J Rhinol.
2024 Jul;31(2):119-123. 10.18787/jr.2024.00016.
A Case of Primary Tuberculosis of the Paranasal Sinuses
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, School of Medicine, Kyung Hee University, Seoul, Republic of Korea
- KMID: 2558239
- DOI: http://doi.org/10.18787/jr.2024.00016
Abstract
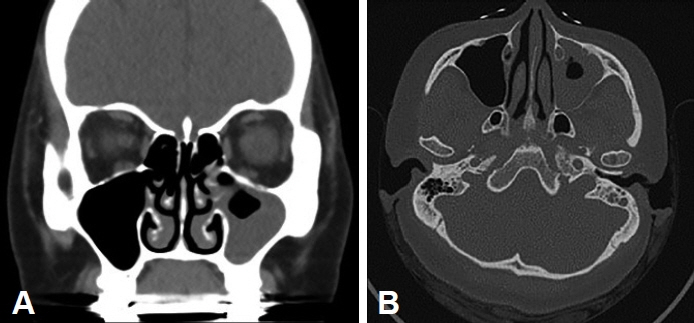
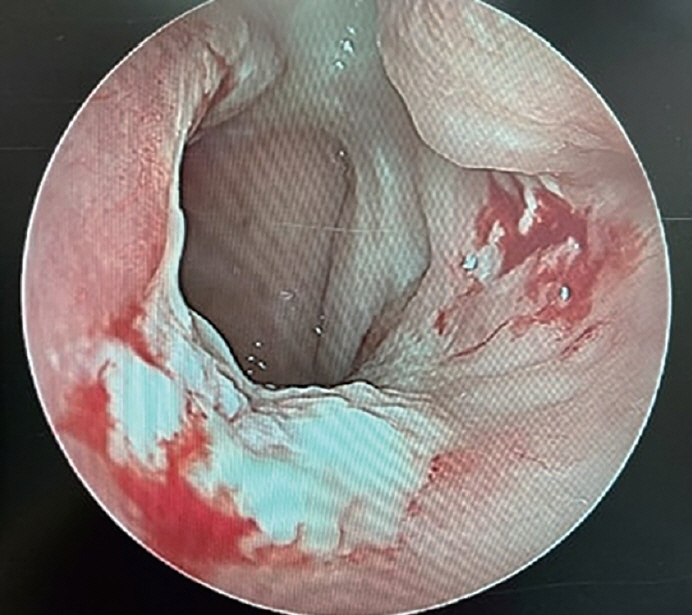
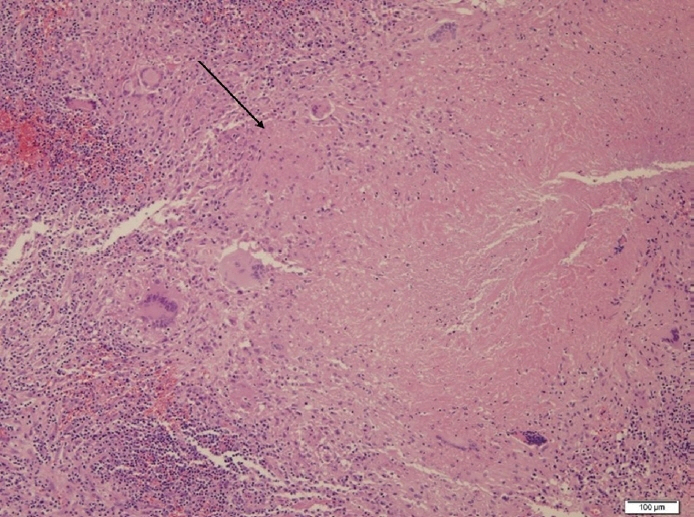
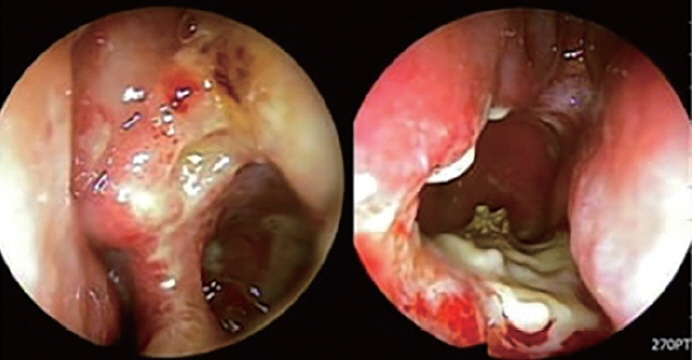
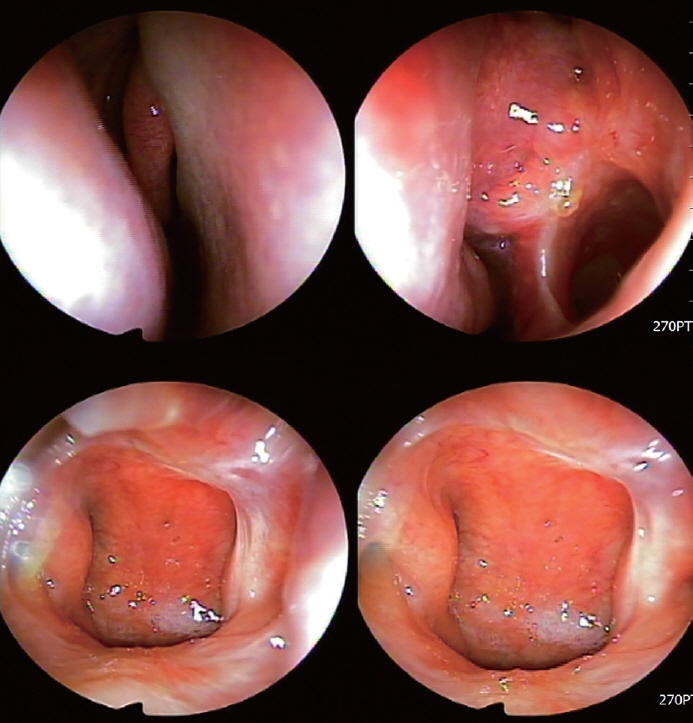
- Tuberculosis of the paranasal sinus is a rare disease caused by infection with Mycobacterium tuberculosis, the causative agent of pulmonary tuberculosis. Although the worldwide incidence of tuberculosis is declining, the diagnosis of primary paranasal tuberculosis remains challenging and cannot be ruled out in patients presenting with refractory chronic rhinosinusitis after adequate surgical and medical treatment. We experienced a case of paranasal tuberculosis with no evidence of previous tuberculosis infection. It was diagnosed after a surgical biopsy revealed granulomatous inflammation and caseous necrosis. The patient responded well to antituberculosis drug therapy and became free of symptoms after 7 months of treatment. We report our findings in this case with a review of the recent literature.
Keyword
Figure
Reference
-
References
1. Kim J, Lee H, In H, Kim Y. [Characteristics of the notified tuberculosis: the Republic of Korea, 2021]. Public Health Wkly Rep. 2022; 15(12):739–46. Korean.2. Lee MS, Kim DJ, Kim MS, Sung KJ, Park DJ. [Sinonasal tuberculosis: report of two cases demonstrated with CT]. J Korean Radiol Soc. 1999; 41(6):1107–9. Korean.3. Sanehi S, Dravid C, Chaudhary N, Venkatachalam VP. Tuberculosis of paranasal sinuses. Indian J Otolaryngol Head Neck Surg. 2008; 60(1):85–7.
Article4. Butt AA. Nasal tuberculosis in the 20th century. Am J Med Sci. 1997; 313(6):332–5.
Article5. Dey S, Misra S, Dutta M. Primary sinonasal tuberculosis: a diagnostic challenge. Turk Arch Otorhinolaryngol. 2018; 56(2):117–21.
Article6. Saha K, Mitra M, Saha A, Barma P. Primary nasal tuberculosis following blunt trauma nose. Med J Dr D.Y. Patil Univ. 2014; 7(1):50–2.7. Sethi A, Agarwal AK, Girhotra M, Naithani P. Tuberculosis: an extremely unusual cause of orbital wall erosion. Orbit. 2011; 30(2):101–4.8. Alavi SM, Nashibi R. Nasal tuberculosis in a 56 year old woman. Caspian J Intern Med. 2014; 5(1):49–51.9. Khan S, Pujani M, Jetley S. Primary nasal tuberculosis: resurgence or coincidence−a report of four cases with review of literature. J Lab Physicians. 2017; 9(1):26–30.10. Jablenska L, Lo S, Uddin J, Toma A. Nasolacrimal tuberculosis: case report highlighting the need for imaging in identifying and managing it effectively. Orbit. 2010; 29(2):126–8.
Article11. Bhandare CA, Barad PS. Lupus vulgaris with endopthalmitis--a rare manifestation of extrapulmonary tuberculosis in India. Indian J Tuberc. 2010; 57(3):98–101.12. Hwang JH, Jin DS, Chai YH, Lee KO. [Two cases of primary tuberculosis arising in nasal cavity]. Korean J Otorhinolaryngol-Head Neck Surg. 1995; 38(8):1273–6. Korean.13. Jennette JC, Falk RJ, Andrassy K, Bacon PA, Churg J, Gross WL, et al. Nomenclature of systemic vasculitides. Arthritis Rheum. 1994; 37(2):187–92.
Article14. Srouji IA, Andrews P, Edwards C, Lund VJ. Patterns of presentation and diagnosis of patients with Wegener’s granulomatosis: ENT aspects. J Laryngol Otol. 2007; 121(7):653–8.
Article15. Cannady SB, Batra PS, Koening C, Lorenz RR, Citardi MJ, Langford C, et al. Sinonasal Wegener granulomatosis: a single-institution experience with 120 cases. Laryngoscope. 2009; 119(4):757–61.
Article16. Aloulah M, Manes RP, Ng YH, Fitzgerald JE, Glazer CS, Ryan MW, et al. Sinonasal manifestations of sarcoidosis: a single institution experience with 38 cases. Int Forum Allergy Rhinol. 2013; 3(7):567–72.
Article17. Wilson R, Lund V, Sweatman M, Mackay IS, Mitchell DN. Upper respiratory tract involvement in sarcoidosis and its management. Eur Respir J. 1988; 1(3):269–72.18. Haverkos BM, Pan Z, Gru AA, Freud AG, Rabinovitch R, Xu-Welliver M, et al. Extranodal NK/T cell lymphoma, nasal type (ENKTL-NT): an update on epidemiology, clinical presentation, and natural history in North American and European cases. Curr Hematol Malig Rep. 2016; 11(6):514–27.
Article19. Trimarchi M, Gregorini G, Facchetti F, Morassi ML, Manfredini C, Maroldi R, et al. Cocaine-induced midline destructive lesions: clinical, radiographic, histopathologic, and serologic features and their differentiation from Wegener granulomatosis. Medicine (Baltimore). 2001; 80(6):391–404.