Healthc Inform Res.
2024 Jul;30(3):206-223. 10.4258/hir.2024.30.3.206.
Satisfaction of Patients and Physicians with Telehealth Services during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Telemedicine Research Center, National Research Institute of Tuberculosis and Lung Diseases (NRITLD), Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 2Social Determinants of Health Research Center, Birjand University of Medical Sciences, Birjand, Iran
- KMID: 2558317
- DOI: http://doi.org/10.4258/hir.2024.30.3.206
Abstract
Objectives
The rapid spread of coronavirus disease 2019 (COVID-19) posed significant challenges to healthcare systems, prompting the widespread adoption of telehealth to provide medical services while minimizing the risk of virus transmission. This study aimed to assess the satisfaction rates of both patients and physicians with telehealth during the COVID-19 pandemic.
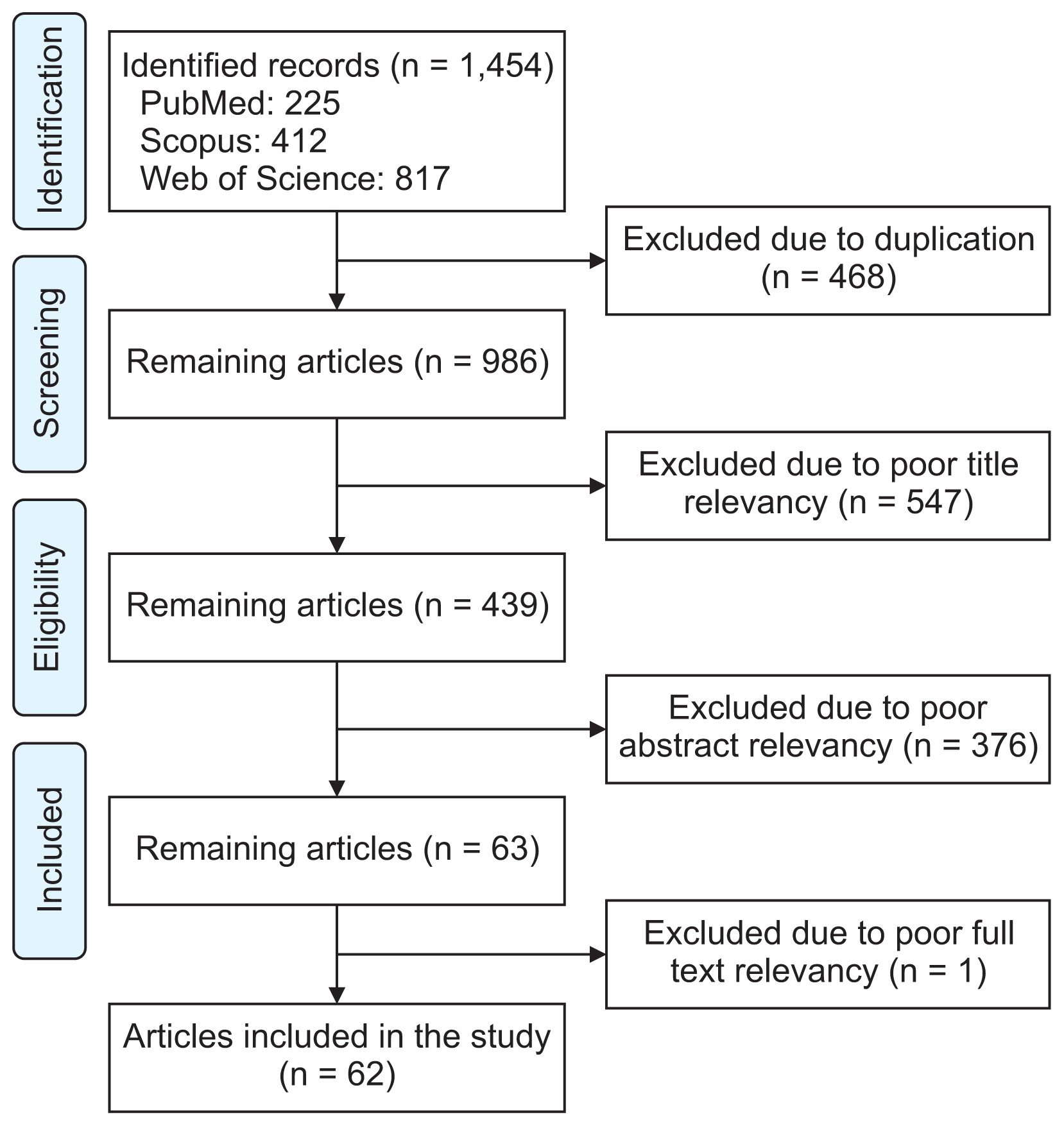
Methods
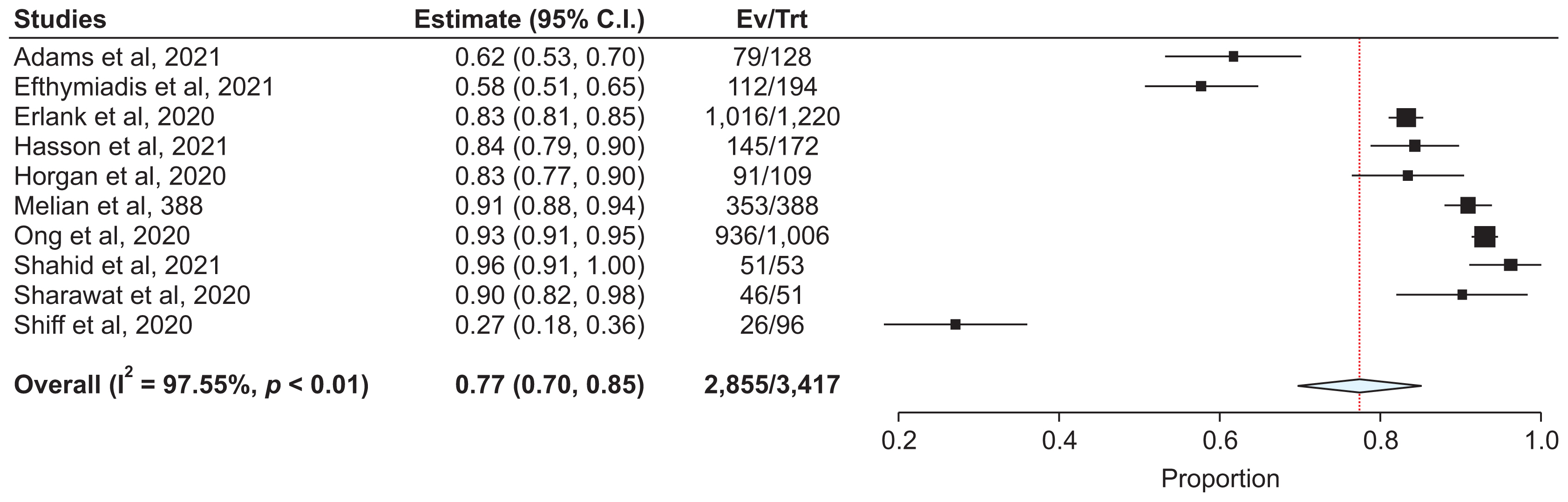
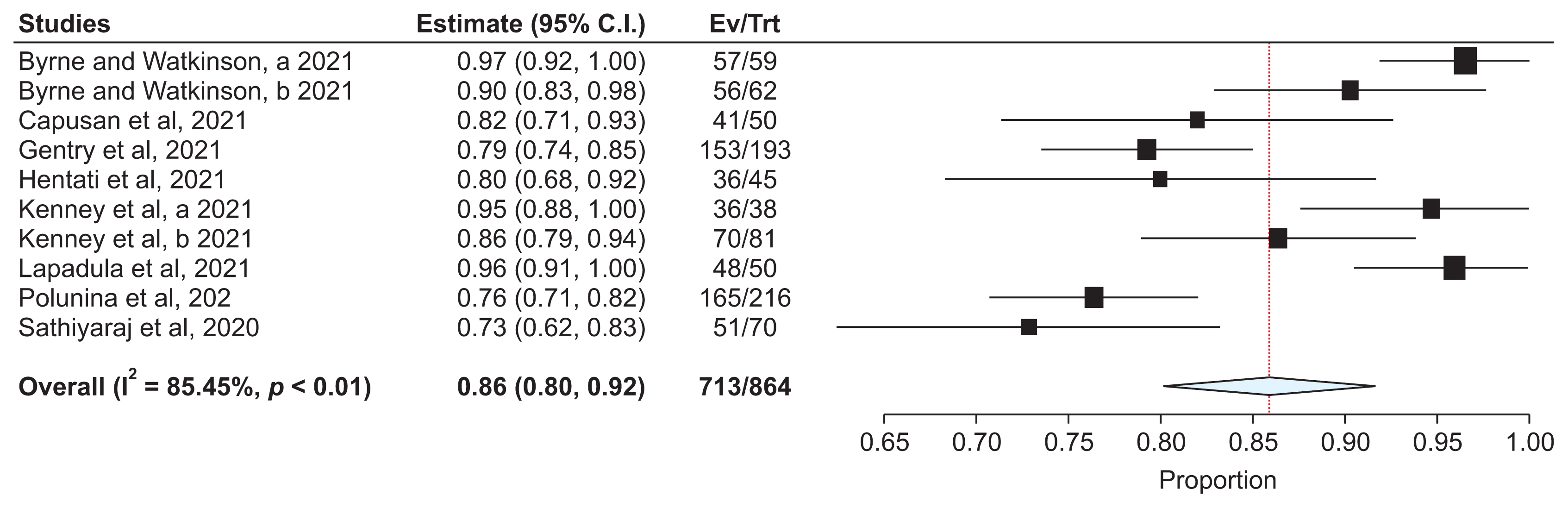
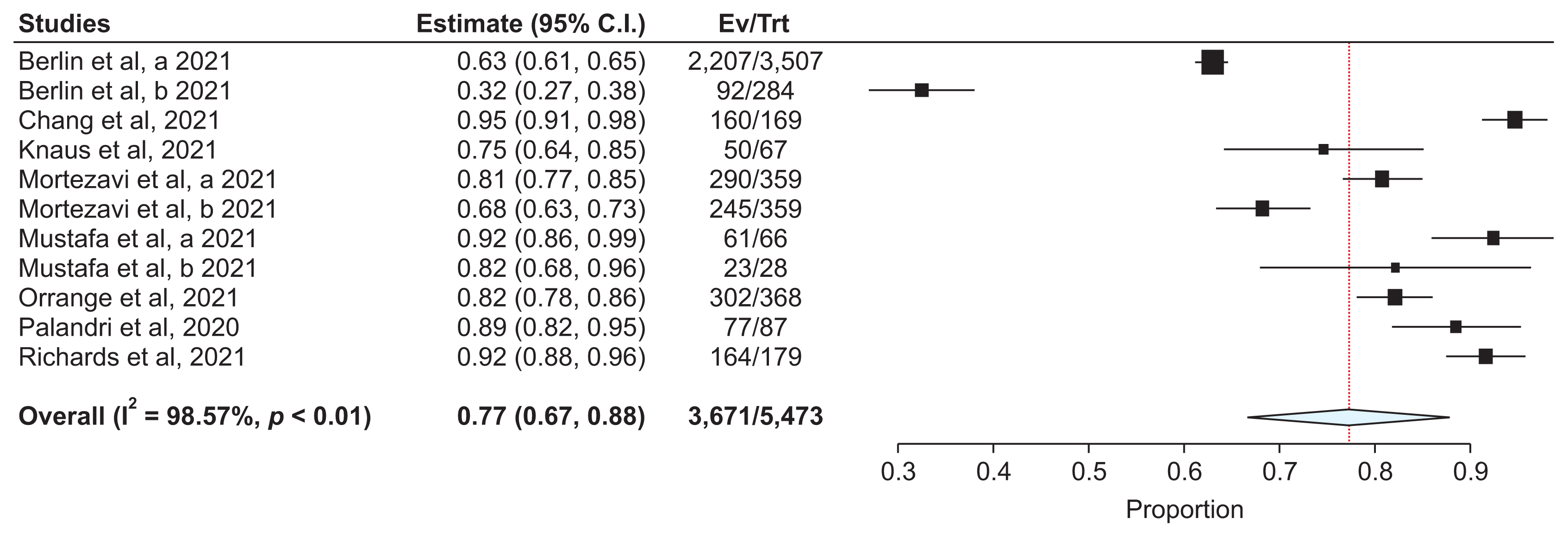
Searches were conducted in the Web of Science, PubMed, and Scopus databases from January 1, 2020, to January 1, 2023. We included studies that utilized telehealth during the COVID-19 pandemic and reported satisfaction data for both patients and physicians. Data extraction was performed using a form designed by the researchers. A meta-analysis was carried out using random-effects models with the OpenMeta-Analyst software. A subgroup analysis was conducted based on the type of telehealth services used: telephone, video, and a combination of both.
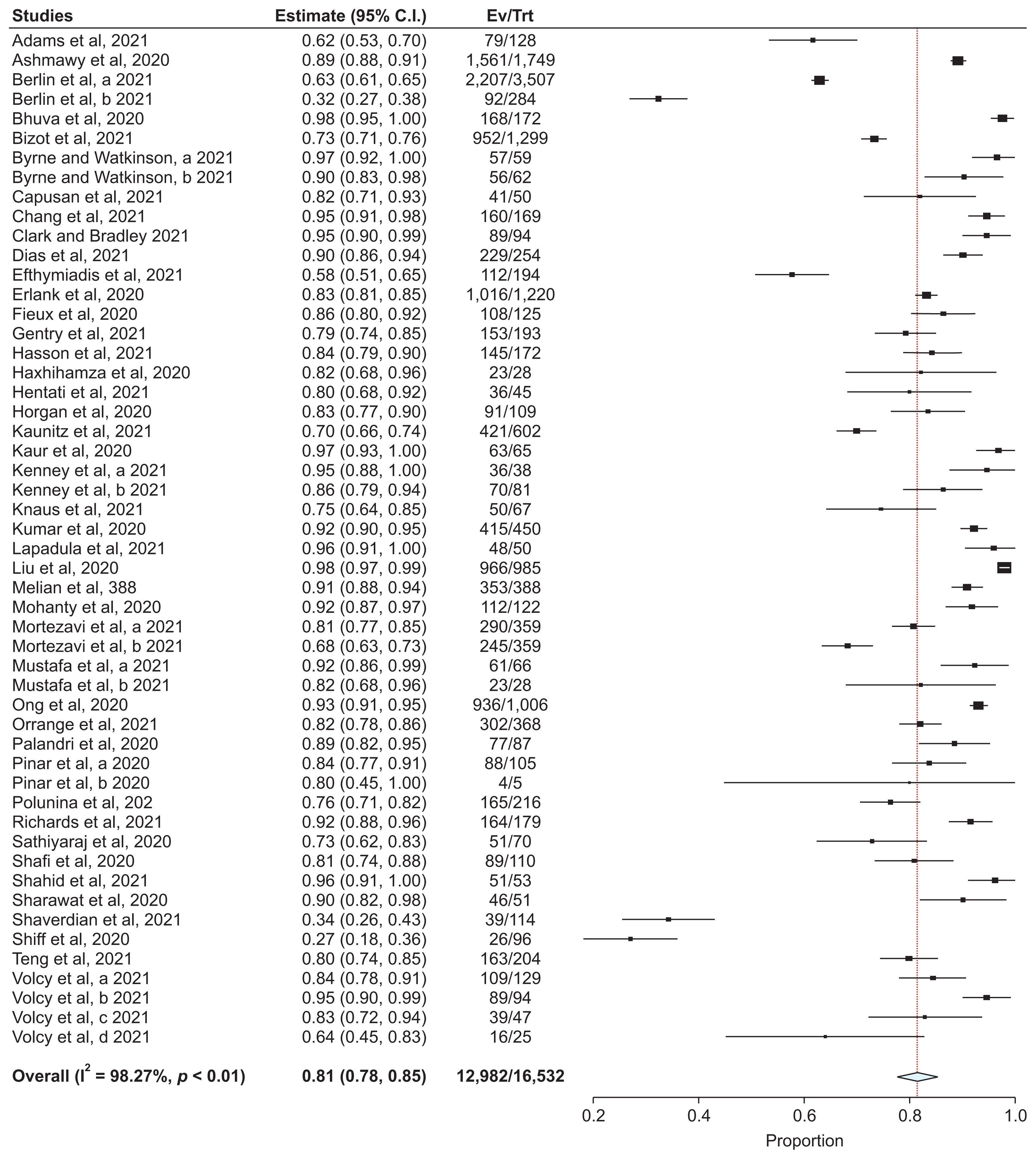
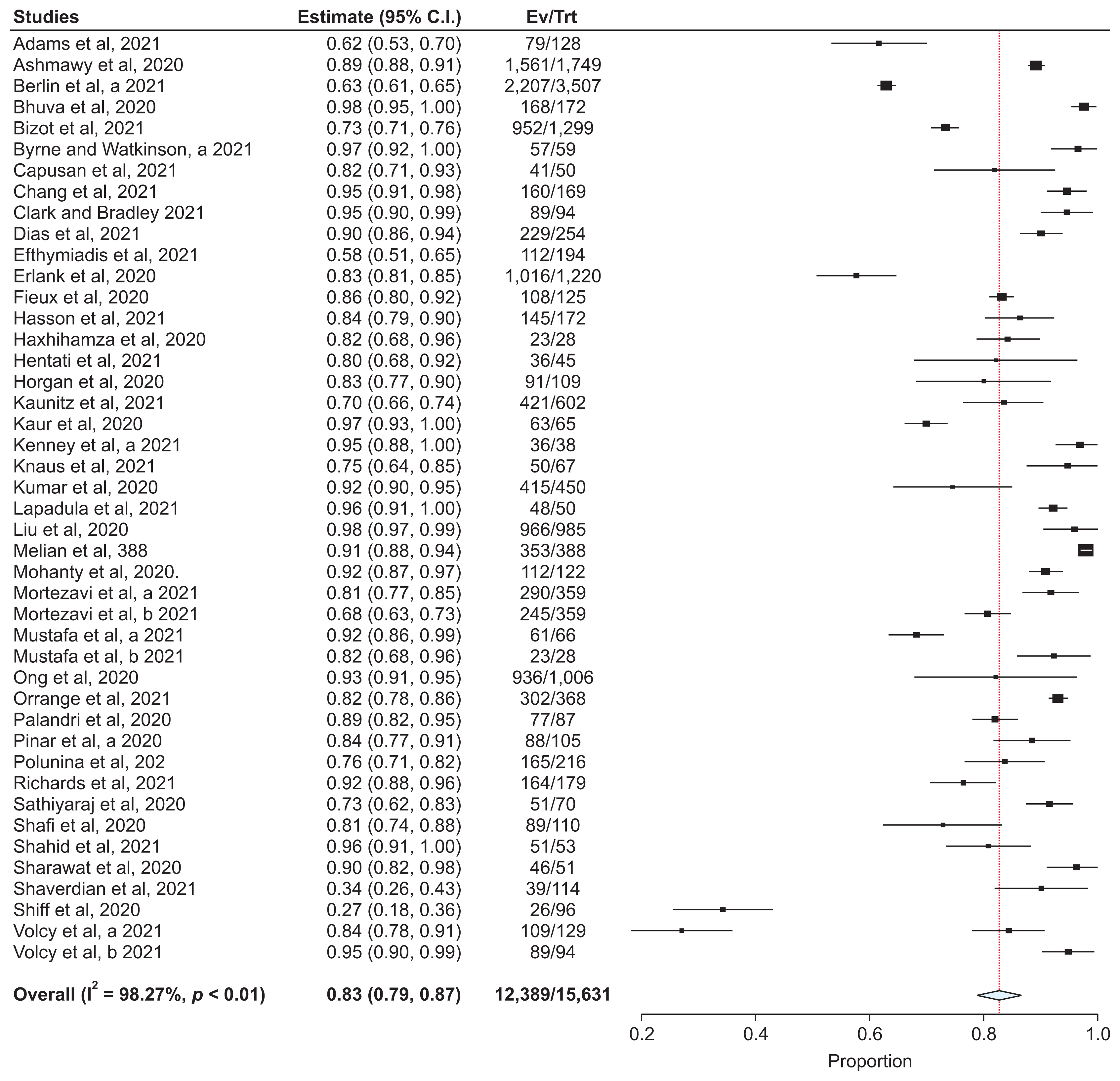
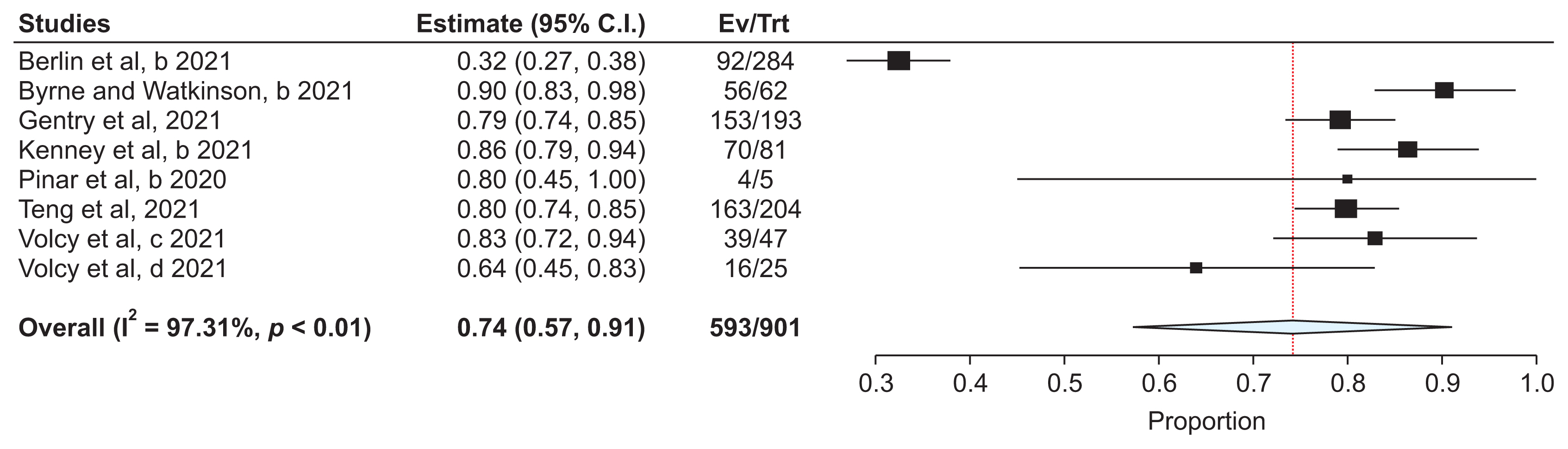
Results
From an initial pool of 1,454 articles, 62 met the inclusion criteria for this study. The most commonly used methods were video and telephone calls. The overall satisfaction rate with telehealth during the COVID-19 pandemic was 81%. Satisfaction rates were higher among patients at 83%, compared to 74% among physicians. Specifically, telephone consultations had a satisfaction rate of 77%, video consultations 86%, and a mix of both methods yielded a 77% satisfaction rate.
Conclusions
Overall, satisfaction with telehealth during the COVID-19 pandemic was considered satisfactory, with both patients and physicians reporting high levels of satisfaction. Telehealth has proven to be an effective alternative for delivering healthcare services during pandemics.
Figure
Reference
-
References
1. Gilbert AW, Billany JC, Adam R, Martin L, Tobin R, Bagdai S, et al. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual. 2020; 9(2):e000985. https://doi.org/10.1136/bmjoq-2020-000985.
Article2. Gentry MT, Puspitasari AJ, McKean AJ, Williams MD, Breitinger S, Geske JR, et al. Clinician satisfaction with rapid adoption and implementation of telehealth services during the COVID-19 pandemic. Telemed J E Health. 2021; 27(12):1385–92. https://doi.org/10.1089/tmj.2020.0575.
Article3. Andrews E, Berghofer K, Long J, Prescott A, Caboral-Stevens M. Satisfaction with the use of telehealth during COVID-19: an integrative review. Int J Nurs Stud Adv. 2020; 2:100008. https://doi.org/10.1016/j.ijnsa.2020.100008.
Article4. Harkey LC, Jung SM, Newton ER, Patterson A. Patient satisfaction with telehealth in rural settings: a systematic review. Int J Telerehabil. 2020; 12(2):53–64. https://doi.org/10.5195/ijt.2020.6303.
Article5. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015; 4(1):1. https://doi.org/10.1186/2046-4053-4-1.
Article6. Jung AR, Kim D, Park EA. Cognitive intervention using information and communication technology for older adults with mild cognitive impairment: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021; 18(21):11535. https://doi.org/10.3390/ijerph182111535.
Article7. Hadeler E, Gitlow H, Nouri K. Definitions, survey methods, and findings of patient satisfaction studies in teledermatology: a systematic review. Arch Dermatol Res. 2021; 313(4):205–15. https://doi.org/10.1007/s00403-020-02110-0.
Article8. Barker TH, Stone JC, Sears K, Klugar M, Leonardi-Bee J, Tufanaru C, et al. Revising the JBI quantitative critical appraisal tools to improve their applicability: an overview of methods and the development process. JBI Evid Synth. 2023; 21(3):478–93. https://doi.org/10.11124/JBIES-22-00125.
Article9. Wallace BC, Schmid CH, Lau J, Trikalinos TA. Meta-Analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol. 2009; 9:80. https://doi.org/10.1186/1471-2288-9-80.
Article10. Jackson D, White IR, Thompson SG. Extending DerSimonian and Laird’s methodology to perform multivariate random effects meta-analyses. Stat Med. 2010; 29(12):1282–97. https://doi.org/10.1002/sim.3602.
Article11. Lin L. Comparison of four heterogeneity measures for meta-analysis. J Eval Clin Pract. 2020; 26(1):376–84. https://doi.org/10.1111/jep.13159.
Article12. Pogorzelska K, Chlabicz S. Patient satisfaction with telemedicine during the COVID-19 pandemic-a systematic review. Int J Environ Res Public Health. 2022; 19(10):6113. https://doi.org/10.3390/ijerph19106113.
Article13. Hoff T, Lee DR. Physician satisfaction with telehealth: a systematic review and agenda for future research. Qual Manag Health Care. 2022; 31(3):160–9. https://doi.org/10.1097/QMH.0000000000000359.
Article14. Aashima , Nanda M, Sharma R. A review of patient satisfaction and experience with telemedicine: a virtual solution during and beyond COVID-19 pandemic. Telemed J E Health. 2021; 27(12):1325–31. https://doi.org/10.1089/tmj.2020.0570.
Article15. Saiyed S, Nguyen A, Singh R. Physician perspective and key satisfaction indicators with rapid telehealth adoption during the coronavirus disease 2019 pandemic. Telemed J E Health. 2021; 27(11):1225–34. https://doi.org/10.1089/tmj.2020.0492.
Article16. Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020; 20(1):1193. https://doi.org/10.1186/s12889-020-09301-4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patient Perception of Telehealth Services for Breast and Gynecologic Oncology Care during the COVID-19 Pandemic: A Single Center Surveybased Study
- The Prevalence of Post-Traumatic Stress Disorder in the General Population during the COVID-19 Pandemic: A Systematic Review and Single-Arm Meta-Analysis
- Depression in pregnant and postpartum women during COVID-19 pandemic: systematic review and meta-analysis
- A Scoping Review on the Expected Role of Community Pharmacists in the Era of COVID-19 Pandemic Crisis Across OECD Countries
- Epidemiology and Outcome of Out-of-Hospital Cardiac Arrests during the COVID-19 Pandemic in South Korea: A Systematic Review and Meta-Analyses