Healthc Inform Res.
2024 Jul;30(3):184-193. 10.4258/hir.2024.30.3.184.
Evolving Software Architecture Design in Telemedicine: A PRISMA-based Systematic Review
- Affiliations
-
- 1School of Economics, Innovation, and Technology, Kristiania University College, Oslo, Norway
- 2Department of Computer Science, Brunel University, Uxbridge, UK
- KMID: 2558315
- DOI: http://doi.org/10.4258/hir.2024.30.3.184
Abstract
Objectives
This article presents a systematic review of recent advancements in telemedicine architectures for continuous monitoring, providing a comprehensive overview of the evolving software engineering practices underpinning these systems. The review aims to illuminate the critical role of telemedicine in delivering healthcare services, especially during global health crises, and to emphasize the importance of effectiveness, security, interoperability, and scalability in these systems.
Methods
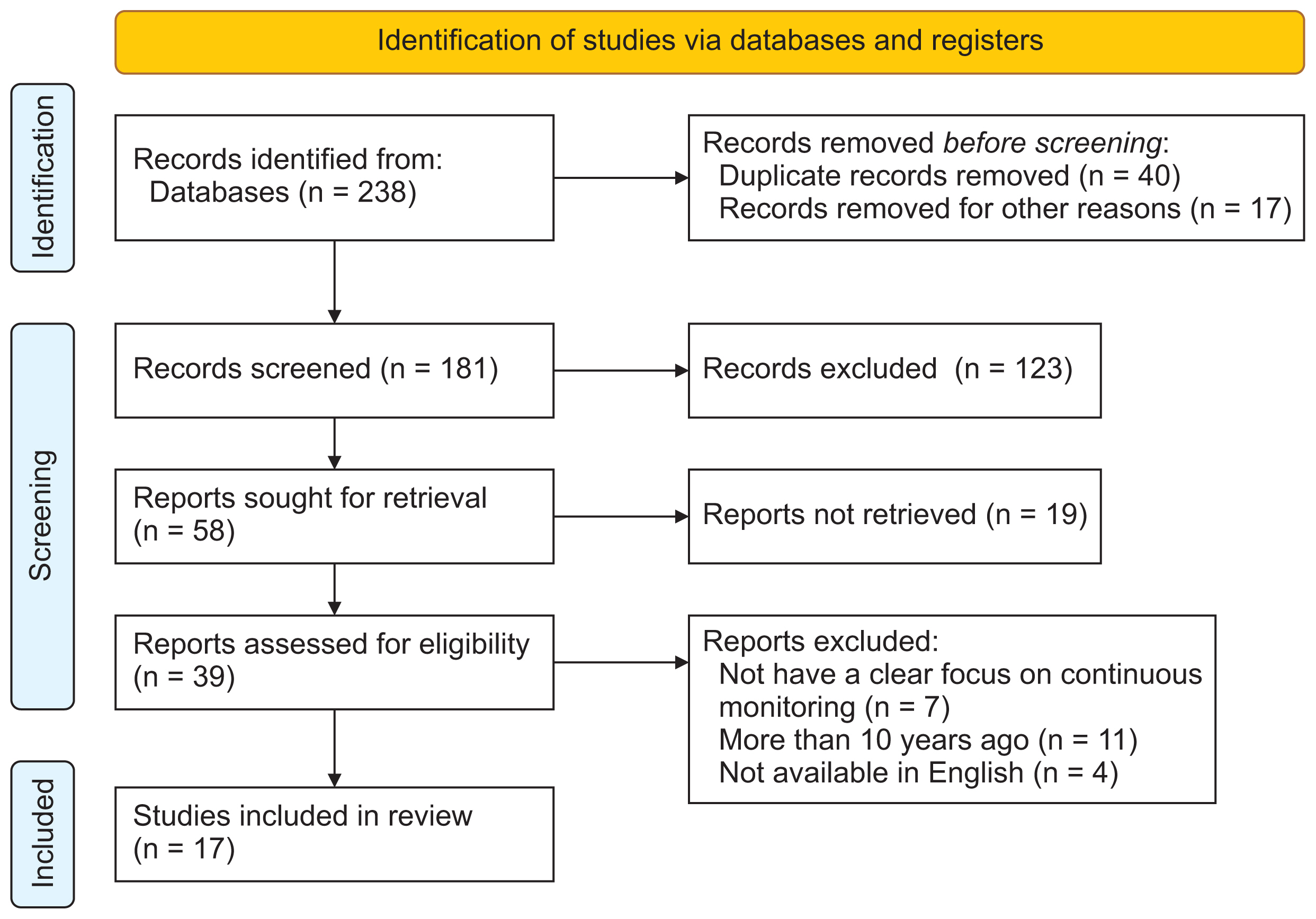
A systematic review methodology was employed, adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses framework. As the primary research method, the PubMed, IEEE Xplore, and Scopus databases were searched to identify articles relevant to telemedicine architectures for continuous monitoring. Seventeen articles were selected for analysis, and a methodical approach was employed to investigate and synthesize the findings.
Results
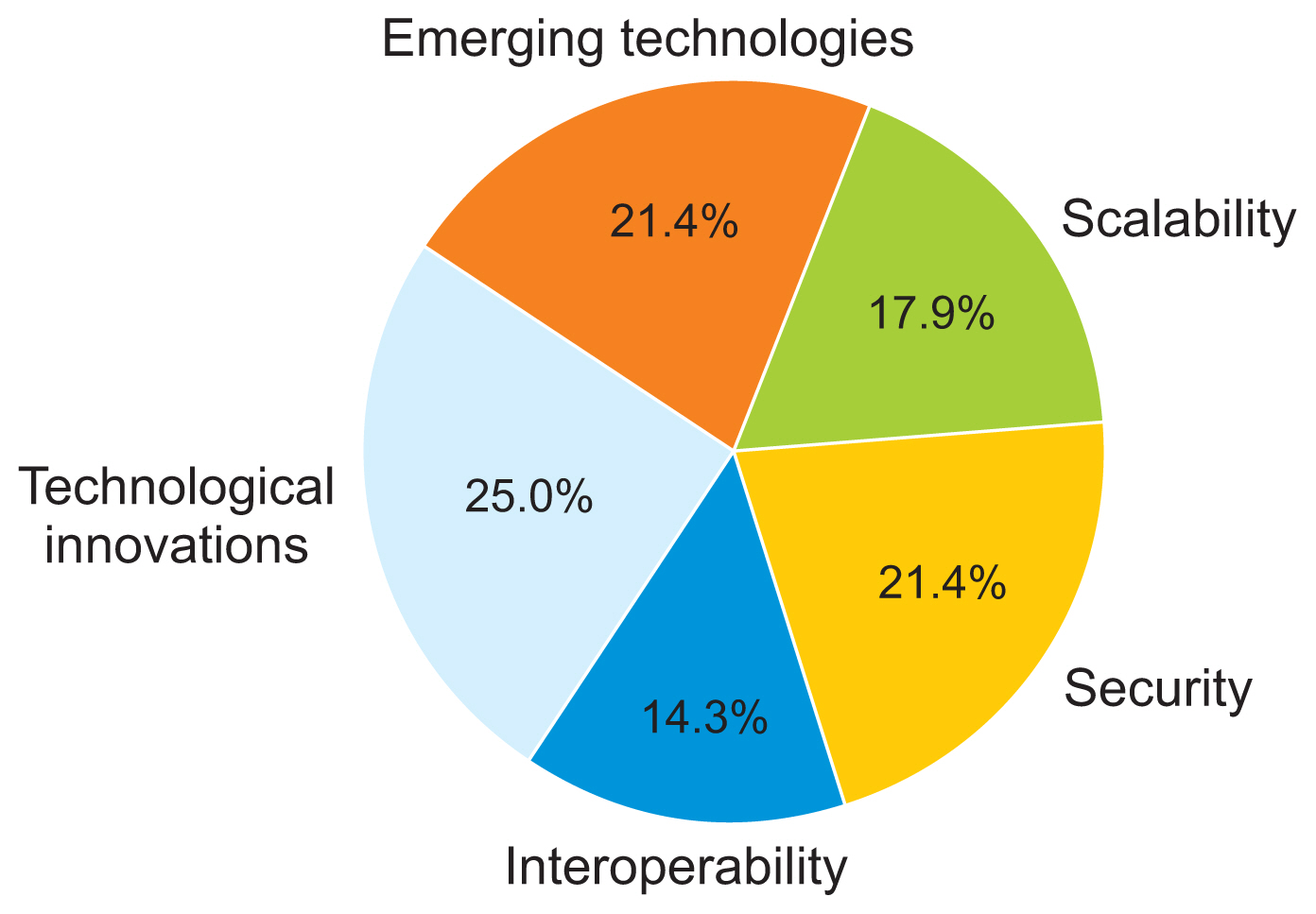
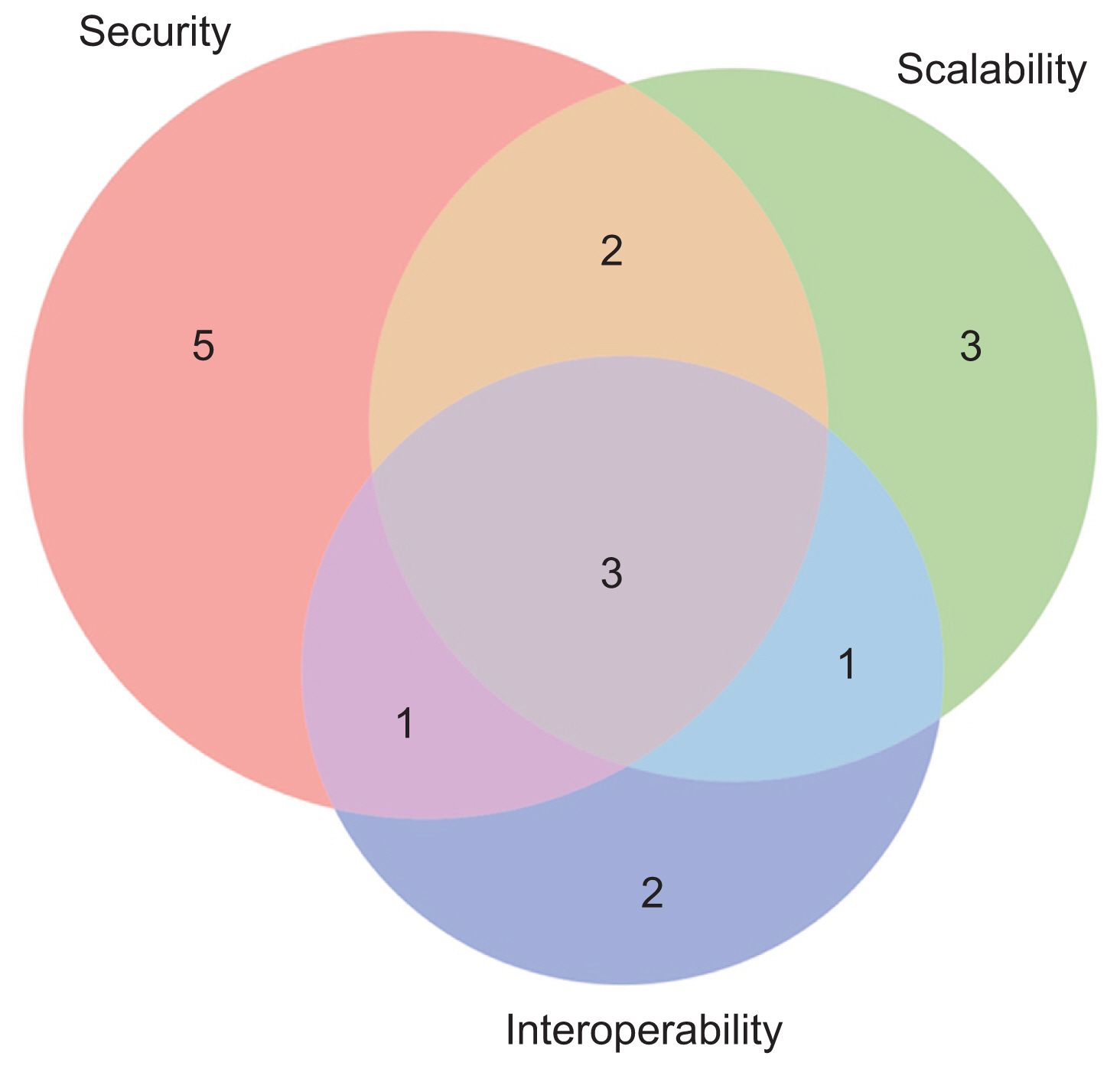
The review identified a notable trend towards the integration of emerging technologies into telemedicine architectures. Key areas of focus include interoperability, security, and scalability. Innovations such as cognitive radio technology, behavior-based control architectures, Health Level Seven International (HL7) Fast Healthcare Interoperability Resources (FHIR) standards, cloud computing, decentralized systems, and blockchain technology are addressing challenges in remote healthcare delivery and continuous monitoring.
Conclusions
This review highlights major advancements in telemedicine architectures, emphasizing the integration of advanced technologies to improve interoperability, security, and scalability. The findings underscore the successful application of cognitive radio technology, behavior-based control, HL7 FHIR standards, cloud computing, decentralized systems, and blockchain in advancing remote healthcare delivery.
Figure
Reference
-
References
1. Al-Sarayreh KT, Meridji K, Abran A. Software engineering principles: a systematic mapping study and a quantitative literature review. Eng Sci Technol Int J. 2021; 24(3):768–81. https://doi.org/10.1016/j.jestch.2020.11.005.
Article2. Fairley RE. Principles of software engineering. Hoboken (NJ): John Wiley & Sons;2011.3. Schieferdecker I, Ritter T. Advanced software engineering. Neugebauer R, editor. Digitalisierung. Heidelberg, Germany: Springer;2018. https://doi.org/10.1007/978-3-662-55890-4_21.
Article4. Yau SS. Position statement: advances and challenges of software engineering. In : Proceedings of 2008 32nd Annual IEEE International Computer Software and Applications Conference; 2008 Jul 28–Aug 1; Turku, Finland. https://doi.org/10.1109/COMPSAC.2008.240.
Article5. de Morais Barroca Filho I, Aquino GS Junior, Vasconcelos TB. Extending and instantiating a software reference architecture for IoT-based healthcare applications. Misra S, Gervasi O, Murgante B, Stankova E, Korkhov V, Torre C, editors. Computational science and its applications– ICCSA 2019. Cham, Switzerland: Springer;2019. p. 203–18. https://doi.org/10.1007/978-3-030-24308-1_17.
Article6. Barroca Filho ID, de Aquino GS Junior. A software reference architecture for IoT-based healthcare applications. Gervasi O, Murgante B, Misra S, Stankova E, Torre CM, Roca AM, editors. Computational science and its applications–ICCSA 2018. Cham, Switzerland: Springer;2018. p. 173–88. https://doi.org/10.1007/978-3-319-95171-3_15.
Article7. Krey M. Key challenges to enabling IT in healthcare. In : Proceedings of 2016 IEEE International Conference on Healthcare Informatics (ICHI); 2016 Oct 4–7; Chicago, IL, USA. p. 328–33. https://doi.org/10.1109/ICHI.2016.60.8. Quy VK, Hau NV, Anh DV, Ngoc LA. Smart healthcare IoT applications based on fog computing: architecture, applications and challenges. Complex Intell Systems. 2022; 8(5):3805–15. https://doi.org/10.1007/s40747-021-00582-9.
Article9. Kuziemsky CE, Knight J. 5th International workshop on software engineering in health care (SEHC 2013). In : Proceedings of 2013 35th International Conference on Software Engineering (ICSE); 2013 May 18–26; San Francisco, CA, USA. p. 1549–50. https://doi.org/10.1109/ICSE.2013.6606781.
Article10. Ayanlade OS, Oyebisi TO, Kolawole BA. Health Information Technology Acceptance Framework for diabetes management. Heliyon. 2019; 5(5):e01735. https://doi.org/10.1016/j.heliyon.2019.e01735.
Article11. Shenvi AA. Medical software: a regulatory process framework. In : Proceedings of the 3rd India Software Engineering Conference; 2010 Feb 25–27; Mysore, India. p. 119–24. https://doi.org/10.1145/1730874.1730897.
Article12. Miller RA, Gardner RM. Recommendations for responsible monitoring and regulation of clinical software systems. J Am Med Inf Assoc. 1997; 4(6):442–57. https://doi.org/10.1136/jamia.1997.0040442.
Article13. Troshani I, Goldberg S, Wickramasinghe N. Designing enabling regulatory frameworks to facilitate the diffusion of wireless technology solutions in healthcare. Wickramasinghe N, Al-Hakim L, Gonzalez C, Tan J, editors. Lean thinking for Healthcare. New York (NY): Springer;2014. p. 331–44. https://doi.org/10.1007/978-1-4614-8036-5_19.
Article14. Richardson I, Reid L, O’Leary P. Healthcare systems quality: development and use. In : Proceedings of the International Workshop on Software Engineering in Healthcare Systems; 2016 May 14–22; Austin, TX, USA. p. 50–3. https://doi.org/10.1145/2897683.2897686.
Article15. Schulz S, Stegwee R, Chronaki C. Standards in healthcare data. Kubben P, Dumontier M, Dekker A, editors. Fundamentals of clinical data science. Cham, Switzerland: Springer;2019. p. 19–36. https://doi.org/10.1007/978-3-319-99713-1_3.
Article16. Robinson PN, Graessner H. Rare-disease data standards. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2022; 65(11):1126–32. https://doi.org/10.1007/s00103-022-03591-2.
Article17. Imler TD, Vreeman DJ, Kannry J. Healthcare data standards and exchange. Finnell J, Dixon B, editors. Clinical informatics study guide: text and review. Cham, Switzerland: Springer;2016. p. 233–53. https://doi.org/10.1007/978-3-319-22753-5_11.
Article18. Alkraiji AI, Jackson T, Murray I. Factors impacting the adoption decision of health data standards in tertiary healthcare organisations in Saudi Arabia. J Enterp Inf Manag. 2016; 29(5):650–76. https://doi.org/10.1108/JEIM-11-2014-0111.
Article19. Hovenga E, Grain H. Health data standards’ limitations. Roadmap to successful digital health ecosystems. New York (NY): Academic Press;2022. p. 169–207. https://doi.org/10.1016/B978-0-12-823413-6.00015-X.
Article20. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Article21. Shaikh A, Al Reshan MS, Sulaiman A, Alshahrani H, Asiri Y. Secure telemedicine system design for COVID-19 patients treatment using service oriented architecture. Sensors (Basel). 2022; 22(3):952. https://doi.org/10.3390/s22030952.
Article22. Adarsh A, Pathak S, Kumar B. Design and analysis of a reliable, prioritized and cognitive radio-controlled telemedicine network architecture for internet of healthcare things. Int J Comput Netw Appl. 2021; 8(1):54–66. https://doi.org/10.22247/ijcna/2021/207982.
Article23. Ferdana N, Adriansyah A, Budiyanto S, Andika J. Design of a telemedicine robot using behavior-based control architecture. AIP Conference Proceedings. 2020; 2217(1):030092. https://doi.org/10.1063/5.0000595.
Article24. Albahri OS, Zaidan AA, Zaidan BB, Albahri AS, Mohsin AH, Mohammed KI, et al. New mHealth hospital selection framework supporting decentralised telemedicine architecture for outpatient cardiovascular disease-based integrated techniques: Haversine-GPS and AHP-VIKOR. J Ambient Intell Humaniz Comput. 2022; 13:219–39. https://doi.org/10.1007/s12652-021-02897-4.
Article25. Liu L, Wang L, Huang Q, Zhou L, Fu X, Liu L. An efficient architecture for medical high-resolution images transmission in mobile telemedicine systems. Comput Methods Programs Biomed. 2020; 187:105088. https://doi.org/10.1016/j.cmpb.2019.105088.
Article26. Mishra S, Bhutia SD, Akhtar N, Dhar S. Cloud-based multilayer telemedicine architecture: a case study. Bera R, Sarkar S, Singh O, Saikia H, editors. Advances in communication, devices and networking. Singapore: Springer;2019. p. 553–61. https://doi.org/10.1007/978-981-13-3450-4_60.
Article27. Ferreira FA, Cadotte BF, Mohamed RN, Rodrigues ST, Gruby T, Davidson A, et al. Hybrid videoconferencing architecture for telemedicine. United State patent. 11, 038,933. 2021. Jun. 15.28. Goeg KR, Rasmussen RK, Jensen L, Wollesen CM, Larsen S, Pape-Haugaard LB. A future-proof architecture for telemedicine using loose-coupled modules and HL7 FHIR. Comput Methods Programs Biomed. 2018; 160:95–101. https://doi.org/10.1016/j.cmpb.2018.03.010.
Article29. Tiwari V, Bansod PP, Kumar A. Compressed medical image transmission in telemedicine architecture. Tiwari B, Tiwari V, Das K, Mishra D, Bansal J, editors. Proceedings of International Conference on Recent Advancement on Computer and Communication. Singapore: Springer;2018. p. 205–12. https://doi.org/10.1007/978-981-10-8198-9_21.
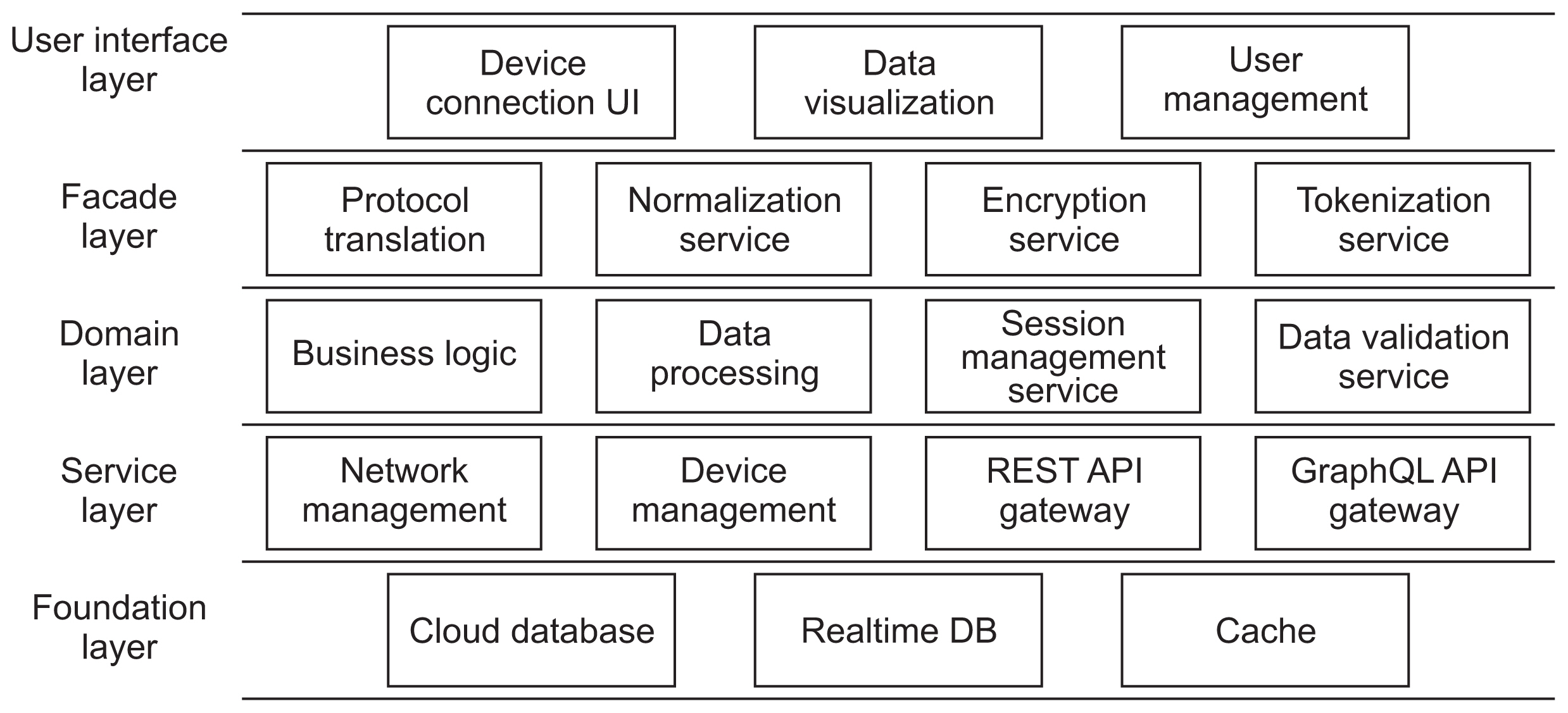
Article30. Dubgorn A, Kalinina O, Lyovina A, Rotar O. Foundation architecture of telemedicine system services based on Health 4.0 concept. SHS Web of Conferences. 2018; 44:00032. https://doi.org/10.1051/shsconf/20184400032.
Article31. Shaikh AZ, Tamil L. Cognitive radio enabled telemedicine system. Wirel Pers Commun. 2015; 83:765–78. https://doi.org/10.1007/s11277-015-2423-1.
Article32. Poenaru E, Poenaru C. Networking architectures for healthcare wireless sensor networks comparison of architectures used for remote patient monitoring. In : Proceedings of 2013 11th RoEduNet International Conference; 2013 Jan 17–19; Sinaia, Romania. p. 1–6. https://doi.org/10.1109/RoEduNet.2013.6511728.33. Pramanik PK, Nayyar A, Pareek G. WBAN: driving e-healthcare beyond telemedicine to remote health monitoring: architecture and protocols. Jude HD, Balas VE, editors. Telemedicine technologies. New York (NY): Academic Medicine;2019. p. 89–119. https://doi.org/10.1016/B978-0-12-816948-3.00007-6.
Article34. Luan Y, Ren G. The E-health network design. In : Proceedings of 2015 International Conference on Network and Information Systems for Computers; 2015 Jan 23–25; Wuhan, China. p. 557–9. https://doi.org/10.1109/ICNISC.2015.100.
Article35. Salman OH, Rasid MF, Saripan MI, Subramaniam SK. Multi-sources data fusion framework for remote triage prioritization in telehealth. J Med Syst. 2014; 38(9):103. https://doi.org/10.1007/s10916-014-0103-4.
Article36. Mironov R, Kountchev R. Architecture for medical image processing. Kountchev R, Iantovics B, editors. Advances in intelligent analysis of medical data and decision support systems. Heidelberg, Germany: Springer;2013. p. 225–34. https://doi.org/10.1007/978-3-319-00029-9_20.
Article37. Pandya B, Chuang FK, Tseng CH, Chiueh TD. An energy-efficient communication system using joint beamforming in multi-hop health monitoring sensor networks. J Wirel Commun Netw. 2017; 2017:172. https://doi.org/10.1186/s13638-017-0957-5.
Article38. Kim DW, Choi JY, Han KH. Risk management-based security evaluation model for telemedicine systems. BMC Med Inform Decis Mak. 2020; 20(1):106. https://doi.org/10.1186/s12911-020-01145-7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Real-time Emergency Telemedicine System: Prototype Design and Functional Evaluation
- Telemedicine in the U.S.A. with Focus on Clinical Applications and Issues
- A Design of A Mobile Remote Monitoring PDA Prototype Base on Embedded Linux with Wireless LAN Environment
- Design and Construction of a NLP Based Knowledge Extraction Methodology in the Medical Domain Applied to Clinical Information
- Quality Reporting of Systematic Review and Meta-Analysis According to PRISMA 2020 Guidelines: Results from Recently Published Papers in the Korean Journal of Radiology