J Korean Med Sci.
2024 Jul;39(29):e217. 10.3346/jkms.2024.39.e217.
Long-Term Outcome of Time-Staged Gamma Knife Radiosurgery for Large Arteriovenous Malformations
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Neurosurgery, Pusan National University Hospital, Busan, Korea
- 3Department of Neurosurgery, Chungnam National University Sejong Hospital, Sejong, Korea
- 4Department of Neurosurgery, Gachon University Gil Medical Center, Incheon, Korea
- 5Department of Neurosurgery, Soonchunhyang University Seoul Hospital, Seoul, Korea
- 6Department of Internal Medicine, Chung-Ang University Gwangmyeong Hospital, Chung-Ang University College of Medicine, Gwangmyeong, Korea
- 7Department of Human Systems Medicine, Medical Statistics Laboratory, Seoul National University College of Medicine, Seoul, Korea
- 8Department of Neurosurgery, Cancer Research Institute and Ischemic/Hypoxic Disease Institute, Seoul National University College of Medicine, Seoul, Korea
- 9Advanced Institute of Convergence Technology, Seoul National University, Suwon, Korea
- KMID: 2558260
- DOI: http://doi.org/10.3346/jkms.2024.39.e217
Abstract
- Background
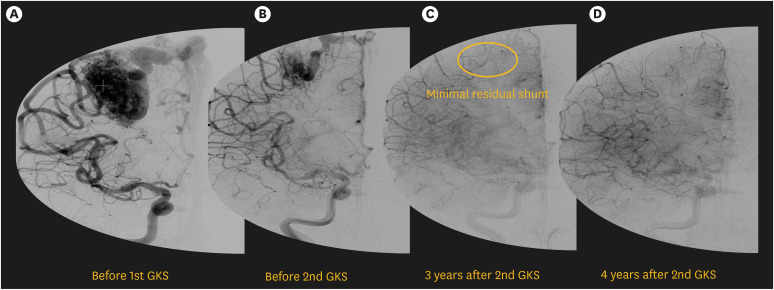
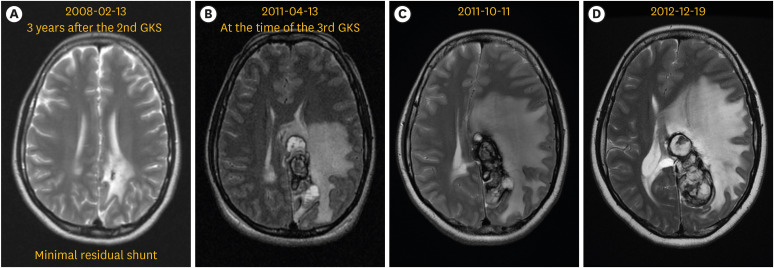
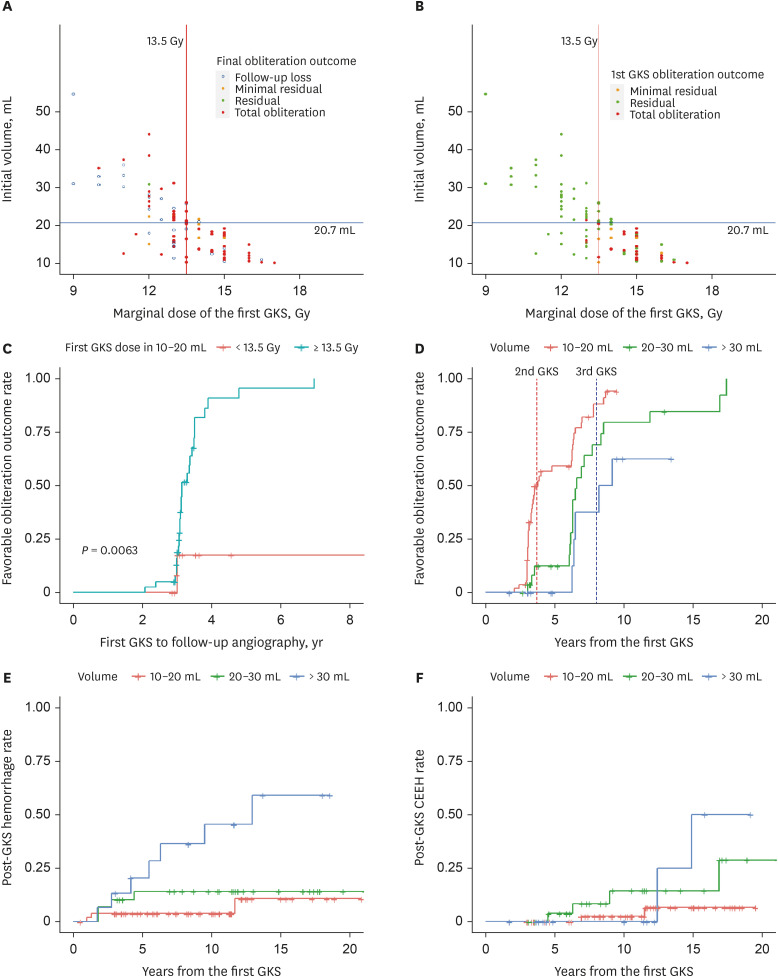
Treatment for large (> 10 mL) arteriovenous malformations (AVMs) remains highly challenging. This study evaluated long-term effect of time-staged gamma knife radiosurgery (GKS) for large AVMs. Methods: For patients with large AVMs treated by time-staged GKS over 10 years, timestaged GKS was repeated every three years targeting the entire nidus if total obliteration was not achieved. Obliteration rate and post-GKS complications were assessed based on 10 mL volume interval of AVMs. Prognostic factors for these outcomes were evaluated using Cox regression analysis.
Results
Ninety-six patients were analyzed. For AVMs in the 10–20 mL subgroup, a dose ≥ 13.5Gy yielded higher obliteration rate in the first GKS. In the 20–30 mL subgroup, a second GKS significantly boosted obliteration. AVMs > 30 mL did not achieve any obliteration with the first GKS. Among 35 (36.4%) cases lost to follow-up, 7 (7.2%) were lost due to GKS complications. Kaplan-Meier analysis showed that each subgroup needed different time for achieving 50% favorable obliteration outcome rate: 3.5, 6.5, and 8.2 years for 10–20 mL, 20–30 mL, and > 30 mL subgroup, respectively. Total obliteration rate calculated by intention-to-treat method: 73%, 51.7%, 35.7%, respectively, 61.5% overall. Post-GKS hemorrhage and chronic encapsulated expanding hematoma (CEEH) occurred in 13.5% and 8.3% of cases, respectively. Two patients died. Dose and volume were significant prognostic factors for obliteration. Initial AVM volume was a significant prognostic factor of post-GKS hemorrhage and CEEH.
Conclusion
Time-staged GKS for large AVMs less than 30 mL has highly favorable long-term outcome and a tolerable complication rate.
Keyword
Figure
Reference
-
1. Pan DH, Guo WY, Chung WY, Shiau CY, Chang YC, Wang LW. Gamma knife radiosurgery as a single treatment modality for large cerebral arteriovenous malformations. J Neurosurg. 2000; 93(Suppl 3):113–119.2. Lunsford LD, Kondziolka D, Flickinger JC, Bissonette DJ, Jungreis CA, Maitz AH, et al. Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg. 1991; 75(4):512–524. PMID: 1885968.3. Mathis JA, Barr JD, Horton JA, Jungreis CA, Lunsford LD, Kondziolka DS, et al. The efficacy of particulate embolization combined with stereotactic radiosurgery for treatment of large arteriovenous malformations of the brain. AJNR Am J Neuroradiol. 1995; 16(2):299–306. PMID: 7726076.4. Seymour ZA, Sneed PK, Gupta N, Lawton MT, Molinaro AM, Young W, et al. Volume-staged radiosurgery for large arteriovenous malformations: an evolving paradigm. J Neurosurg. 2016; 124(1):163–174. PMID: 26140495.5. Sirin S, Kondziolka D, Niranjan A, Flickinger JC, Maitz AH, Lunsford LD. Prospective staged volume radiosurgery for large arteriovenous malformations: indications and outcomes in otherwise untreatable patients. Neurosurgery. 2008; 62(Suppl 2):744–754. PMID: 18596431.6. Karlsson B, Jokura H, Yamamoto M, Söderman M, Lax I. Is repeated radiosurgery an alternative to staged radiosurgery for very large brain arteriovenous malformations? J Neurosurg. 2007; 107(4):740–744. PMID: 17937217.7. Yang SY, Kim DG, Chung HT, Paek SH, Park JH, Han DH. Radiosurgery for large cerebral arteriovenous malformations. Acta Neurochir (Wien). 2009; 151(2):113–124. PMID: 19209384.8. Kim HY, Chang WS, Kim DJ, Lee JW, Chang JW, Kim DI, et al. Gamma Knife surgery for large cerebral arteriovenous malformations. J Neurosurg. 2010; 113(Suppl):2–8. PMID: 21121781.9. Park HR, Lee JM, Kim JW, Han JH, Chung HT, Han MH, et al. Time-staged gamma knife stereotactic radiosurgery for large cerebral arteriovenous malformations: a preliminary report. PLoS One. 2016; 11(11):e0165783. PMID: 27806123.10. Han JH, Kim DG, Chung HT, Park CK, Paek SH, Kim JE, et al. Clinical and neuroimaging outcome of cerebral arteriovenous malformations after gamma knife surgery: analysis of the radiation injury rate depending on the arteriovenous malformation volume. J Neurosurg. 2008; 109(2):191–198. PMID: 18671629.11. Karlsson B, Lindquist C, Steiner L. Prediction of obliteration after gamma knife surgery for cerebral arteriovenous malformations. Neurosurgery. 1997; 40(3):425–430. PMID: 9055280.12. Veznedaroglu E, Andrews DW, Benitez RP, Downes MB, Werner-Wasik M, Rosenstock J, et al. Fractionated stereotactic radiotherapy for the treatment of large arteriovenous malformations with or without previous partial embolization. Neurosurgery. 2008; 62(Suppl 2):763–775. PMID: 18596429.13. Lee SH, Lim YJ, Choi SK, Kim TS, Rhee BA. Radiosurgical considerations in the treatment of large cerebral arteriovenous malformations. J Korean Neurosurg Soc. 2009; 46(4):378–384. PMID: 19893730.14. Kano H, Kondziolka D, Flickinger JC, Park KJ, Parry PV, Yang HC, et al. Stereotactic radiosurgery for arteriovenous malformations, part 6: multistaged volumetric management of large arteriovenous malformations. J Neurosurg. 2012; 116(1):54–65. PMID: 22077447.15. Nagy G, Grainger A, Hodgson TJ, Rowe JG, Coley SC, Kemeny AA, et al. Staged-volume radiosurgery of large arteriovenous malformations improves outcome by reducing the rate of adverse radiation effects. Neurosurgery. 2017; 80(2):180–192. PMID: 28173493.16. El-Shehaby AMN, Reda WA, Abdel Karim KM, Emad Eldin RM, Nabeel AM, Tawadros SR. Volume-staged gamma knife radiosurgery for large brain arteriovenous malformation. World Neurosurg. 2019; 132:e604–e612. PMID: 31442655.17. Kjellberg RN. Isoeffective Dose Parameters for Brain Necrosis in Relation to Proton Radiosurgical Dosimetry. Amsterdam, Netherlands: Elsevier/North-Holland Biomedical Press;1979.18. Lee CC, Pan DH, Ho DM, Wu HM, Chung WY, Liu KD, et al. Chronic encapsulated expanding hematoma after gamma knife stereotactic radiosurgery for cerebral arteriovenous malformation. Clin Neurol Neurosurg. 2011; 113(8):668–671. PMID: 21507569.19. Park JC, Ahn JS, Kwon DH, Kwun BD. Growing organized hematomas following gamma knife radiosurgery for cerebral arteriovenous malformation: five cases of surgical excision. J Korean Neurosurg Soc. 2015; 58(1):83–88. PMID: 26279820.20. Kurita H, Sasaki T, Kawamoto S, Taniguchi M, Kitanaka C, Nakaguchi H, et al. Chronic encapsulated expanding hematoma in association with gamma knife stereotactic radiosurgery for a cerebral arteriovenous malformation. Case report. J Neurosurg. 1996; 84(5):874–878. PMID: 8622164.21. Karlsson B, Jokura H, Yang HC, Yamamoto M, Martinez-Alvarez R, Kawagishi J, et al. Risk for hemorrhage the first 2 years after gamma knife surgery for arteriovenous malformations: an update. Neurosurgery. 2022; 91(6):920–927. PMID: 36219806.22. Pinzi V, Marchetti M, Viola A, Tramacere I, Cane I, Iezzoni C, et al. Hypofractionated radiosurgery for large or in critical-site intracranial meningioma: results of a phase 2 prospective study. Int J Radiat Oncol Biol Phys. 2023; 115(1):153–163. PMID: 36075299.23. Nahum AE. The radiobiology of hypofractionation. Clin Oncol (R Coll Radiol). 2015; 27(5):260–269. PMID: 25797579.24. Franzin A, Panni P, Spatola G, Del Vecchio A, Gallotti AL, Gigliotti CR, et al. Results of volume-staged fractionated gamma knife radiosurgery for large complex arteriovenous malformations: obliteration rates and clinical outcomes of an evolving treatment paradigm. J Neurosurg. 2016; 125(Suppl 1):104–113. PMID: 27903180.25. Yamamoto M, Akabane A, Matsumaru Y, Higuchi Y, Kasuya H, Urakawa Y. Long-term follow-up results of intentional 2-stage gamma knife surgery with an interval of at least 3 years for arteriovenous malformations larger than 10 cm3 . J Neurosurg. 2012; 117(Suppl):126–134. PMID: 23205800.26. Ilyas A, Chen CJ, Ding D, Taylor DG, Moosa S, Lee CC, et al. Volume-staged versus dose-staged stereotactic radiosurgery outcomes for large brain arteriovenous malformations: a systematic review. J Neurosurg. 2018; 128(1):154–164. PMID: 28128692.27. Moosa S, Chen CJ, Ding D, Lee CC, Chivukula S, Starke RM, et al. Volume-staged versus dose-staged radiosurgery outcomes for large intracranial arteriovenous malformations. Neurosurg Focus. 2014; 37(3):E18.28. Heffez DS, Osterdock RJ, Alderete L, Grutsch J. The effect of incomplete patient follow-up on the reported results of AVM radiosurgery. Surg Neurol. 1998; 49(4):373–381. PMID: 9537655.29. Tripepi G, Chesnaye NC, Dekker FW, Zoccali C, Jager KJ. Intention to treat and per protocol analysis in clinical trials. Nephrology (Carlton). 2020; 25(7):513–517. PMID: 32147926.30. Chung WY, Shiau CY, Wu HM, Liu KD, Guo WY, Wang LW, et al. Staged radiosurgery for extra-large cerebral arteriovenous malformations: method, implementation, and results. J Neurosurg. 2008; 109(Suppl):65–72. PMID: 19123890.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrence of pediatric cerebral arteriovenous malformation after obliteration by radiosurgery: a case report
- Radiosurgery for Cerebrovascular Disease
- Gamma Knife Radiosurgery for Arteriovenous Malformations: Past Hope and Present Reality
- Gamma Knife Radiosurgery for Pediatric Arteriovenous Malformations
- How to use Leksell GammaPlan