Clin Endosc.
2024 Jul;57(4):495-500. 10.5946/ce.2023.124.
Prevalence and natural course of incidental gastric subepithelial tumors
- Affiliations
-
- 1Department of Internal Medicine, Presbyterian Medical Center, Jeonju, Korea
- KMID: 2558106
- DOI: http://doi.org/10.5946/ce.2023.124
Abstract
- Background/Aims
Gastric subepithelial tumors (SETs) are often encountered during the upper gastrointestinal endoscopic screening. We assessed the prevalence of gastric SETs and the risk factors for their progression.
Methods
We reviewed the electronic medical records of 30,754 patients who underwent upper gastrointestinal endoscopic screening at our medical center between January 2013 and December 2016.
Results
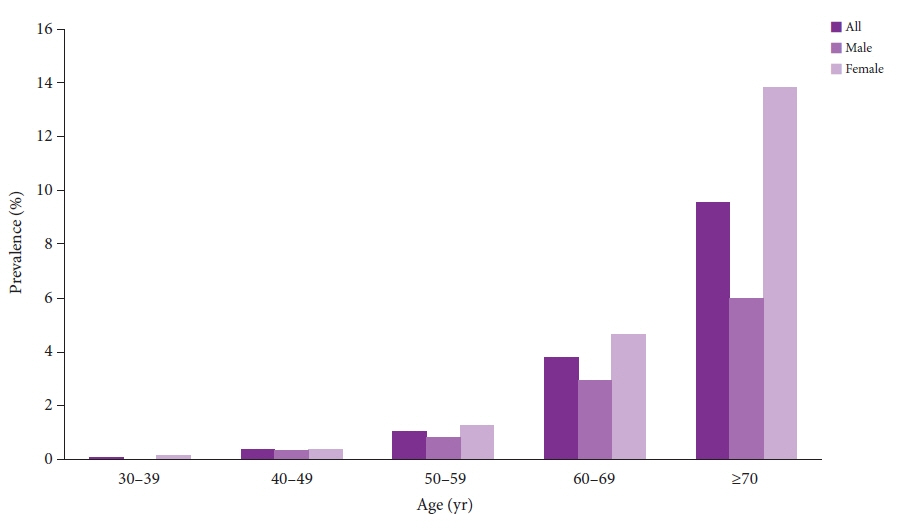
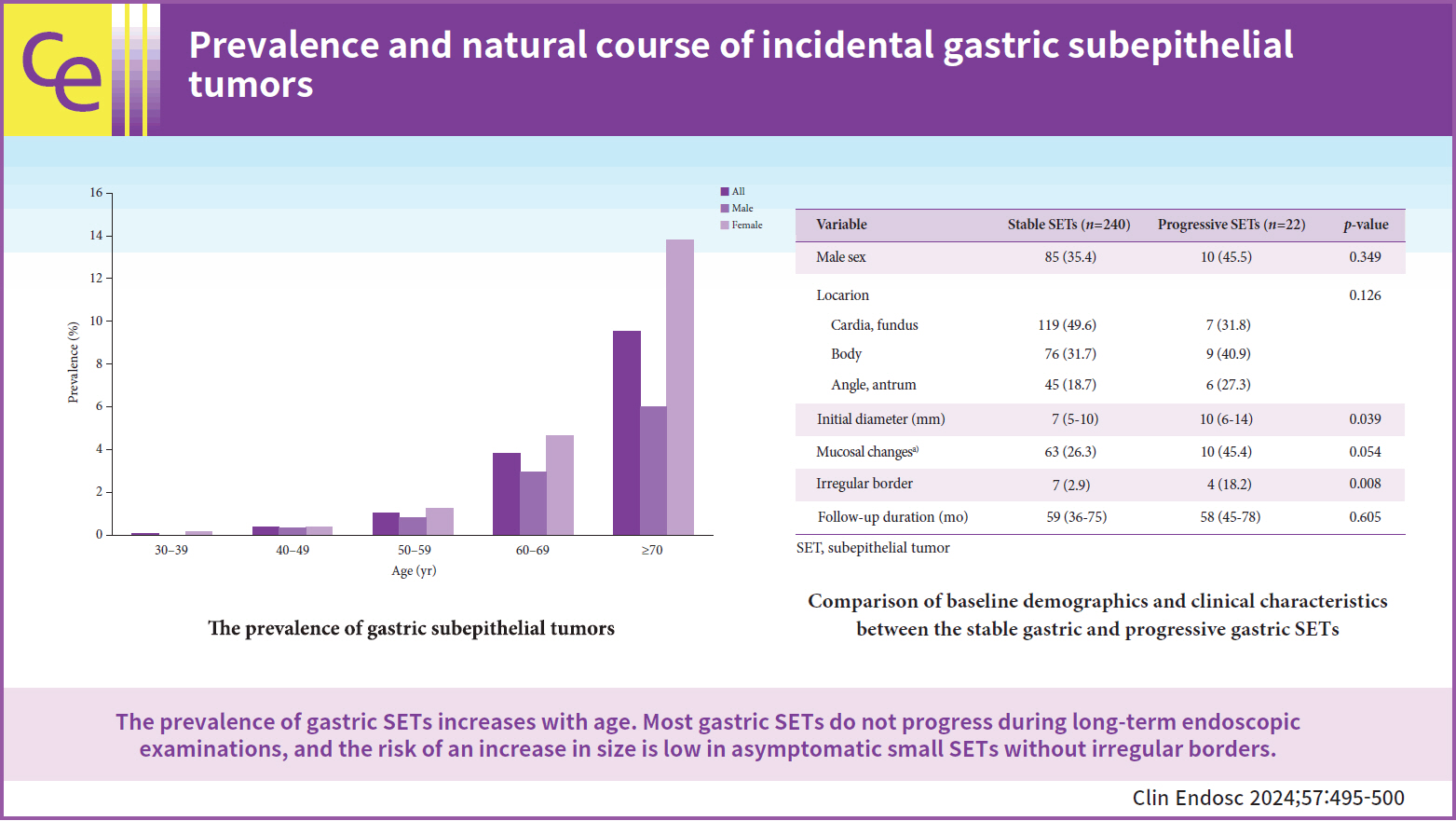
Among the 30,754 patients examined, 599 (1.94%) had gastric SETs. The prevalence increased with age and was 9.56% in patients aged ≥70 years. In total, 262 patients underwent serial endoscopy for more than 6 months. The median age was 68 years (interquartile range [IQR], 61–74), and the number of females was 167 (63.7%). During a median follow-up of 58 months (IQR, 38–75), 22 patients (8.4%) showed significant changes in tumor size. An irregular border (odds ratio, 4.623; 95% confidence interval, 1.093–19.558; p=0.037) was a significant risk factor for progression. Seven patients underwent surgical or endoscopic resections. The pathologies of gastric SETs included leiomyomas (n=3), gastrointestinal stromal tumors (n=2), and lipomas (n=2).
Conclusions
The prevalence of gastric SETs increases with age. Most gastric SETs do not progress during long-term endoscopic examinations, and the risk of an increase in size is low in asymptomatic small SETs without irregular borders.
Figure
Reference
-
1. Cho JW; Korean ESD Study Group. Current guidelines in the management of upper gastrointestinal subepithelial tumors. Clin Endosc. 2016; 49:235–240.
Article2. Lim YJ, Son HJ, Lee JS, et al. Clinical course of subepithelial lesions detected on upper gastrointestinal endoscopy. World J Gastroenterol. 2010; 16:439–444.
Article3. Lee JH, Lee HL, Ahn YW, et al. Prevalence of gastric subepithelial tumors in Korea: a single center experience. Korean J Gastroenterol. 2015; 66:274–276.
Article4. Goto O, Kaise M, Iwakiri K. Advancements in the diagnosis of gastric subepithelial tumors. Gut Liver. 2022; 16:321–330.
Article5. Cho J, Han J, Choi M, et al. Correlation between endoscopic resection outcomes and endosonographic findings in gastric tumors with muscularis propria origin. Medicine (Baltimore). 2022; 101:e29947.
Article6. Kim B, Kang S, Lee E, et al. Gastric subepithelial tumor: long-term natural history and risk factors for progression. Surg Endosc. 2022; 36:5232–5242.
Article7. Kim MY, Jung HY, Choi KD, et al. Natural history of asymptomatic small gastric subepithelial tumors. J Clin Gastroenterol. 2011; 45:330–336.
Article8. Chen H, Li B, Li L, et al. Current status of endoscopic resection of gastric subepithelial tumors. Am J Gastroenterol. 2019; 114:718–725.
Article9. Kim SY, Kim KO. Management of gastric subepithelial tumors: the role of endoscopy. World J Gastrointest Endosc. 2016; 8:418–424.
Article10. Deprez PH, Moons LMG, OʼToole D, et al. Endoscopic management of subepithelial lesions including neuroendocrine neoplasms: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022; 54:412–429.
Article11. Han J, Cho J, Song J, et al. Endoscopic subserosal dissection for gastric tumors: 18 cases in a single center. Surg Endosc. 2022; 36:8039–8046.
Article12. Song JH, Kim SG, Chung SJ, et al. Risk of progression for incidental small subepithelial tumors in the upper gastrointestinal tract. Endoscopy. 2015; 47:675–679.
Article13. Min YW, Park HN, Min BH, et al. Preoperative predictive factors for gastrointestinal stromal tumors: analysis of 375 surgically resected gastric subepithelial tumors. J Gastrointest Surg. 2015; 19:631–638.14. Nishida T, Blay JY, Hirota S, et al. The standard diagnosis, treatment, and follow-up of gastrointestinal stromal tumors based on guidelines. Gastric Cancer. 2016; 19:3–14.
Article