Healthc Inform Res.
2024 Jul;30(3):224-233. 10.4258/hir.2024.30.3.224.
Associations between Nicotine Dependence, Smartphone Usage Patterns, and Expected Compliance with a Smoking Cessation Application among Smokers
- Affiliations
-
- 1Department of Internal Medicine, Kangwon National University Hospital, Chuncheo, Korea
- 2Schema Labs Inc., Chuncheon, Korea
- 3Department of Computer Science and Engineering, Kangwon National University, Chuncheon, Korea
- 4Department of Medical Informatics, Kangwon National University School of Medicine, Chuncheon, Korea
- 5Institute of Medical Science, Kangwon National University School of Medicine, Chuncheon, Korea
- 6Department of Data Science, Weknew Co. Ltd., Chuncheon, Korea
- 7Department of Neuropsychiatry, Kangwon National University Hospital, Chuncheon, Korea
- 8Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea
- KMID: 2558318
- DOI: http://doi.org/10.4258/hir.2024.30.3.224
Abstract
Objectives
Smoking remains the leading cause of preventable disease. However, smokers have shown poor compliance with smoking cessation clinics. Smartphone applications present a promising opportunity to improve this compliance. This study aimed to explore the relationship between nicotine dependence, smartphone usage patterns, and anticipated compliance with a smoking cessation application among smokers, with the goal of informing future development of such applications.
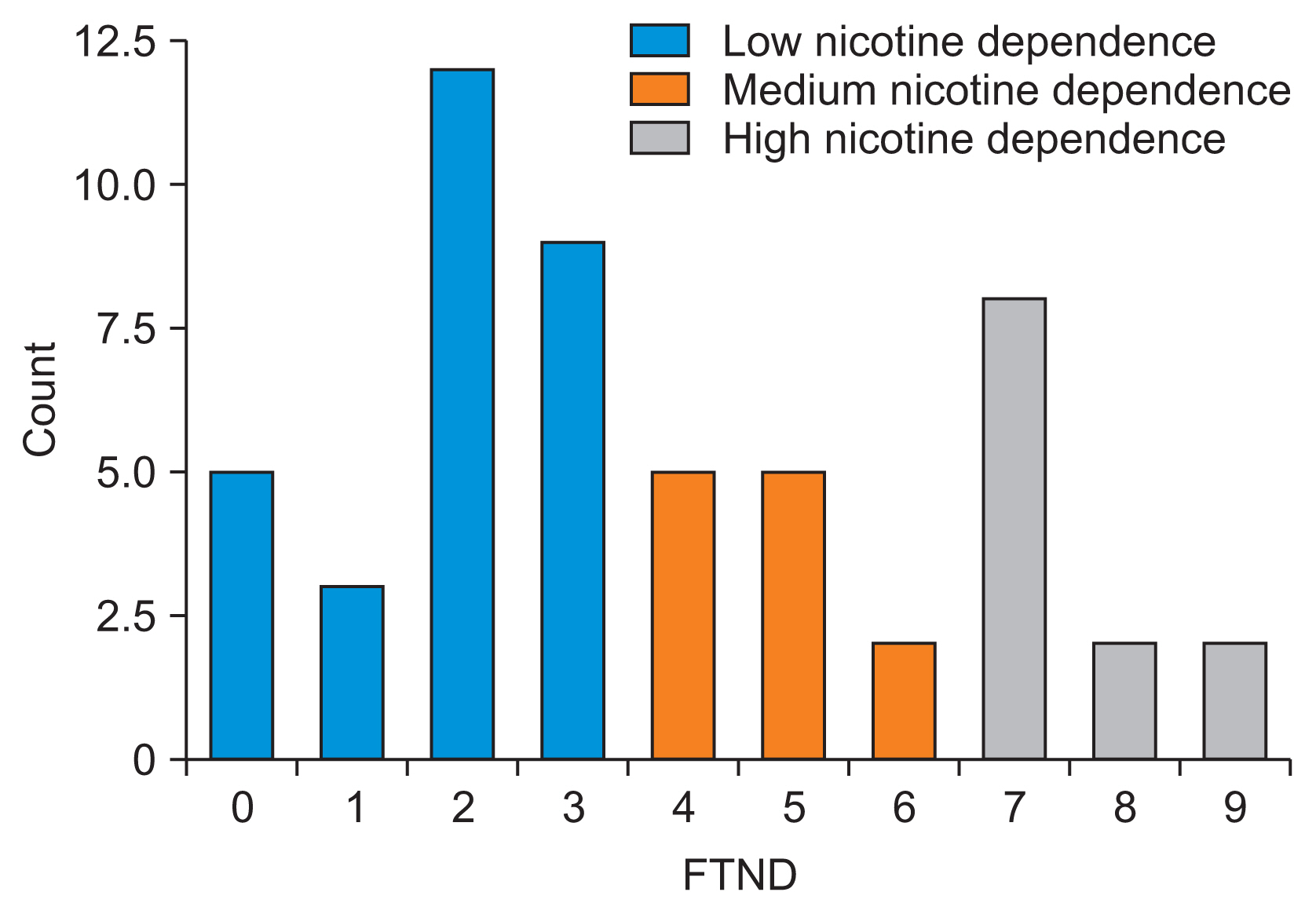
Methods
A total of 53 current smokers were surveyed using a questionnaire. Nicotine dependence was assessed using the Fagerstrom Test for Nicotine Dependence (FTND). Variables included the number of hours spent using a phone, willingness to quit smoking, number of previous quit attempts, desired number of text messages about smoking cessation, expected duration of application usage, and FTND scores. Kendall’s partial correlation, adjusted for age, was employed for the analysis.
Results
The amount of time smokers spent on their mobile devices was negatively correlated with the number of smoking cessation text messages they wanted to receive (τ coefficient = –0.210, p = 0.026) and the duration they intended to use the cessation application (τ coefficient = –0.260, p = 0.006). Conversely, the number of desired text messages was positively correlated with the intended duration of application usage (τ coefficient = 0.366, p = 0.00012).
Conclusions
Smokers who spent more time on their mobile devices tended to prefer using the cessation application for shorter periods, whereas those who desired more text messages about smoking cessation were more inclined to use the application for longer durations.
Keyword
Figure
Reference
-
References
1. US Centers for Disease Control and Prevention. Current cigarette smoking among adults in the United States [Internet]. Atlanta, GA: Centers for Disease Control and Prevention;2023. [cited at 2024 Jul 10]. Available from: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm.2. Institute for Health Metrics and Evaluation. Smoking and tobacco [Internet]. Seattle, WA: Institute for Health Metrics and Evaluation;c2024. [cited at 2024 Jul 10]. Available from: https://www.healthdata.org/researchanalysis/health-risks-issues/smoking-and-tobacco.3. World Health Organization. WHO report on the global tobacco epidemic, 2017: monitoring tobacco use and prevention policies [Internet]. Geneva, Switzerland: World Health Organization;2017. [cited at 2024 Jul 10]. Available from: https://www.who.int/publications/i/item/9789241512824.4. World Health Organization. WHO global report on trends in prevalence of tobacco use 2000–2025, fourth edition [Internet]. Geneva, Switzerland: World Health Organization;2021. [cited at 2024 Jul 10]. Available from: https://www.who.int/publications/i/item/9789240039322.5. US Department of Health and Human Services. Smoking cessation: a report of the surgeon general [Internet]. Rockville (MD): US Department of Health and Human Services;2020. [cited at 2024 Jul 10]. Available from: https://www.hhs.gov/sites/default/files/2020-cessationsgr-full-report.pdf.6. Chean KY, Goh LG, Liew KW, Tan CC, Choi XL, Tan KC, et al. Barriers to smoking cessation: a qualitative study from the perspective of primary care in Malaysia. BMJ Open. 2019; 9(7):e025491. https://doi.org/10.1136/bmjopen-2018-025491.
Article7. Benowitz NL. Nicotine addiction. N Engl J Med. 2010; 362(24):2295–303. https://doi.org/10.1056/NEJMra0809890.
Article8. Rollema H, Chambers LK, Coe JW, Glowa J, Hurst RS, Lebel LA, et al. Pharmacological profile of the alpha4beta2 nicotinic acetylcholine receptor partial agonist varenicline, an effective smoking cessation aid. Neuropharmacology. 2007; 52(3):985–94. https://doi.org/10.1016/j.neuropharm.2006.10.016.
Article9. DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004; 42(3):200–9. https://doi.org/10.1097/01.mlr.0000114908.90348.f9.
Article10. Iacoviello BM, Steinerman JR, Klein DB, Silver TL, Berger AG, Luo SX, et al. Clickotine, a personalized smartphone app for smoking cessation: initial evaluation. JMIR Mhealth Uhealth. 2017; 5(4):e56. https://doi.org/10.2196/mhealth.7226.11. Yu SH, Kim MJ, Jeon J, Park HK, Hwang HS, Park KY. Short-term success rates of smoking cessation support programs and factors predicting smoking relapse: using data from a smoking cessation clinic in a hospital. Korean J Fam Med. 2019; 40(6):373–9. https://doi.org/10.4082/kjfm.18.0094.
Article12. Oh SW. The current status and challenges of national smoking cessation support program in Korea. Korean J Fam Med. 2019; 40(6):351–2. https://doi.org/10.4082/kjfm.40.6E.
Article13. Rajani NB, Bustamante L, Weth D, Romo L, Mastellos N, Filippidis FT. Engagement with gamification elements in a smoking cessation app and short-term smoking abstinence: quantitative assessment. JMIR Serious Games. 2023; 11:e39975. https://doi.org/10.2196/39975.
Article14. Borrelli B, Bartlett YK, Tooley E, Armitage CJ, Wearden A. Prevalence and Frequency of mHealth and eHealth Use Among US and UK Smokers and Differences by Motivation to Quit. J Med Internet Res. 2015; 17(7):e164. https://doi.org/10.2196/jmir.4420.
Article15. Tobacco Use and Dependence Guideline Panel. Treating Tobacco Use and Dependence: 2008 Update. Rockville (MD): US Department of Health and Human Services;2008. [cited at 2024 Jul 10]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK63952/.16. Zeng EY, Heffner JL, Copeland WK, Mull KE, Bricker JB. Get with the program: adherence to a smartphone app for smoking cessation. Addict Behav. 2016; 63:120–4. https://doi.org/10.1016/j.addbeh.2016.07.007.
Article17. Becker S, Kribben A, Meister S, Diamantidis CJ, Unger N, Mitchell A. User profiles of a smartphone application to support drug adherence: experiences from the iNephro project. PLoS One. 2013; 8(10):e78547. https://doi.org/10.1371/journal.pone.0078547.
Article18. Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991; 86(9):1119–27. https://doi.org/10.1111/j.1360-0443.1991.tb01879.x.
Article19. Eum YH, Kim HJ, Bak S, Lee SH, Kim J, Park SH, et al. Factors related to the success of smoking cessation: a retrospective cohort study in Korea. Tob Induc Dis. 2022; 20:15. https://doi.org/10.18332/tid/144272.
Article20. Nazari E, Asgari P, Aghemiri M, Shahriari MH, Zangeneh A, Tabesh H. Developing a questionnaire for mobile phone usage pattern among university students using the Delphi method. Front Health Inf. 2021; 10(1):52. https://doi.org/10.30699/fhi.v10i1.241.
Article21. Jafari A, Peyman N, Gholian-Aval M, Mahdizadeh M, Tehrani H. Design and evaluation of psychometric properties of cigarette smoking tendency questionnaire for female adolescents (CTQFA). BMC Public Health. 2021; 21(1):1746. https://doi.org/10.1186/s12889-021-11784-8.
Article22. Borland R, Yong HH, O’Connor RJ, Hyland A, Thompson ME. The reliability and predictive validity of the Heaviness of Smoking Index and its two components: findings from the International Tobacco Control Four Country study. Nicotine Tob Res. 2010; 12:Suppl. S45–50. https://doi.org/10.1093/ntr/ntq038.
Article23. Shankar D, Borrelli B, Cobb V, Quintiliani LM, Palfai T, Weinstein Z, et al. Text-messaging to promote smoking cessation among individuals with opioid use disorder: quantitative and qualitative evaluation. BMC Public Health. 2022; 22(1):668. https://doi.org/10.1186/s12889-022-13008-z.
Article24. Cummings KM, Jaen CR, Giovino G. Circumstances surrounding relapse in a group of recent exsmokers. Prev Med. 1985; 14:195–202. https://doi.org/10.1016/0091-7435(85)90035-0.
Article25. Timilsina JK, Bhatta B, Devkota A. Nicotine dependence and quitting stages of smokers in Nepal: a community based cross-sectional study. PLoS One. 2022; 17(4):e0266661. https://doi.org/10.1371/journal.pone.0266661.
Article26. Kim SJ, Chae W, Park WH, Park MH, Park EC, Jang SI. The impact of smoking cessation attempts on stress levels. BMC Public Health. 2019; 19(1):267. https://doi.org/10.1186/s12889-019-6592-9.
Article27. Spears CA, Bell SA, Scarlett CA, Anderson NK, Cottrell-Daniels C, Lotfalian S, et al. Text messaging to enhance mindfulness-based smoking cessation treatment: program development through qualitative research. JMIR Mhealth Uhealth. 2019; 7(1):e11246. https://doi.org/10.2196/11246.
Article28. Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across life course. Annu Rev Sociol. 2010; 36:139–57. https://doi.org/10.1146/annurevsoc-070308-120011.
Article29. Lee DG, Lee S, Park HJ. Validation of the Korean version of the Locus of Evaluation Inventory. Korean J Counsel Psychother. 2008; 20(1):65–82.30. Shoukat S. Cell phone addiction and psychological and physiological health in adolescents. EXCLI J. 2019; 18:47–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of a Smoking Cessation Program on Amount of Smoking and Nicotine Dependence and Self-efficacy of Smoking Cessation for Smoking Workers
- Cigarette Smoking, Stage of Smoking Cessation, Nicotine Dependency, and Urine Nicotine Among Smoking Adults with Diabetes
- Pharmacotherpy of Smoking Cessation
- The factors associated with success of smoking cessation at smoking-cessation clinic
- Pharmacotherapy of Nicotine Dependence