Korean J Orthod.
2024 Jul;54(4):247-256. 10.4041/kjod23.188.
Evaluation of mandibular condyle position in Class III patients after bimaxillary orthognathic surgery: A cone-beam computed tomography study
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Istanbul University, İstanbul, Turkiye
- 2Department of Dentomaxillofacial Radiology, Yeditepe University, İstanbul, Turkiye
- 3Department of Robots and Smart Systems, Institute of Science, TurkishGerman University, İstanbul, Turkiye
- KMID: 2558294
- DOI: http://doi.org/10.4041/kjod23.188
Abstract
Objective
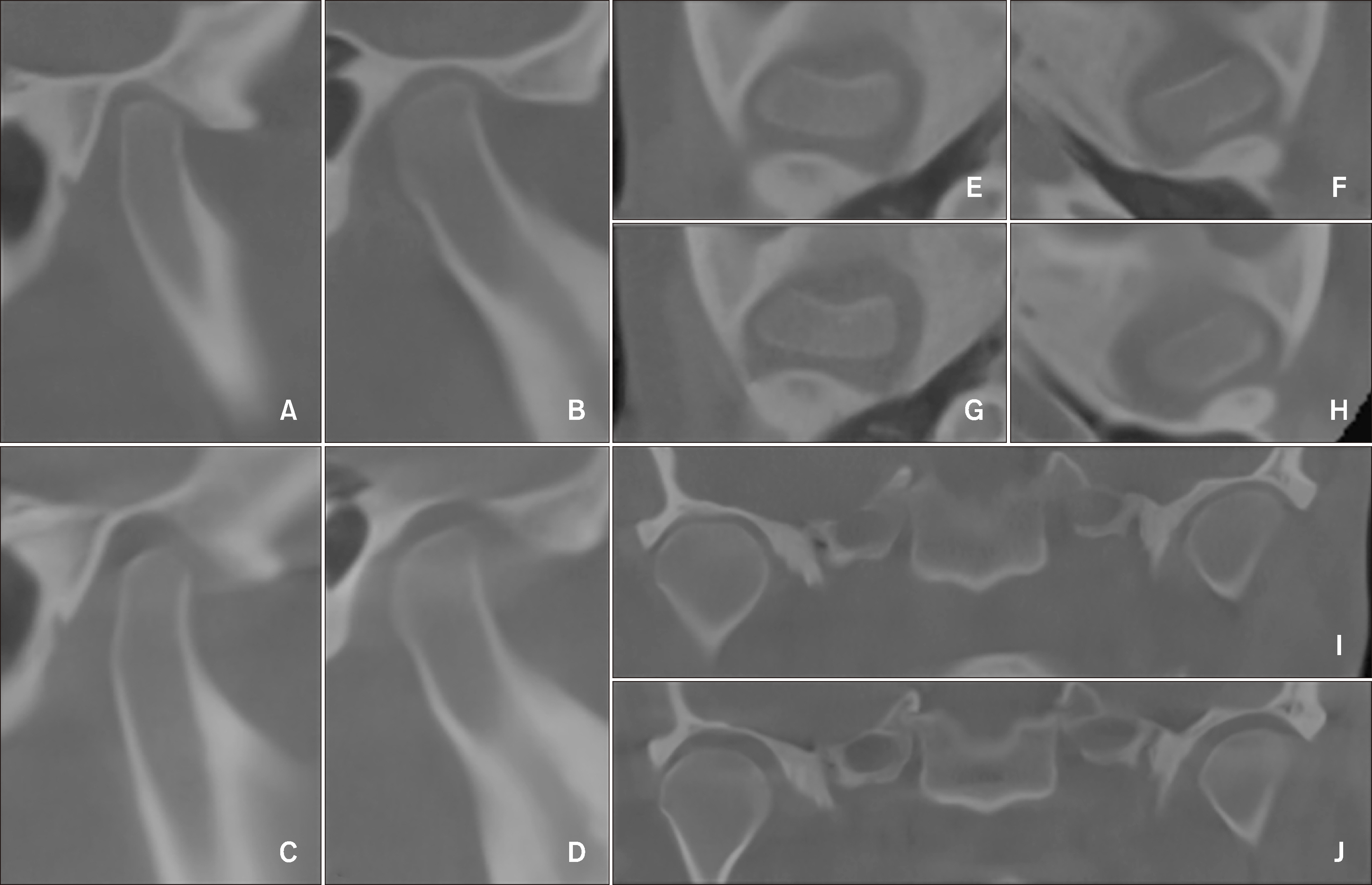
This retrospective study evaluated the mandibular condyle position before and after bimaxillary orthognathic surgery performed with the mandibular condyle positioned manually in patients with mandibular prognathism using cone-beam computed tomography.
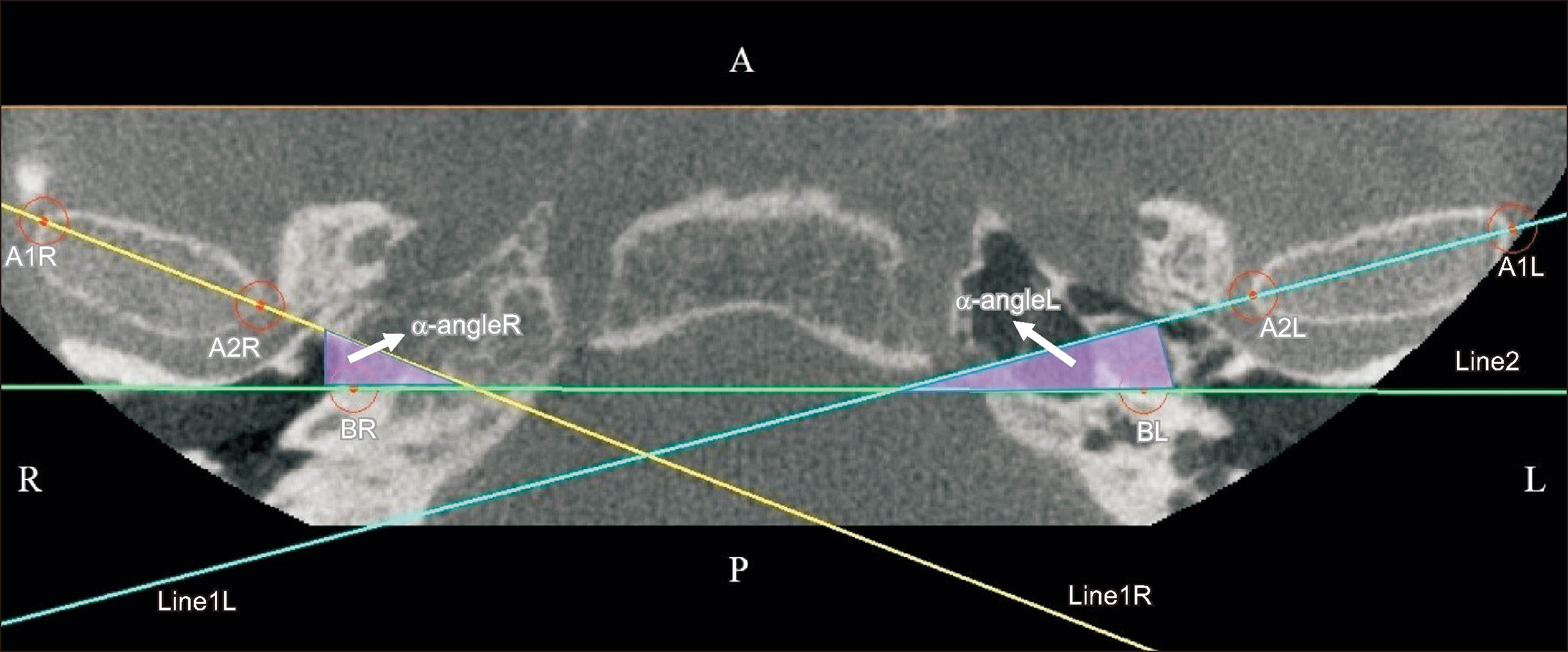
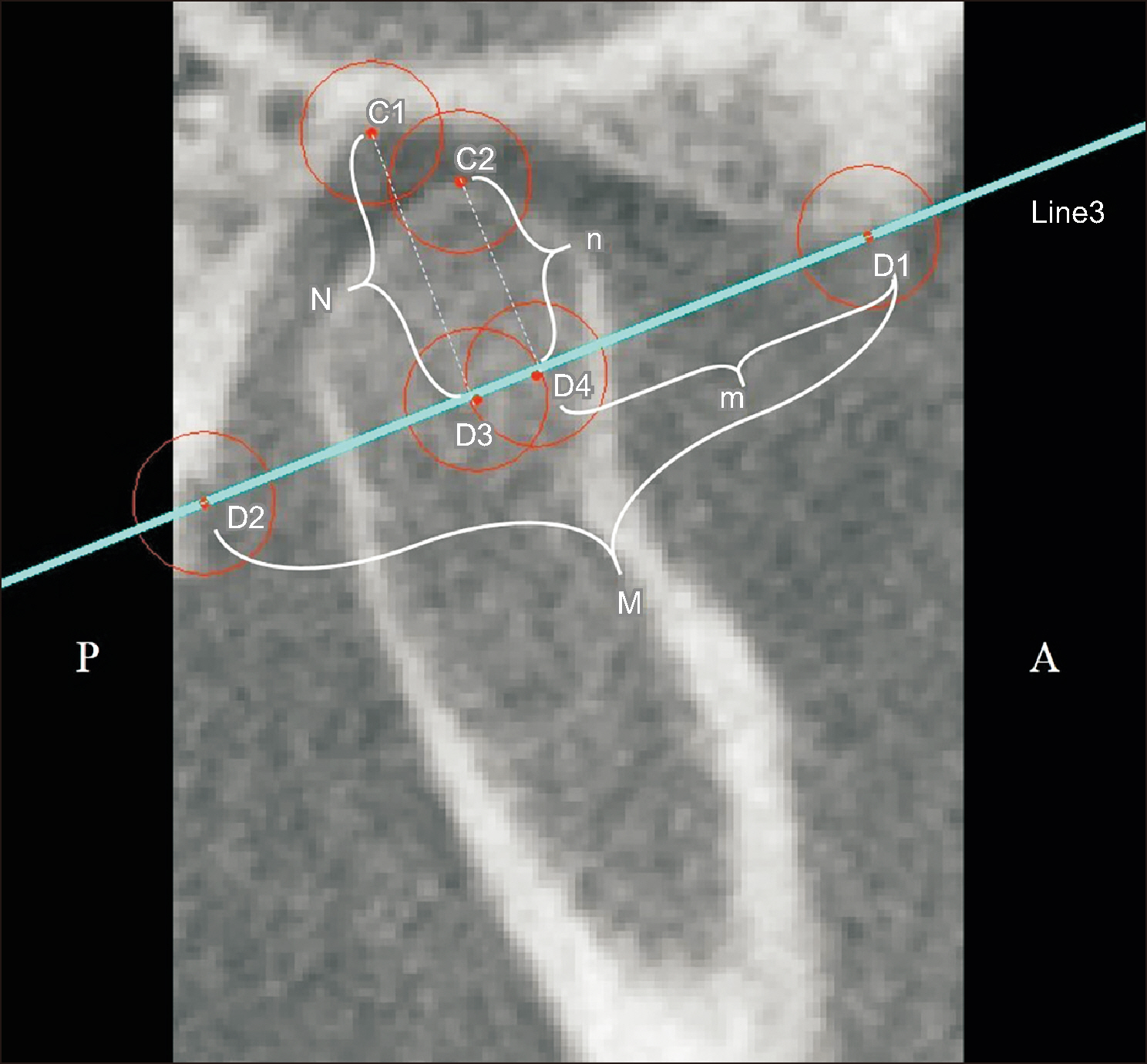
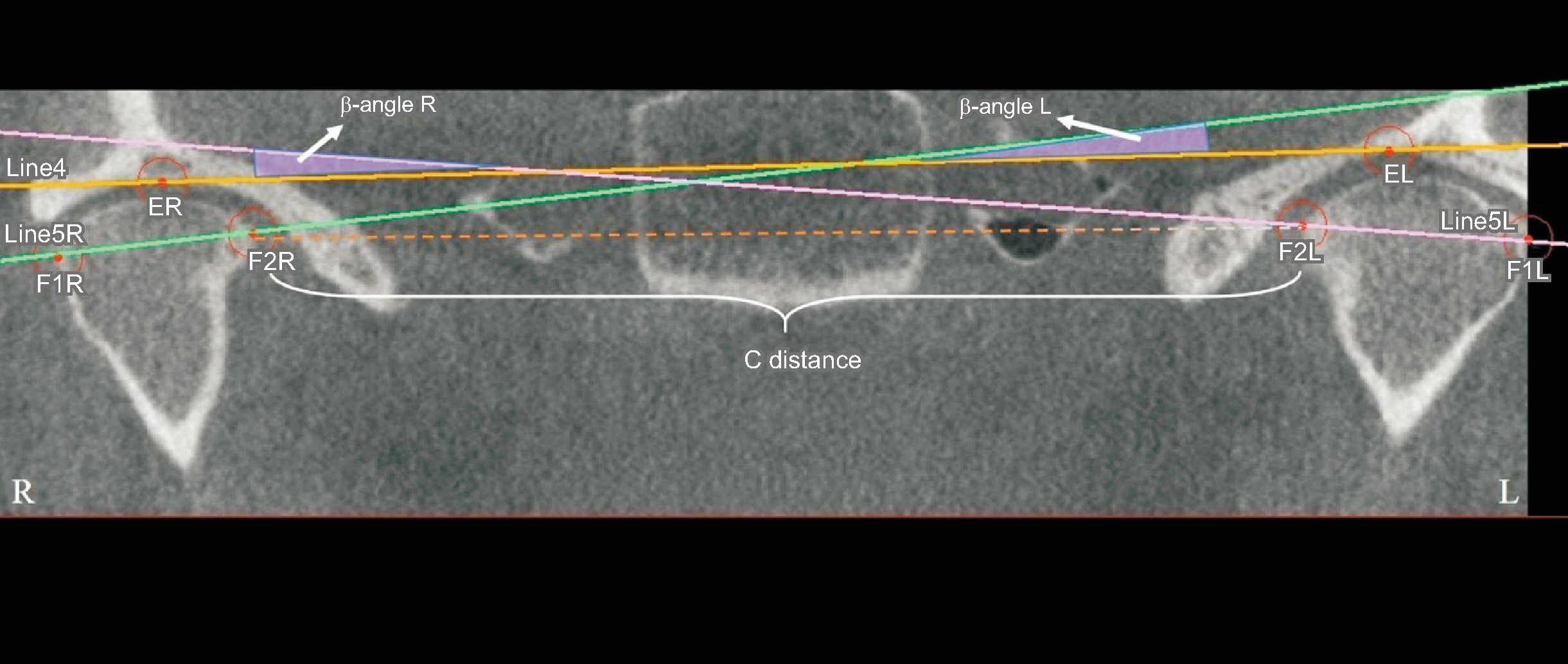
Methods
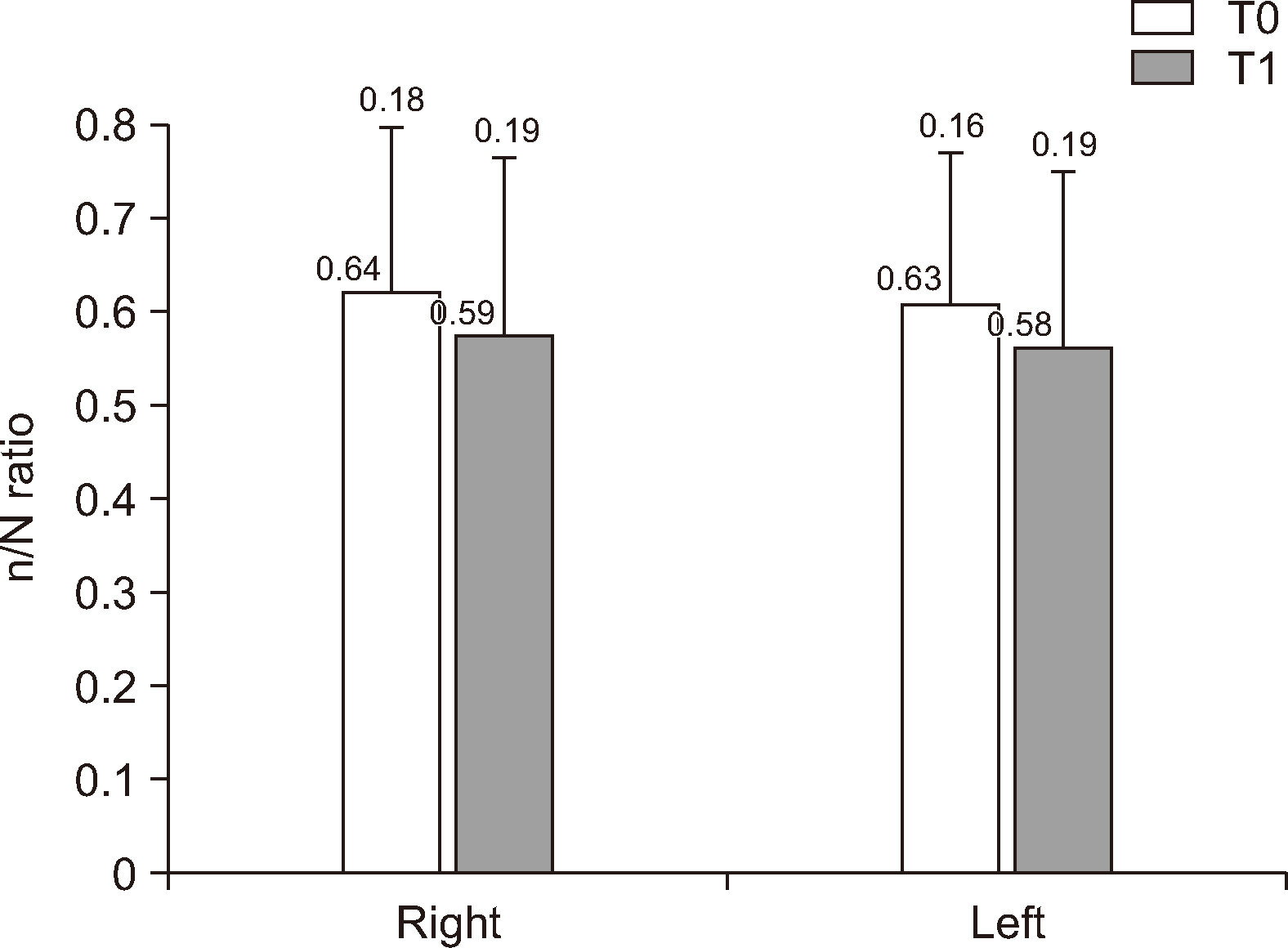
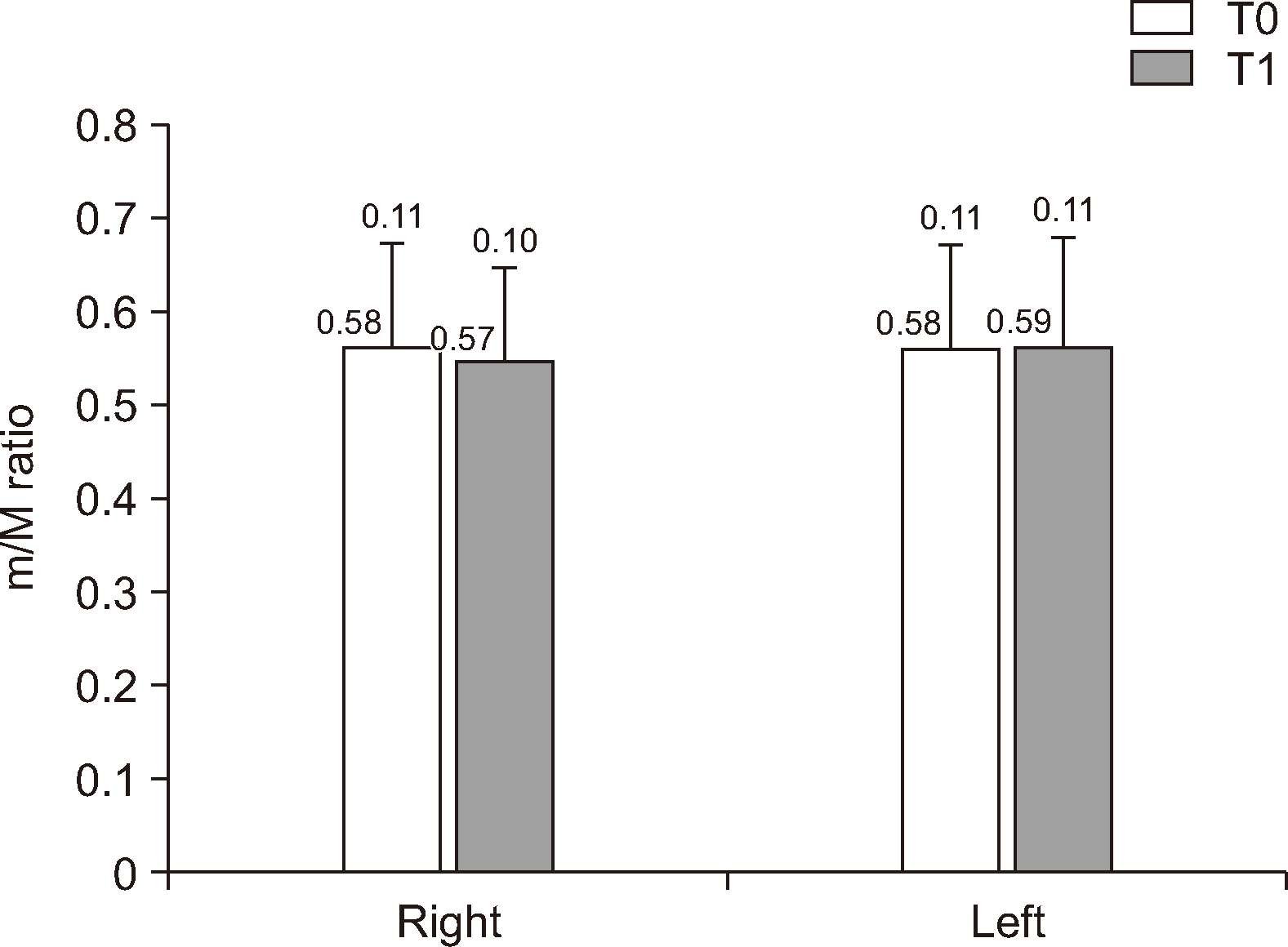
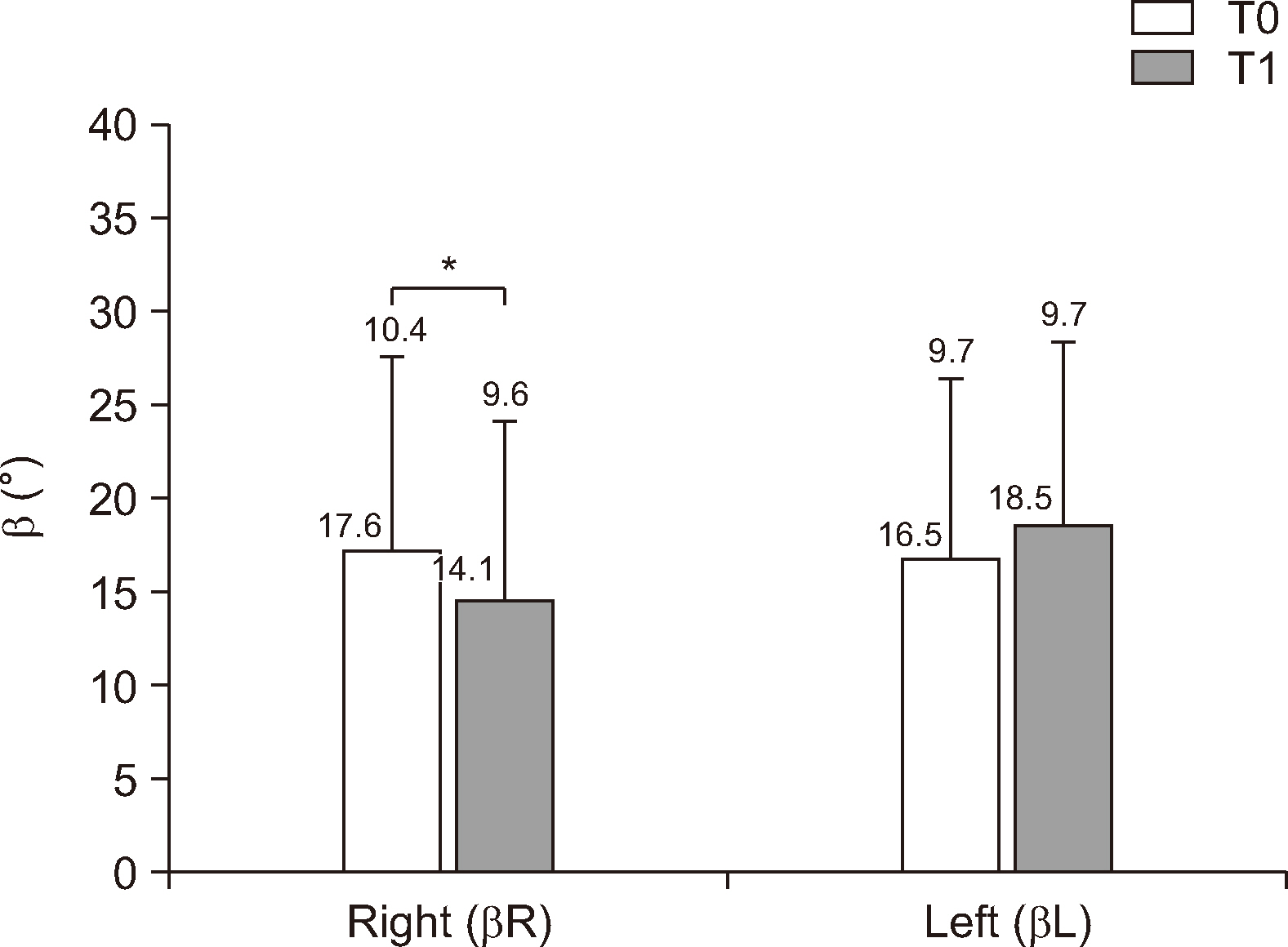
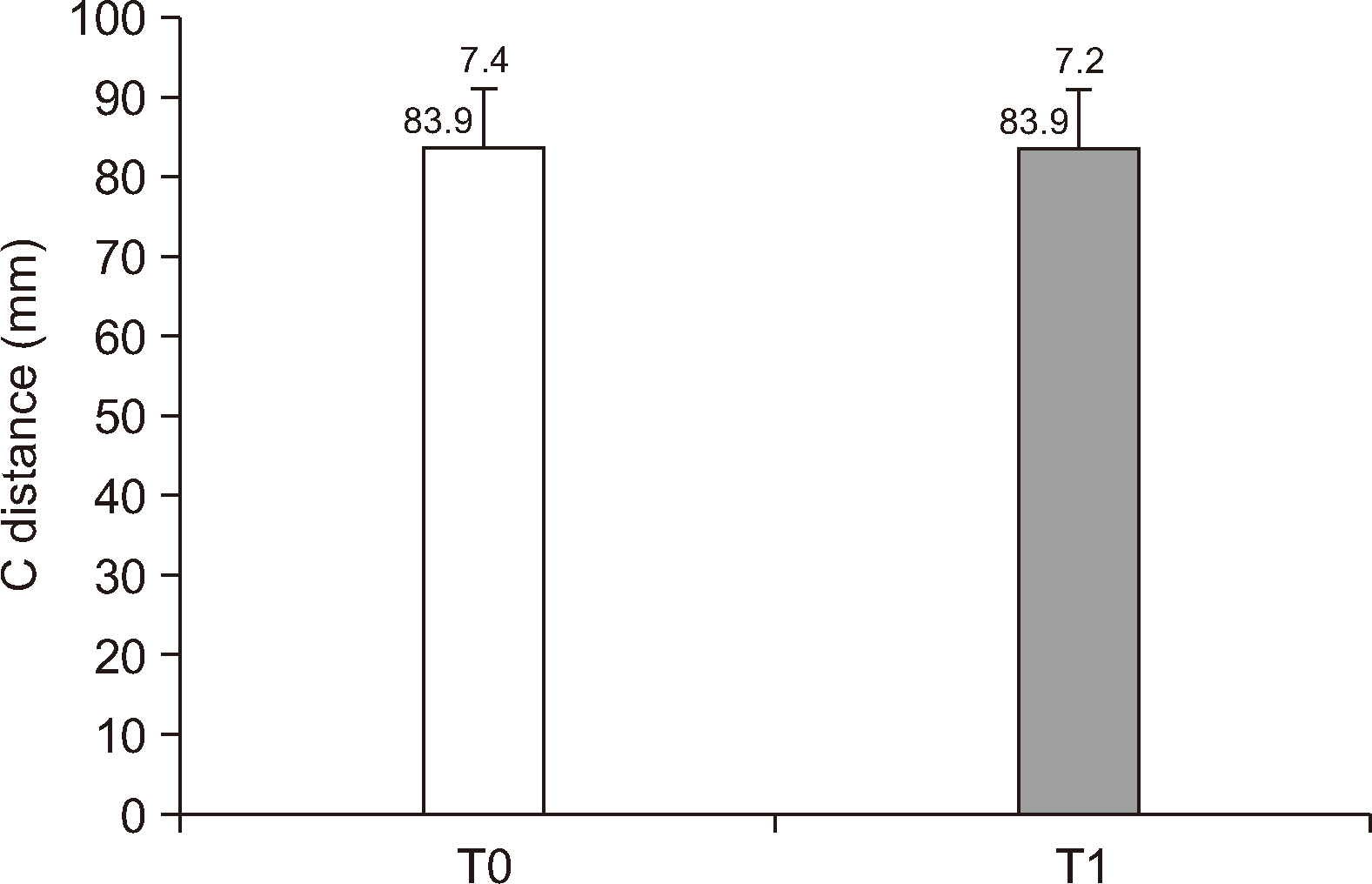
Overall, 88 mandibular condyles from 44 adult patients (20 female and 24 male) diagnosed with mandibular prognathism due to skeletal Class III malocclusion who underwent bilateral sagittal split ramus osteotomy (BSSRO) and Le Fort I performed using the manual condyle positioning method were included. Conebeam computed tomography images obtained 1–2 weeks before (T0) and approximately 6 months after (T1) surgery were analyzed in three planes using 3D Slicer software. Statistical significance was set at P < 0.05 level.
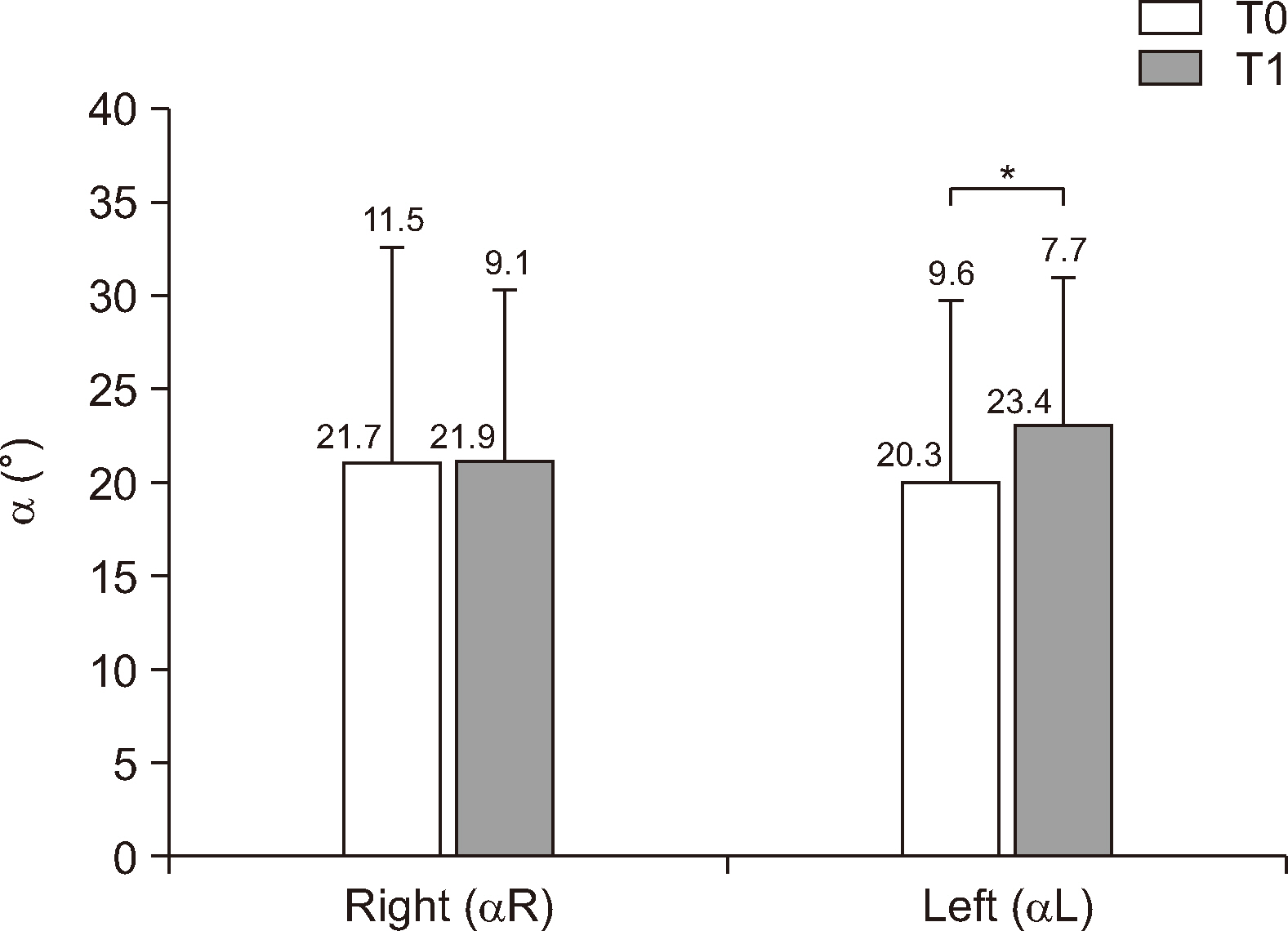
Results
Significant inward rotation of the left mandibular condyle and significant outward rotation of the right mandibular condyle were observed in the axial and coronal planes (P < 0.05). The positions of the right and left condyles in the sagittal plane and the distance between the most medial points of the condyles in the coronal plane did not differ significantly (P > 0.05).
Conclusions
While the change in the sagittal plane can be maintained as before surgery with manual positioning during the BSSRO procedure, significant inward and outward rotation was observed in the axial and coronal planes, respectively, even in the absence of concomitant temporomandibular joint disorder before or after the operation. Further long-term studies are needed to correlate these findings with possible clinical consequences.
Figure
Reference
-
References
1. Kim YI, Cho BH, Jung YH, Son WS, Park SB. 2011; Cone-beam computerized tomography evaluation of condylar changes and stability following two-jaw surgery: le fort I osteotomy and mandibular setback surgery with rigid fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 111:681–7. http://doi.org/10.1016/j.tripleo.2010.08.001. DOI: 10.1016/j.tripleo.2010.08.001. PMID: 21055977.
Article2. Hong M, Kim MJ, Shin HJ, Cho HJ, Baek SH. 2020; Three-dimensional surgical accuracy between virtually planned and actual surgical movements of the maxilla in two-jaw orthognathic surgery. Korean J Orthod. 50:293–303. https://doi.org/10.4041/kjod.2020.50.5.293. DOI: 10.4041/kjod.2020.50.5.293. PMID: 32938822. PMCID: PMC7500567.
Article3. Mda B, F ME, McZ D. 2022; Methods of mandibular condyle position and rotation center used for orthognathic surgery planning: a systematic review. J Stomatol Oral Maxillofac Surg. 123:345–52. https://doi.org/10.1016/j.jormas.2021.06.004. DOI: 10.1016/j.jormas.2021.06.004. PMID: 34237437.
Article4. Meriç G. 2010; A literature review of the sentric relation and registration methods up to date. J Dent Fac Atatürk Uni. 2010:54–9. https://dergipark.org.tr/en/pub/ataunidfd/issue/2481/31754.5. Bettega G, Cinquin P, Lebeau J, Raphaël B. 2002; Computer-assisted orthognathic surgery: clinical evaluation of a mandibular condyle repositioning system. J Oral Maxillofac Surg. 60:27–34. discussion 34–5. https://doi.org/10.1053/joms.2002.29069. DOI: 10.1053/joms.2002.29069. PMID: 11757002.
Article6. Ueki K, Moroi A, Sotobori M, Ishihara Y, Marukawa K, Takatsuka S, et al. 2012; A hypothesis on the desired postoperative position of the condyle in orthognathic surgery: a review. Oral Surg Oral Med Oral Pathol Oral Radiol. 114:567–76. https://doi.org/10.1016/j.oooo.2011.12.026. DOI: 10.1016/j.oooo.2011.12.026. PMID: 22819333.
Article7. Savoldelli C, Chamorey E, Bettega G. 2018; Computer-assisted teaching of bilateral sagittal split osteotomy: learning curve for condylar positioning. PLoS One. 13:e0196136. https://doi.org/10.1371/journal.pone.0196136. DOI: 10.1371/journal.pone.0196136. PMID: 29694423. PMCID: PMC5918964. PMID: af8cc01d35b640559d4f5731ce013f9d.
Article8. Podčernina J, Urtāne I, Pirttiniemi P, Šalms Ģ, Radziņš O, Aleksejūnienė J. 2020; Evaluation of condylar positional, structural, and volumetric status in class III orthognathic surgery patients. Medicina (Kaunas). 56:672. https://doi.org/10.3390/medicina56120672. DOI: 10.3390/medicina56120672. PMID: 33291272. PMCID: PMC7762172. PMID: 5b5c5b09ed6d43728867478b33423c78.
Article9. Costa F, Robiony M, Toro C, Sembronio S, Polini F, Politi M. 2008; Condylar positioning devices for orthognathic surgery: a literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 106:179–90. https://doi.org/10.1016/j.tripleo.2007.11.027. DOI: 10.1016/j.tripleo.2007.11.027. PMID: 18417381.
Article10. Choi BJ, Kim BS, Lim JM, Jung J, Lee JW, Ohe JY. 2018; Positional change in mandibular condyle in facial asymmetric patients after orthognathic surgery: cone-beam computed tomography study. Maxillofac Plast Reconstr Surg. 40:13. https://doi.org/10.1186/s40902-018-0152-6. DOI: 10.1186/s40902-018-0152-6. PMID: 29984220. PMCID: PMC6015790. PMID: 89bb133f32784a8f9487abb77af450ea.
Article11. Koo TK, Li MY. 2016; A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 15:155–63. https://doi.org/10.1016/j.jcm.2016.02.012. DOI: 10.1016/j.jcm.2016.02.012. PMID: 27330520. PMCID: PMC4913118.
Article12. Bethge LS, Ballon A, Mack M, Landes C. 2015; Intraoperative condyle positioning by sonographic monitoring in orthognathic surgery verified by MRI. J Craniomaxillofac Surg. 43:71–80. https://doi.org/10.1016/j.jcms.2014.10.012. DOI: 10.1016/j.jcms.2014.10.012. PMID: 25457463.
Article13. Gerressen M, Stockbrink G, Smeets R, Riediger D, Ghassemi A. 2007; Skeletal stability following bilateral sagittal split osteotomy (BSSO) with and without condylar positioning device. J Oral Maxillofac Surg. 65:1297–302. https://doi.org/10.1016/j.joms.2006.10.026. DOI: 10.1016/j.joms.2006.10.026. PMID: 17577492.14. Sander AK, Martini M, Konermann AC, Meyer U, Wenghoefer M. 2015; Freehand condyle-positioning during orthognathic surgery: postoperative cone-beam computed tomography shows only minor morphometric alterations of the temporomandibular joint position. J Craniofac Surg. 26:1471–6. https://doi.org/10.1097/SCS.0000000000001781. DOI: 10.1097/SCS.0000000000001781. PMID: 26163838.15. Hollender L, Ridell A. 1974; Radiography of the temporomandibular joint after oblique sliding osteotomy of the mandibular rami. Scand J Dent Res. 82:466–9. https://doi.org/10.1111/j.1600-0722.1974.tb00403.x. DOI: 10.1111/j.1600-0722.1974.tb00403.x. PMID: 4529372.
Article16. Hu J, Wang D, Zou S. 2000; Effects of mandibular setback on the temporomandibular joint: a comparison of oblique and sagittal split ramus osteotomy. J Oral Maxillofac Surg. 58:375–80. discussion 380–1. https://doi.org/10.1016/s0278-2391(00)90915-7. DOI: 10.1016/S0278-2391(00)90915-7. PMID: 10759116.
Article17. Kawamata A, Fujishita M, Nagahara K, Kanematu N, Niwa K, Langlais RP. 1998; Three-dimensional computed tomography evaluation of postsurgical condylar displacement after mandibular osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 85:371–6. https://doi.org/10.1016/s1079-2104(98)90059-2. DOI: 10.1016/S1079-2104(98)90059-2. PMID: 9574943.
Article18. Kim MI, Kim JH, Jung S, Park HJ, Oh HK, Ryu SY, et al. 2015; Condylar positioning changes following unilateral sagittal split ramus osteotomy in patients with mandibular prognathism. Maxillofac Plast Reconstr Surg. 37:36. https://doi.org/10.1186/s40902-015-0036-y. DOI: 10.1186/s40902-015-0036-y. PMID: 26501042. PMCID: PMC4608983.
Article19. Lee JS, Xi T, Kwon TG. 2017; Three-dimensional analysis of mandibular condyle position in patients with deviated mandibular prognathism. Int J Oral Maxillofac Surg. 46:1052–8. https://doi.org/10.1016/j.ijom.2017.02.1272. DOI: 10.1016/j.ijom.2017.02.1272. PMID: 28302336.
Article20. Lee W, Park JU. 2002; Three-dimensional evaluation of positional change of the condyle after mandibular setback by means of bilateral sagittal split ramus osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 94:305–9. https://doi.org/10.1067/moe.2002.126452. DOI: 10.1067/moe.2002.126452. PMID: 12324783.
Article21. Ma RH, Li G, Yin S, Sun Y, Li ZL, Ma XC. 2020; Quantitative assessment of condyle positional changes before and after orthognathic surgery based on fused 3D images from cone beam computed tomography. Clin Oral Investig. 24:2663–72. https://doi.org/10.1007/s00784-019-03128-z. DOI: 10.1007/s00784-019-03128-z. PMID: 31728734.
Article22. Sobouti F, Hadian H, Pakravan AH, Rahimi Z, Rakhshan V, Dadgar S. 2022; Short-term and long-term alterations of condylar position after bilateral sagittal split ramus osteotomy for mandibular setback: a preliminary before-after clinical trial. Dent Res J (Isfahan). 19:19. https://doi.org/10.4103/1735-3327.338782. DOI: 10.4103/1735-3327.338782. PMID: 35308442. PMCID: PMC8927962. PMID: 7235f4da86984ad086d74c1d59dcda92.
Article23. Ueki K, Nakagawa K, Takatsuka S, Shimada M, Marukawa K, Takazakura D, et al. 2000; Temporomandibular joint morphology and disc position in skeletal class III patients. J Craniomaxillofac Surg. 28:362–8. https://doi.org/10.1054/jcms.2000.0181. DOI: 10.1054/jcms.2000.0181. PMID: 11465144.
Article24. Kim YI, Jung YH, Cho BH, Kim JR, Kim SS, Son WS, et al. 2010; The assessment of the short- and long-term changes in the condylar position following sagittal split ramus osteotomy (SSRO) with rigid fixation. J Oral Rehabil. 37:262–70. https://doi.org/10.1111/j.1365-2842.2009.02056.x. DOI: 10.1111/j.1365-2842.2009.02056.x. PMID: 20113391.
Article25. Nishimura A, Sakurada S, Iwase M, Nagumo M. 1997; Positional changes in the mandibular condyle and amount of mouth opening after sagittal split ramus osteotomy with rigid or nonrigid osteosynthesis. J Oral Maxillofac Surg. 55:672–6. discussion 677–8. https://doi.org/10.1016/s0278-2391(97)90572-3. DOI: 10.1016/S0278-2391(97)90572-3. PMID: 9216497.26. Kim JW, Lee DH, Lee SY, Kim JH, Lee SH. 2009; 3-D CT evaluation of condyle head position, mandibular width, and mandibular angle after mandibular setback surgery. J Korean Assoc Oral Maxillofac Surg. 35:229–39. https://www.jkaoms.org/journal/view.html?uid=374&vmd=Full.27. Jung GS, Kim TK, Lee JW, Yang JD, Chung HY, Cho BC, et al. 2017; The effect of a condylar repositioning plate on condylar position and relapse in two-jaw surgery. Arch Plast Surg. 44:19–25. https://doi.org/10.5999/aps.2017.44.1.19. DOI: 10.5999/aps.2017.44.1.19. PMID: 28194343. PMCID: PMC5300918. PMID: 580d9d457aae41e59b8f4de365a4a3e8.
Article28. Omar EAZ, Bamber MA. 2010; Orthognathic model surgery by using of a passive robot arm. Saudi Dent J. 22:47–55. https://doi.org/10.1016/j.sdentj.2010.02.006. DOI: 10.1016/j.sdentj.2010.02.006. PMID: 24227912. PMCID: PMC3824638.
Article29. Ueki K, Hashiba Y, Marukawa K, Alam S, Nakagawa K, Yamamoto E. 2008; Skeletal stability after mandibular setback surgery: bicortical fixation using a 2.0-mm locking plate system versus monocortical fixation using a nonlocking plate system. J Oral Maxillofac Surg. 66:900–4. https://doi.org/10.1016/j.joms.2007.08.033. DOI: 10.1016/j.joms.2007.08.033. PMID: 18423278.30. Choi KY, Lee SH. 1996; Evaluation of condylar position using computed tomograph following bilateral sagittal split ramus osteotomy. Maxillofac Plast Reconstr Surg. 18:570–93. https://kiss.kstudy.com/Detail/Ar?key=1956811.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mandibular condyle position in cone beam computed tomography
- Cone beam computed tomography findings of ectopic mandibular third molar in the mandibular condyle: report of a case
- Three-dimensional analysis of pharyngeal airway change of skeletal class III patients in cone beam computed tomography after bimaxillary surgery
- Positional change in mandibular condyle in facial asymmetric patients after orthognathic surgery: cone-beam computed tomography study
- Two-dimensional and volumetric airway changes after bimaxillary surgery for class III malocclusion