Ann Surg Treat Res.
2024 Aug;107(2):68-80. 10.4174/astr.2024.107.2.68.
Low muscle mass-to-fat ratio is an independent factor that predicts worse overall survival and complications in patients with colon cancer: a retrospective single-center cohort study
- Affiliations
-
- 1Department of General Surgery, the Second Affiliated Hospital of Soochow University, Suzhou, China
- 2Department of Thyroid and Breast Surgery, Suzhou Wuzhong People’s Hospital, Suzhou, China
- KMID: 2558383
- DOI: http://doi.org/10.4174/astr.2024.107.2.68
Abstract
- Purpose
This study was performed to investigate influencing factors of preoperative muscle mass-to-fat ratio (MMFR) and its impact on overall survival and postoperative complications of colon cancer.
Methods
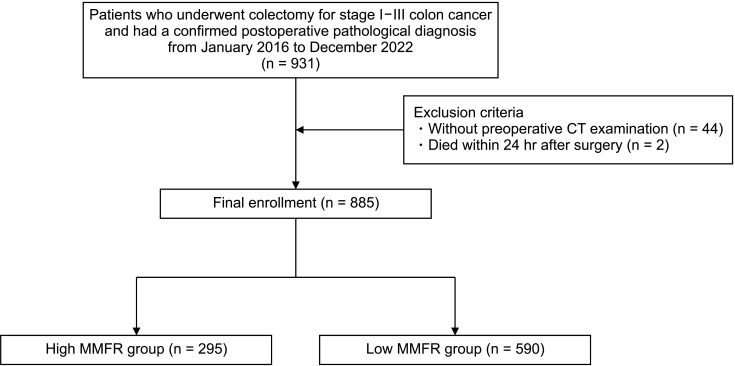
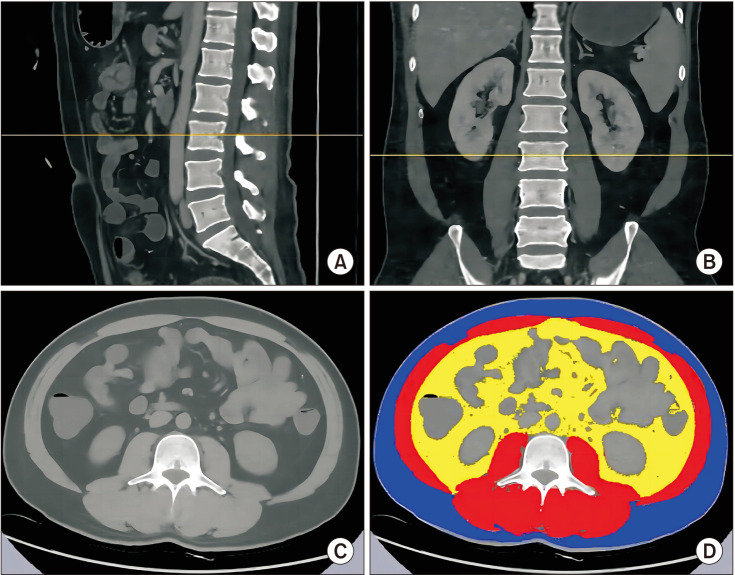
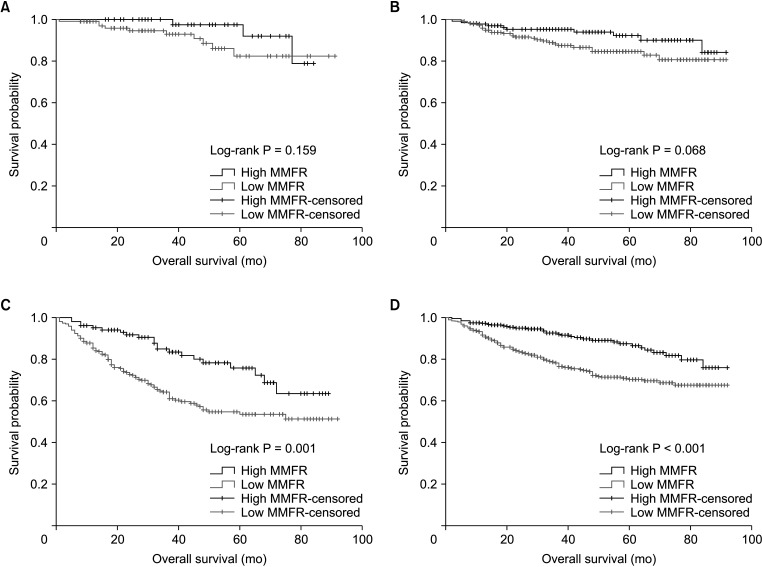
Patients who underwent colectomy for stage I–III colon cancer at the Second Affiliated Hospital of Soochow University between January 2016 and December 2022 were included. The skeletal muscle and fat area at the third lumbar vertebra were measured with preoperative CT measurement. MMFR was defined as the ratio of skeletal muscle area to total fat area, and low MMFR was defined as the 2 lowest tertiles (≤0.585). Univariate and multivariable analyses were conducted to assess the impact of MMFR on overall complications and survival outcomes. Kaplan-Meier survival curves and log-rank test were used to compare the overall survival between high MMFR and low MMFR groups.
Results
A total of 885 patients were analyzed. Female sex, older age, high body mass index, sarcopenia, and high cancer stage were more likely to result in low MMFR. Complications, including intestinal fistula, chylous fistula and organ space surgical site infection were significantly higher in the low MMFR group. Low MMFR was an independent factor associated with overall complications (odds ratio, 1.940; 95% confidence interval [CI], 1.252–3.007; P < 0.01) and long-term survival (hazard ratio, 2.222; 95% CI, 1.443–3.425; P < 0.01). Furthermore, patients with high MMFR had a higher survival rate than patients with low MMFR (P < 0.01).
Conclusion
Low MMFR is an independent factor that predicts worse overall survival and complications in patients with colon cancer.
Keyword
Figure
Reference
-
1. Paik JH, Ryu CG, Hwang DY. Risk factors of recurrence in TNM stage I colorectal cancer. Ann Surg Treat Res. 2023; 104:281–287. PMID: 37179701.2. Dai W, Mo S, Xiang W, Han L, Li Q, Wang R, et al. The critical role of tumor size in predicting prognosis for T1 colon cancer. Oncologist. 2020; 25:244–251. PMID: 32162825.3. Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011; 12:489–495. PMID: 21296615.4. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48:16–31. PMID: 30312372.5. Dodson S, Baracos VE, Jatoi A, Evans WJ, Cella D, Dalton JT, et al. Muscle wasting in cancer cachexia: clinical implications, diagnosis, and emerging treatment strategies. Annu Rev Med. 2011; 62:265–279. PMID: 20731602.6. Güç ZG, Altay C, Özgül HA, Ellidokuz H, Yavuzşen T. GNRI and CONUT scores: simple predictors of sarcopenia in metastatic colorectal cancer patients. Support Care Cancer. 2022; 30:7845–7852. PMID: 35716261.7. Khan AI, Psutka SP, Patil DH, Hong G, Williams MA, Bilen MA, et al. Sarcopenia and systemic inflammation are associated with decreased survival after cytoreductive nephrectomy for metastatic renal cell carcinoma. Cancer. 2022; 128:2073–2084. PMID: 35285950.8. Yamada K, Saito M, Ando M, Abe T, Mukoyama T, Agawa K, et al. Reduced number and immune dysfunction of CD4+ T cells in obesity accelerate colorectal cancer progression. Cells. 2022; 12:86. PMID: 36611881.9. Kim JM, Chung E, Cho ES, Agawa K, Lee JH, Shin SJ, Lee HS, et al. Impact of subcutaneous and visceral fat adiposity in patients with colorectal cancer. Clin Nutr. 2021; 40:5631–5638. PMID: 34662848.10. Brown JC, Caan BJ, Prado CM, Cespedes Feliciano EM, Xiao J, Kroenke CH, et al. The association of abdominal adiposity with mortality in patients with stage I–III colorectal cancer. J Natl Cancer Inst. 2020; 112:377–383. PMID: 31355882.11. Yu PC, Hsu CC, Lee WJ, Liang CK, Chou MY, Lin MH, et al. Muscle-to-fat ratio identifies functional impairments and cardiometabolic risk and predicts outcomes: biomarkers of sarcopenic obesity. J Cachexia Sarcopenia Muscle. 2022; 13:368–376. PMID: 34866342.12. Basile D, Rosati G, Bergamo F, Garattini SK, Banzi M, Zampino M, et al. Prognostic value of body mass index in stage II/III colon cancer: posthoc analysis from the TOSCA trial. Clin Colorectal Cancer. 2023; 22:190–198. PMID: 36935327.13. Gani F, Buettner S, Margonis GA, Sasaki K, Wagner D, Kim Y, et al. Sarcopenia predicts costs among patients undergoing major abdominal operations. Surgery. 2016; 160:1162–1171. PMID: 27302103.14. Zarinsefat A, Terjimanian MN, Sheetz KH, Stein IC, Mazurek AA, Waits SA, et al. Perioperative changes in trunk musculature and postoperative outcomes. J Surg Res. 2014; 191:106–112. PMID: 24750985.15. Murphy N, Jenab M, Gunter MJ. Adiposity and gastrointestinal cancers: epidemiology, mechanisms and future directions. Nat Rev Gastroenterol Hepatol. 2018; 15:659–670. PMID: 29970888.16. Watanabe J, Tatsumi K, Ota M, Suwa Y, Suzuki S, Watanabe A, et al. The impact of visceral obesity on surgical outcomes of laparoscopic surgery for colon cancer. Int J Colorectal Dis. 2014; 29:343–351. PMID: 24297037.17. Lee S, Lee DH, Lee JH, Shin SJ, Lee HS, Park EJ, et al. Association of body mass index with survival in Asian patients with colorectal cancer. Cancer Res Treat. 2022; 54:860–872. PMID: 34665954.18. Hawley SE, Bell ZW, Huang Y, Gibbs JC, Churchward-Venne TA. Evaluation of sex-based differences in resistance exercise training-induced changes in muscle mass, strength, and physical performance in healthy older (≥60 y) adults: a systematic review and meta-analysis. Ageing Res Rev. 2023; 91:102023. PMID: 37507092.19. Janssen I, Heymsfield SB, Wang ZM, Ross R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J Appl Physiol (1985). 2000; 89:81–88. PMID: 10904038.20. Kim HJ, Choi GS. Clinical implications of lymph node metastasis in colorectal cancer: current status and future perspectives. Ann Coloproctol. 2019; 35:109–117. PMID: 31288500.21. Aoyama T, Oba K, Honda M, Sadahiro S, Hamada C, Mayanagi S, et al. Impact of postoperative complications on the colorectal cancer survival and recurrence: analyses of pooled individual patients’ data from three large phase III randomized trials. Cancer Med. 2017; 6:1573–1580. PMID: 28639738.22. Matsubara D, Arita T, Nakanishi M, Kuriu Y, Murayama Y, Kudou M, et al. The impact of postoperative inflammation on recurrence in patients with colorectal cancer. Int J Clin Oncol. 2020; 25:602–613. PMID: 31758273.23. Mungo B, Papageorge CM, Stem M, Molena D, Lidor AO. The impact of operative approach on postoperative complications following colectomy for colon caner. World J Surg. 2017; 41:2143–2152. PMID: 28332057.24. Arron MN, Greijdanus NG, Bastiaans S, Vissers PA, Verhoeven RH, Ten Broek RP, et al. Long-term oncological outcomes after colorectal anastomotic leakage: a retrospective Dutch population-based study. Ann Surg. 2022; 276:882–889. PMID: 35930021.25. He J, He M, Tang JH, Wang XH. Anastomotic leak risk factors following colon cancer resection: a systematic review and meta-analysis. Langenbecks Arch Surg. 2023; 408:252. PMID: 37386211.26. Li Q, An T, Wu J, Lu W, Wang Y, Li J, et al. The impact of sarcopenia on the outcome of patients with left-sided colon and rectal cancer after curative surgery. BMC Cancer. 2023; 23:640. PMID: 37430182.27. Alonso S, Pascual M, Salvans S, Mayol X, Mojal S, Gil MJ, et al. Postoperative intra-abdominal infection and colorectal cancer recurrence: a prospective matched cohort study of inflammatory and angiogenic responses as mechanisms involved in this association. Eur J Surg Oncol. 2015; 41:208–214. PMID: 25468742.28. Feng Z, Pang K, Tian M, Gu X, Lin H, Yang X, et al. Sarcobesity, but not visceral fat, is an independent risk factor for complications after radical resection of colorectal cancer. Front Nutr. 2023; 10:1126127. PMID: 37260520.29. Kim J, Han SH, Kim HI. Detection of sarcopenic obesity and prediction of long-term survival in patients with gastric cancer using preoperative computed tomography and machine learning. J Surg Oncol. 2021; 124:1347–1355. PMID: 34490899.30. Malietzis G, Currie AC, Athanasiou T, Johns N, Anyamene N, Glynne-Jones R, et al. Influence of body composition profile on outcomes following colorectal cancer surgery. Br J Surg. 2016; 103:572–580. PMID: 26994716.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associations Between Trunk Muscle/Fat Composition, Narrowing Lumbar Disc Space, and Low Back Pain in Middle-Aged Farmers: A Cross-Sectional Study
- Prognostic Factor and Survival Benefit of Adjuvant Chemotherapy in Stage IIA Colon Cancer
- The Impact of Preoperative Low Body Mass Index on Postoperative Complications and Long-term Survival Outcomes in Gastric Cancer Patients
- Association of Chest CT-Based Quantitative Measures of Muscle and Fat with Post-Lung Transplant Survival and Morbidity: A Single Institutional Retrospective Cohort Study in Korean Population
- Clinical impact of sarcopenia in patients with colon cancer undergoing laparoscopic surgery