J Korean Med Sci.
2024 Jul;39(29):e211. 10.3346/jkms.2024.39.e211.
Barriers to Choosing Pediatrics as a Specialty: Insights From a CrossSectional Analysis
- Affiliations
-
- 1Department of Medical Education, Jeonbuk National University Medical School, Jeonju, Korea
- 2Department of Pediatrics, Jeonbuk National University Children’s Hospital, Jeonju, Korea
- 3Research Institute of Clinical Medicine, Jeonbuk National University, Jeonju, Korea
- KMID: 2558248
- DOI: http://doi.org/10.3346/jkms.2024.39.e211
Abstract
- Background
The pediatric field in South Korea is experiencing a significant workforce crisis due to a sharp decline in pediatricians, exacerbated by a decrease in pediatric residents and a series of distressing incidents in pediatric healthcare institutions. No prior studies have explored the waning interest in pediatrics among South Korea’s medical students and interns, which our research seeks to address during a pediatric workforce decline. This study aimed to investigate the declining interest in pediatrics among medical students and interns in South Korea amidst decreasing birth rates. We conducted a comprehensive survey to identify the factors deterring young medical professionals from pursuing a career in pediatrics.
Methods
In this cross-sectional study, in December 2023 we surveyed medical students and interns at Jeonbuk National University and Hospital using a 40-item electronically distributed questionnaire tailored to assess the factors influencing specialty choice, focusing on pediatrics. The participants were divided into the pre-clinical and clinical groups, allowing for analysis across educational stages. The survey covered demographics, perceptions of pediatrics, attitudes toward medical errors, and awareness of critical issues; it included a range of question types to ensure detailed and nuanced data collection.
Results
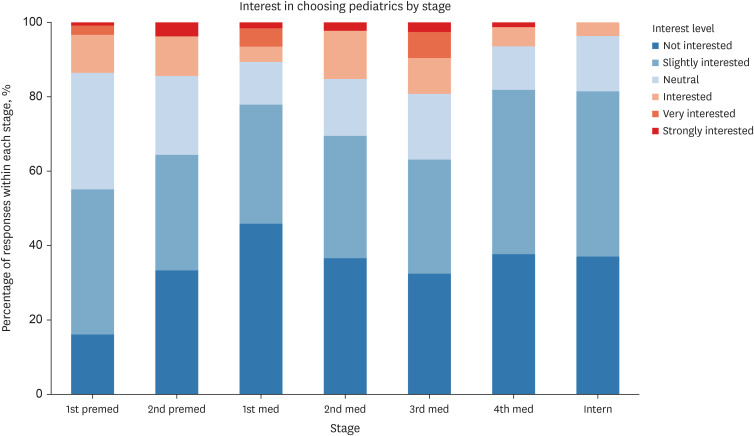
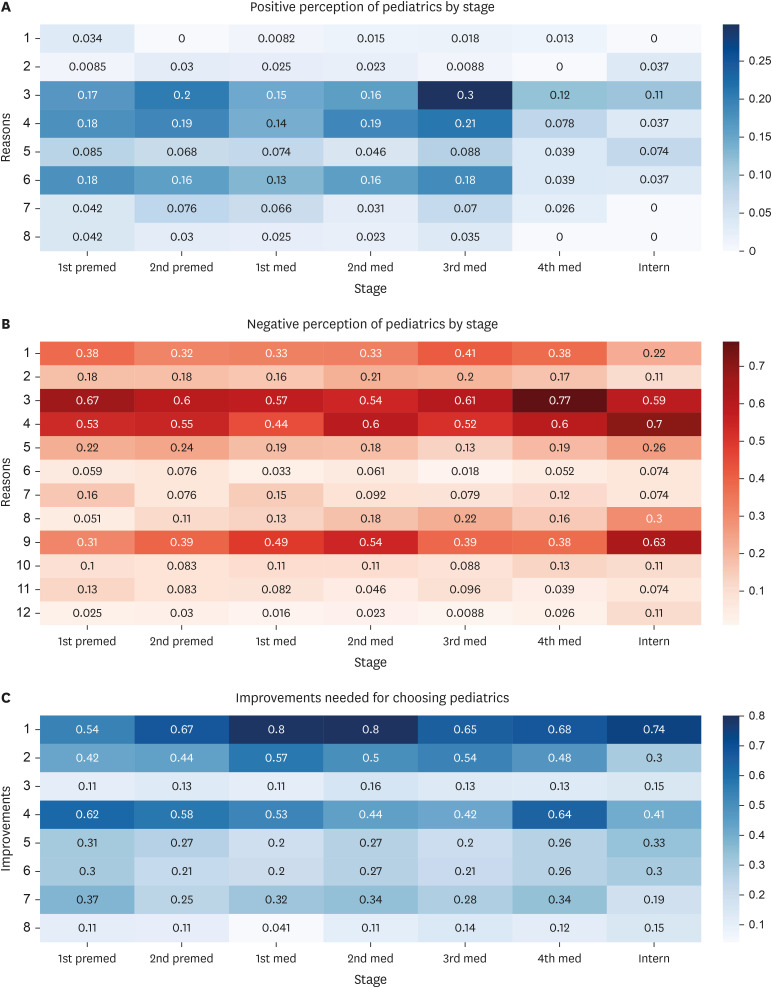
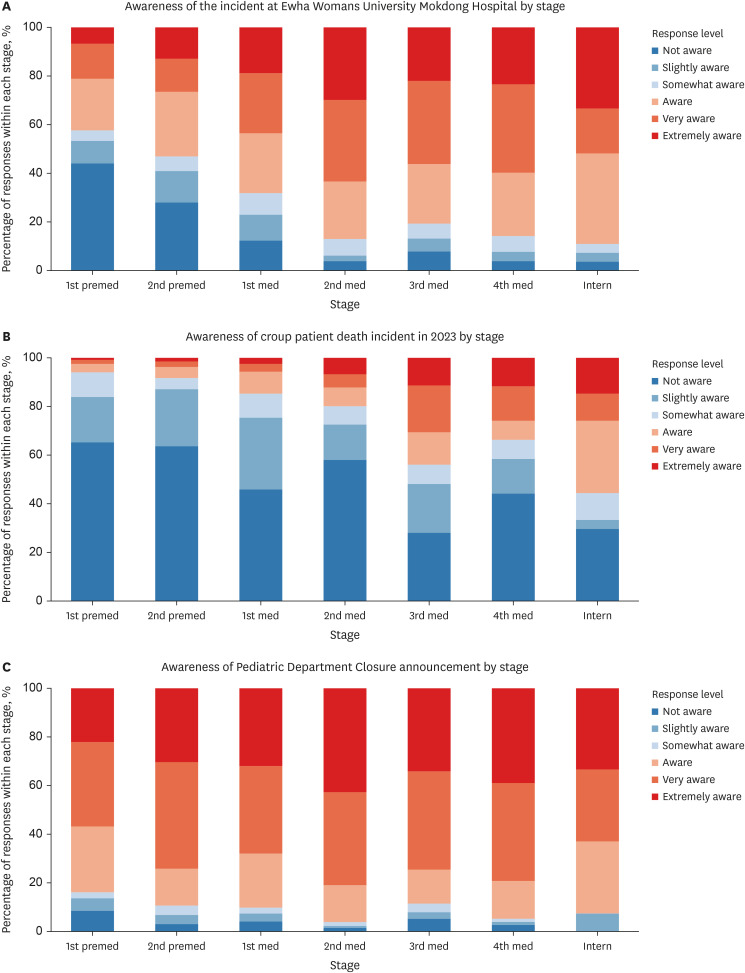
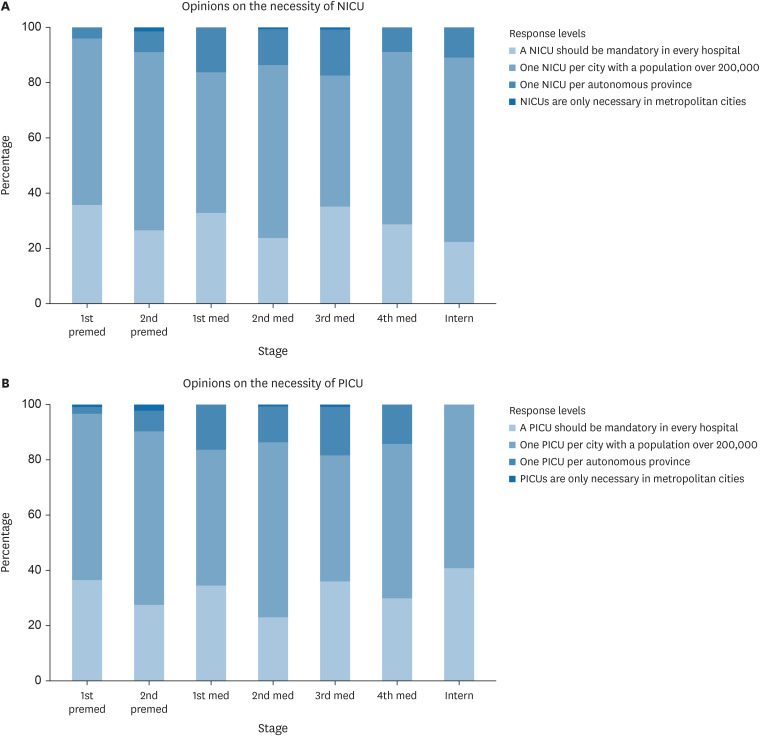
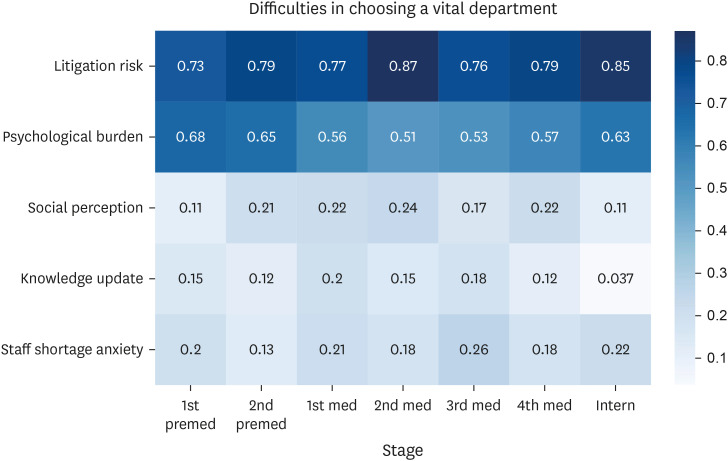
Our findings revealed a clear decrease in interest in pediatrics as medical students progressed through their education, with 86.69% displaying negative views. Although a sense of mission and emotional satisfaction from patient interactions were highlighted as positive influences, they were significantly countered by worries related to declining pediatric populations, legal challenges, and interactions with patient guardians. Additionally, 95.84% of the participants recognized the critical role of vital pediatric departments; however, litigation risks and psychological burdens substantially affected their willingness to specialize in these areas. The analysis also showed an increasing awareness of pediatric incidents as students advanced through their education; however, this did not directly correlate with their choice of specialty (P = 0.090).
Conclusion
The results emphasize the necessity for targeted interventions to alleviate concerns and improve the attractiveness of pediatrics. These efforts are essential to counteract the declining interest and ensure a sustainable pediatric workforce for the future.
Keyword
Figure
Reference
-
1. The Korean Pediatric Society. Updated 2022. Accessed January 19, 2024. https://www.pediatrics.or.kr/bbs/index.html?code=notice&category=&gubun=&page=1&number=13473&mode=view&keyfield=&key= .2. The Korean Society of Neonatology. Updated 2018. Accessed January 19, 2024. https://www.neonatology.or.kr/ .3. The Supreme Court of Korea. Decision on Citrobacter Freundii Infection Leading to Fatal Septicemia. Updated 2022. Accessed April 23, 2024. https://judges.scourt.go.kr/portal/news/NewsViewAction.work?seqnum=4784&gubun=2&searchOption=&searchWord=# .4. Kim J. In an era of low birth rates, support measures for children and adolescents in crisis. Med Policy Forum. 2023; 20(4):48–53.5. Ministry of Health and Welfare. Updated 2023. Accessed January 20, 2024. https://www.mohw.go.kr/board.es?mid=a10504000000&bid=0030&cg_code= .6. Ye RM, Choi YH. Analysis of pediatric emergency medical use and resource changes and medical accessibility. Updated 2023. Accessed May 23, 2024. https://repository.hira.or.kr/handle/2019.oak/3209 .7. Woo BS. Essential medical crisis and medical school capacity. Med Policy Forum. 2023; 21(2):3–6.8. The Korean Pediatric Society. Updated 2023. Accessed January 20, 2024. https://www.pediatrics.or.kr/bbs/index.html?code=notice&category=&gubun=&page=1&number=13931&mode=view&keyfield=all&key= .9. Khamees A, Awadi S, Al Sharie S, Faiyoumi BA, Alzu’bi E, Hailat L, et al. Factors affecting medical student’s decision in choosing a future career specialty: a cross-sectional study. Ann Med Surg (Lond). 2022; 74:103305. PMID: 35145673.10. Al-Beitawi SN, Al-Shatanawi TN, Qudsieh SA, Abu Marar EI, Al Zoubi MS, Al-Zubi M. 6th year medical students’ future specialty preferences: a cross-sectional study. Ann Med Surg (Lond). 2021; 66:102373. PMID: 34040768.11. Alawad AA, Khan WS, Abdelrazig YM, Elzain YI, Khalil HO, Ahmed OB, et al. Factors considered by undergraduate medical students when selecting specialty of their future careers. Pan Afr Med J. 2015; 20:102. PMID: 26090050.12. Smith F, Lambert TW, Goldacre MJ. Factors influencing junior doctors’ choices of future specialty: trends over time and demographics based on results from UK national surveys. J R Soc Med. 2015; 108(10):396–405. PMID: 26432808.13. Roberts C, Vick D, Oakley J. G198(P) Students’ perceptions of paediatrics and the impact of a careers workshop. Arch Dis Child. 2020; 105(Suppl 1):A70–A71.14. Kahvo M, Whelan R, Vallabhaneni P. Why choose paediatrics? A scoping review of factors affecting the choice of paediatrics as a career. Eur J Pediatr. 2023; 182(1):9–23. PMID: 36316579.15. Balmer DF, Gottlieb-Smith RJ, Hobday PM, Long M, Carraccio C, Bale JF, et al. Pediatric career choice: insights from a novel, medical school pathway program. Acad Pediatr. 2020; 20(1):97–103. PMID: 31404708.16. Amudhan AS, Palaniyandi A, Rajan M, Parthiban P, Rajendraprasath S, Saminathan T, et al. The Driving factors important for evaluation student’s opinion which influenced decision making of career choice: pediatrics as a career choice as an example. Acta Inform Med. 2021; 29(2):94–98. PMID: 34584330.17. Shortland D, Roland D, Lumsden DE, Ewing C, L’Esperance V, McColgan M, et al. Career intentions and choices of paediatricians entering training in the UK. Arch Dis Child. 2015; 100(6):537–541. PMID: 25538188.