Korean J Orthod.
2024 Jul;54(4):229-238. 10.4041/kjod23.256.
Prevalence of malocclusions and parafunctional habits in pediatric patients with developmental dyslexia
- Affiliations
-
- 1Institute of Dental Clinic, Catholic University of Sacred Heart, IRCCS A. Gemelli University Polyclinic Foundation, Rome, Italy
- 2College of Dental Medicine, Midwestern University, Downers Grove, IL, USA
- KMID: 2558292
- DOI: http://doi.org/10.4041/kjod23.256
Abstract
Objective
The study aimed to assess the prevalence of dental malocclusion, orthodontic parameters, and parafunctional habits in children with developmental dyslexia (DD).
Methods
Forty pediatric patients (67.5% boys and 32.5% girls, mean age: 11.02 ± 2.53 years, range: 6–15 years) with DD were compared with 40 age- and sex-matched healthy participants for prevalence of dental malocclusion, orthodontic parameters, and parafunctional habits. Dental examinations were performed by an orthodontist.
Results
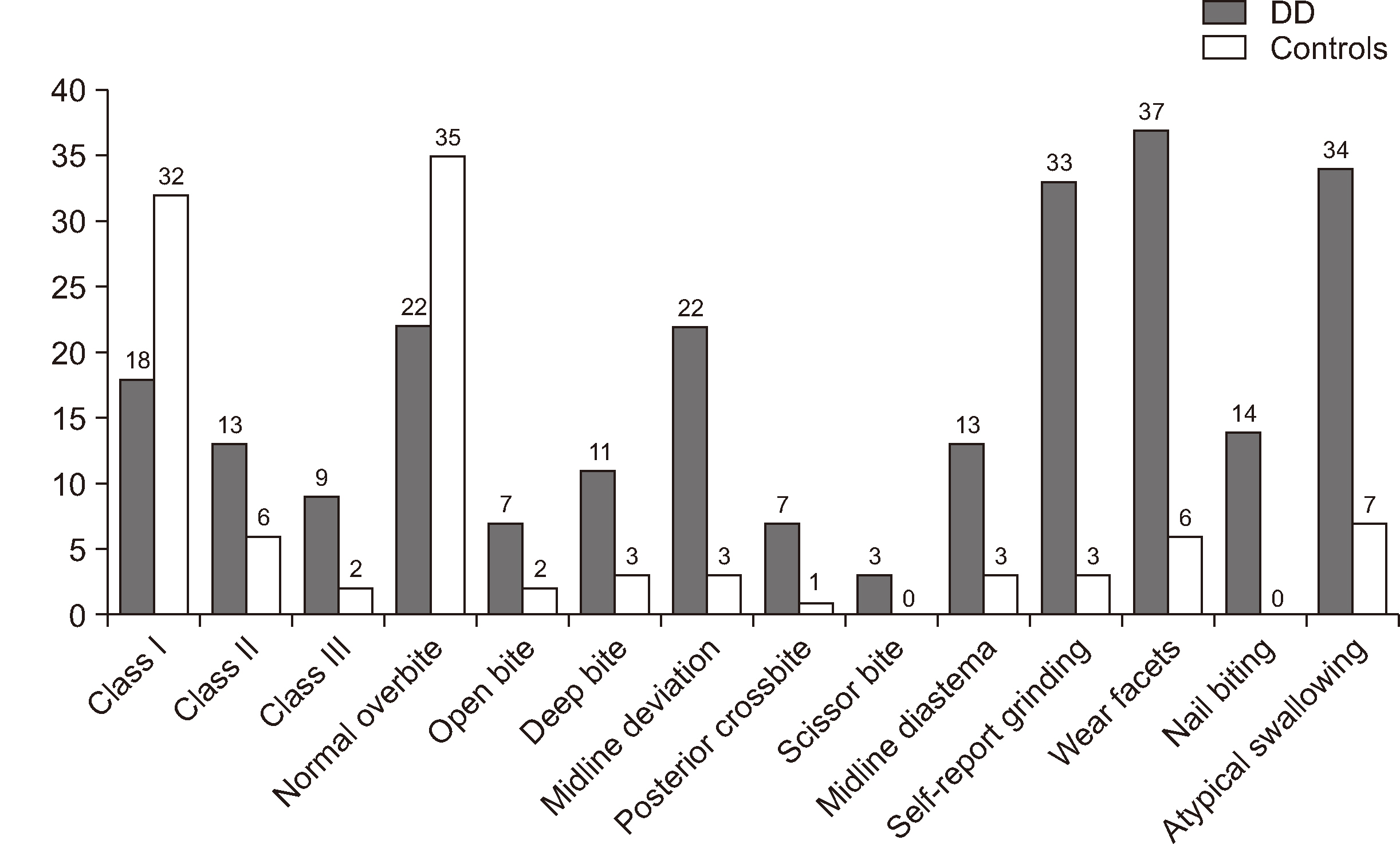
Pediatric patients with DD exhibited a significantly higher prevalence of Angle Class III malocclusion (22.5% vs. 5.0%, P = 0.024), deep bite (27.5% vs. 7.5%, P = 0.019), midline deviation (55.0% vs. 7.5%, P < 0.0001), midline diastemas (32.5% vs. 7.5%, P = 0.010), wear facets (92.5% vs. 15.0%, P < 0.0001), self-reported nocturnal teeth grinding (82.5% vs. 7.5%, P < 0.0001), nail biting (35.0% vs. 0.0%, P < 0.0001), and atypical swallowing (85.0% vs. 17.5%, P < 0.0001) compared to that in healthy controls.
Conclusions
Pediatric patients with DD showed a higher prevalence of Class III malocclusion, greater orthodontic vertical and transverse discrepancies, and incidence of parafunctional activities. Clinicians and dentists should be aware of the vulnerability of children with dyslexia for exhibiting malocclusion and encourage early assessment and multidisciplinary intervention.
Figure
Reference
-
References
1. Authenticated U.S. Government Information (GPO). 2018. First step act of 2018. Public law 115-391; 132 Stat. 5194. GPO;https://www.congress.gov/115/plaws/publ391/PLAW-115publ391.pdf.2. Stanley C, Petscher Y. 2017. Defining dyslexia . U.S. Department of Education, Office of Elementary and Secondary Education, Office of Special Education Programs, National Center on Improving Literacy;Washington, D.C.: https://improvingliteracy.org/brief/defining-dyslexia/index.html.3. Assaf DDC, Knorst JK, Busanello-Stella AR, Ferrazzo VA, Berwig LC, Ardenghi TM, et al. 2021; Association between malocclusion, tongue position and speech distortion in mixed-dentition schoolchildren: an epidemiological study. J Appl Oral Sci. 29:e20201005. https://doi.org/10.1590/1678-7757-2020-1005. DOI: 10.1590/1678-7757-2020-1005. PMID: 34406316. PMCID: PMC8373205. PMID: 72bffb4a29b54ff89f1e2cb74f8ef9ea.4. Lyon GR, Shaywitz SE, Shaywitz BA. 2003; A definition of dyslexia. Ann Dyslexia. 53:1–14. https://doi.org/10.1007/s11881-003-0001-9. DOI: 10.1007/s11881-003-0001-9.5. Shaywitz SE, Shaywitz JE, Shaywitz BA. 2021; Dyslexia in the 21st century. Curr Opin Psychiatry. 34:80–6. https://doi.org/10.1097/YCO.0000000000000670. DOI: 10.1097/YCO.0000000000000670. PMID: 33278155.
Article6. Capellini SA, Coppede AC, Valle TR. 2010; Fine motor function of school-aged children with dyslexia, learning disability and learning difficulties. Pro Fono. 22:201–8. Portuguese. https://doi.org/10.1590/s0104-56872010000300008. DOI: 10.1590/S0104-56872010000300008. PMID: 21103706.7. Chaix Y, Albaret JM, Brassard C, Cheuret E, de Castelnau P, Benesteau J, et al. 2007; Motor impairment in dyslexia: the influence of attention disorders. Eur J Paediatr Neurol. 11:368–74. https://doi.org/10.1016/j.ejpn.2007.03.006. DOI: 10.1016/j.ejpn.2007.03.006. PMID: 17467315.
Article8. Stoodley CJ. 2016; The cerebellum and neurodevelopmental disorders. Cerebellum. 15:34–7. https://doi.org/10.1007/s12311-015-0715-3. DOI: 10.1007/s12311-015-0715-3. PMID: 26298473. PMCID: PMC4811332.
Article9. Nicolson RI, Fawcett AJ, Dean P. 2001; Developmental dyslexia: the cerebellar deficit hypothesis. Trends Neurosci. 24:508–11. https://doi.org/10.1016/s0166-2236(00)01896-8. DOI: 10.1016/S0166-2236(00)01896-8. PMID: 11506881.
Article10. Nicolson RI, Fawcett AJ, Berry EL, Jenkins IH, Dean P, Brooks DJ. 1999; Association of abnormal cerebellar activation with motor learning difficulties in dyslexic adults. Lancet. 353:1662–7. https://doi.org/10.1016/S0140-6736(98)09165-X. DOI: 10.1016/S0140-6736(98)09165-X. PMID: 10335786.
Article11. Smith AM. 1993; Babinski and movement synergism. Rev Neurol (Paris). 149:764–70. French. https://pubmed.ncbi.nlm.nih.gov/7997735/. PMID: 7997735.12. Cheng HY, Murdoch BE, Goozée JV, Scott D. 2007; Physiologic development of tongue-jaw coordination from childhood to adulthood. J Speech Lang Hear Res. 50:352–60. https://doi.org/10.1044/1092-4388(2007/025). DOI: 10.1044/1092-4388(2007/025). PMID: 17463234.13. Perillo L, Esposito M, Contiello M, Lucchese A, Santini AC, Carotenuto M. 2013; Occlusal traits in developmental dyslexia: a preliminary study. Neuropsychiatr Dis Treat. 9:1231–7. https://doi.org/10.2147/NDT.S49985. DOI: 10.2147/NDT.S49985. PMID: 24009421. PMCID: PMC3762607.
Article14. Shi M, Liu X, Zhang C, Zhang H, Liu Q, Wang D, et al. 2021; Effect of dental malocclusion on cerebellar neuron activation via the dorsomedial part of the principal sensory trigeminal nucleus. Eur J Oral Sci. 129:e12788. https://doi.org/10.1111/eos.12788. DOI: 10.1111/eos.12788. PMID: 33945647. PMCID: PMC8453929.
Article15. Bernstein M. 1954; The relation of speech defects and malocclusion. Am J Orthod. 40:149–50. https://doi.org/10.1016/0002-9416(54)90135-9. DOI: 10.1016/0002-9416(54)90135-9.
Article16. Mogren Å, Havner C, Westerlund A, Sjögreen L, Agholme MB, Mcallister A. 2022; Malocclusion in children with speech sound disorders and motor speech involvement: a cross-sectional clinical study in Swedish children. Eur Arch Paediatr Dent. 23:619–28. https://doi.org/10.1007/s40368-022-00728-4. DOI: 10.1007/s40368-022-00728-4. PMID: 35776286. PMCID: PMC9338153.
Article17. Luconi E, Togni L, Mascitti M, Tesei A, Nori A, Barlattani A, et al. 2021; Bruxism in children and adolescents with Down syndrome: a comprehensive review. Medicina (Kaunas). 57:224. https://doi.org/10.3390/medicina57030224. DOI: 10.3390/medicina57030224. PMID: 33804484. PMCID: PMC7999026. PMID: 985dd6e2683245cd87d205e29ca08570.
Article18. Alessandri-Bonetti A, Guglielmi F, Mollo A, Sangalli L, Gallenzi P. 2023; Prevalence of malocclusions in down syndrome population: a cross-sectional study. Medicina (Kaunas). 59:1657. https://doi.org/10.3390/medicina59091657. DOI: 10.3390/medicina59091657. PMID: 37763776. PMCID: PMC10538151. PMID: 86aaccea8f7841b9b5bf36fd488f397a.19. National Institutes of Health (NIH). 2019. Guidelines for the review of inclusion on the basis of sex/gender, race, ethnicity, and age in clinical research [Internet]. NIH;Bethesda: Available from: https://grants.nih.gov/grants/peer/guidelines_general/Review_Human_subjects_Inclusion.pdf. cited 2024 Feb 13.20. United Nations International Children's Emergency Fund (UNICEF). 1989. Convention on the rights of the child text [Internet]. UNICEF;Available from: https://www.unicef.org/child-rights-convention/convention-text. cited 2024 Feb 13.21. European Commission. 2022. EU action on the rights of the child [Internet]. European Commission;Available from: https://ec.europa.eu/info/policies/justice-and-fundamental-rights/rights-child/eu-action-rights-child_en. cited 2024 Feb 13.22. Re AM, Tressoldi PE, Cornoldi C, Lucangeli D. 2011; Which tasks best discriminate between dyslexic university students and controls in a transparent language? Dyslexia. 17:227–41. https://doi.org/10.1002/dys.431. DOI: 10.1002/dys.431. PMID: 21793120.23. Wechsler D. 1991. Wechsler intelligence scale for children (WISC-IV). 4th ed. The Psychological Corporation;San Antonio: https://www.pearsonassessments.com/store/usassessments/en/Store/Professional-Assessments/Cognition-%26-Neuro/Wechsler-Intelligence-Scale-for-Children-%7C-Fourth-Edition/p/100000310.html. DOI: 10.4135/9781412952484.n637.24. dos Santos AAA, Muniz M, Rueda FJM, Martins RMM. 2018; Validity evidence for the 4th edition of the Wechsler Intelligence Scale for Children. PSICO. 49:1–11. https://psycnet.apa.org/record/2018-43143-001. DOI: 10.15448/1980-8623.2018.1.27002.
Article25. Sartori G, Job R, Tressoldi PE. 2007. Battery for the assessment of developmental dyslexia and dysorthographia. Giunti O.S.;Firenze: Italian. https://discovery.sba.uniroma3.it/discovery/fulldisplay?vid=39RM_CABTRE:39CAB_V1&docid=alma990004659710202653&context=L&lang=it.26. Tressoldi PE, Cornoldi C, Re AM. 2013. BVSCO-2: battery for the assessment of writing and spelling proficiency-2. Giunti O.S.;Firenze: Italian. https://discovery.sba.uniroma3.it/discovery/fulldisplay?vid=39RM_CABTRE:39CAB_V1&tab=Everything&docid=alma990005261330202653&context=L&lang=it.27. Cornoldi C, Lucangeli D, Perini N. 2012. AC-MT 6-11- test for the evaluation of calculating and problem solving abilities. Erickson;Trento: Italian. https://www.erickson.it/it/acmt-611-anni-prove-per-la-classe.28. Achenbach TM, Dumenci L. 2001; Advances in empirically based assessment: revised cross-informant syndromes and new DSM-oriented scales for the CBCL, YSR, and TRF: comment on Lengua, Sadowksi, Friedrich, and Fischer (2001). J Consult Clin Psychol. 69:699–702. https://doi.org/10.1037//0022-006X.69.4.699. DOI: 10.1037//0022-006X.69.4.699. PMID: 11550735.
Article29. Achenbach TM. 1991. Manual for child behavior checklist 4-18, 1991 profile. University of Vermont, Department of Psychiatry;Burlington: https://www.amazon.com/Manual-Child-Behavior-Checklist-Profile/dp/0938565087.30. Achenbach TM, Edelbrock C, Howell CT. 1987; Empirically based assessment of the behavioral/emotional problems of 2- and 3- year-old children. J Abnorm Child Psychol. 15:629–50. https://doi.org/10.1007/BF00917246. DOI: 10.1007/BF00917246. PMID: 3437096.
Article31. Achenbach TM. 1991. Manual for the Teacher's Report Form and 1991 profile. University of Vermont, Department of Psychiatry;Burlington: https://search.worldcat.org/ko/title/Manual-for-the-Teacher's-Report-Form-and-1991-profile/oclc/476395212. DOI: 10.1007/978-1-4612-4450-9_14.32. Ackerman JL, Proffit WR, Sarver DM. 1999; The emerging soft tissue paradigm in orthodontic diagnosis and treatment planning. Clin Orthod Res. 2:49–52. https://doi.org/10.1111/ocr.1999.2.2.49. DOI: 10.1111/ocr.1999.2.2.49. PMID: 10534979.33. Salzmann JA. 1965; The angle classification as a parameter of malocclusion. Am J Orthod. 51:465–6. https://doi.org/10.1016/0002-9416(65)90243-5. DOI: 10.1016/0002-9416(65)90243-5. PMID: 14287832.
Article34. Vajaria R, BeGole E, Kusnoto B, Galang MT, Obrez A. 2011; Evaluation of incisor position and dental transverse dimensional changes using the Damon system. Angle Orthod. 81:647–52. https://doi.org/10.2319/071910-420.1. DOI: 10.2319/071910-420.1. PMID: 21446870. PMCID: PMC8919756.
Article35. Littlewood SJ, Mitchell L. 2019. An introduction to orthodontics. Oxford University Press;Oxford: https://global.oup.com/academic/product/an-introduction-to-orthodontics-9780198808664?cc=kr&lang=en&. DOI: 10.1053/j.sodo.2019.10.007.36. Borzabadi-Farahani A, Borzabadi-Farahani A, Eslamipour F. 2009; Malocclusion and occlusal traits in an urban Iranian population. An epidemiological study of 11- to 14-year-old children. Eur J Orthod. 31:477–84. https://doi.org/10.1093/ejo/cjp031. DOI: 10.1093/ejo/cjp031. PMID: 19477970.37. Emodi-Perlman A, Eli I, Friedman-Rubin P, Goldsmith C, Reiter S, Winocur E. 2012; Bruxism, oral parafunctions, anamnestic and clinical findings of temporomandibular disorders in children. J Oral Rehabil. 39:126–35. https://doi.org/10.1111/j.1365-2842.2011.02254.x. DOI: 10.1111/j.1365-2842.2011.02254.x. PMID: 21916926.38. Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne GJ, et al. 2013; Bruxism defined and graded: an international consensus. J Oral Rehabil. 40:2–4. https://doi.org/10.1111/joor.12011. DOI: 10.1111/joor.12011. PMID: 23121262.
Article39. Brookes RL, Stirling J. 2005; The cerebellar deficit hypothesis and dyslexic tendencies in a non-clinical sample. Dyslexia. 11:174–85. https://doi.org/10.1002/dys.293. DOI: 10.1002/dys.293. PMID: 16128047.
Article40. Fawcett AJ, Nicolson RI, Dean P. 1996; Impaired performance of children with dyslexia on a range of cerebellar tasks. Ann Dyslexia. 46:259–83. https://doi.org/10.1007/BF02648179. DOI: 10.1007/BF02648179. PMID: 24234275.41. Fawcett AJ, Nicolson RI. 1999; Performance of dyslexic children on cerebellar and cognitive tests. J Mot Behav. 31:68–78. https://doi.org/10.1080/00222899909601892. DOI: 10.1080/00222899909601892. PMID: 11177620.
Article42. Fiez JA, Petersen SE, Cheney MK, Raichle ME. 1992; Impaired non-motor learning and error detection associated with cerebellar damage. A single case study. Brain. 115(1):155–78. https://doi.org/10.1093/brain/115.1.155. DOI: 10.1093/brain/115.1.155. PMID: 1559151.
Article43. Gonçalves FM, Taveira KVM, Araujo CM, Ravazzi GMNC, Guariza Filho O, Zeigelboim BS, et al. 2023; Association between atypical swallowing and malocclusions: a systematic review. Dental Press J Orthod. 27:e2221285. https://doi.org/10.1590/2177-6709.27.6.e2221285.oar. DOI: 10.1590/2177-6709.27.6.e2221285.oar. PMID: 36995845. PMCID: PMC10042461. PMID: 205b1f7ef2c9490abecb11f1d6cc8045.
Article44. Dillon M, D'Souza E, Edwards I. 2022; Neurodiversity and orthodontic treatment. Orthod Update. 15:132–5. https://doi.org/10.12968/ortu.2022.15.3.132. DOI: 10.12968/ortu.2022.15.3.132.45. Cabaraux P, Agrawal SK, Cai H, Calabro RS, Casali C, Damm L, et al. 2023; Consensus paper: ataxic gait. Cerebellum. 22:394–430. https://doi.org/10.1007/s12311-022-01373-9. Erratum in: Cerebellum 2023;22:431-2. DOI: 10.1007/s12311-022-01413-4. PMID: 35536510.
Article46. Cenzato N, Nobili A, Maspero C. 2021; Prevalence of dental malocclusions in different geographical areas: scoping review. Dent J (Basel). 9:117. https://doi.org/10.3390/dj9100117. DOI: 10.3390/dj9100117. PMID: 34677179. PMCID: PMC8534899. PMID: 36198757c4c34e2e89ea47ed406d3b60.
Article47. Alessandri-Bonetti A, Guglielmi F, Deledda G, Sangalli L, Brogna C, Gallenzi P. 2024; Malocclusions, sleep bruxism, and obstructive sleep apnea risk in pediatric ADHD patients: a prospective study. J Atten Disord. 28:1017–23. https://doi.org/10.1177/10870547231226139. DOI: 10.1177/10870547231226139. PMID: 38327066.48. Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. 2008; Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 35:476–94. https://doi.org/10.1111/j.1365-2842.2008.01881.x. DOI: 10.1111/j.1365-2842.2008.01881.x. PMID: 18557915.
Article49. Okumuş HG, Akdemir D. 2023; Body focused repetitive behavior disorders: behavioral models and neurobiological mechanisms. Turk Psikiyatri Derg. 34:50–9. https://doi.org/10.5080/u26213. DOI: 10.5080/u26213. PMID: 36970962. PMCID: PMC10552165.
Article50. Jenkins DG, Quintana-Ascencio PF. 2020; A solution to minimum sample size for regressions. PLoS One. 15:e0229345. https://doi.org/10.1371/journal.pone.0229345. DOI: 10.1371/journal.pone.0229345. PMID: 32084211. PMCID: PMC7034864. PMID: d1d3b0b19caa48f4a01d88ce93281f6e.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neuropsychological Assessment for Verbal Function
- Recent update on reading disability (dyslexia) focused on neurobiology
- The prevalence of temporomandibular disorders in 16~18 aged subjects at Yongin, Kyungkido, Korea
- Reliability of a Tablet Computer-Based Dyslexia Screening Application Using an Eye-Tracking System
- Developmental Assessment in Pediatric Practice