P, Tsai K, Tepper SJ, Bloudek LM, et al. Treatment persistence and switching in triptan users: a systematic literature review. Headache. 2014; 54(7):1120–1130. PMID: 24912394.27. Braunstein D, Donnet A, Pradel V, Sciortino V, Allaria-Lapierre V, Lantéri-Minet M, et al. Triptans use and overuse: a pharmacoepidemiology study from the French health insurance system database covering 4.1 million people. Cephalalgia. 2015; 35(13):1172–1180. PMID: 25667299.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in Epidemiological Trends and Rehabilitation Usage in Neurological Diseases in Korea: Stroke
- Frequency of Humidifier and Humidifier Disinfectant Usage in Gyeonggi Provine
- The Cumulative Effect of Antipsychotic Usage on Mortality in Schizophrenia: A Nationwide Population-based Cohort Study in Korea
- Long Term Trends and the Future Gastric Cancer Mortality in Korea : 1983~2013
- The Diagnosis and Most-Updated Therapy of Migraine