Clin Endosc.
2024 Jul;57(4):454-465. 10.5946/ce.2023.168.
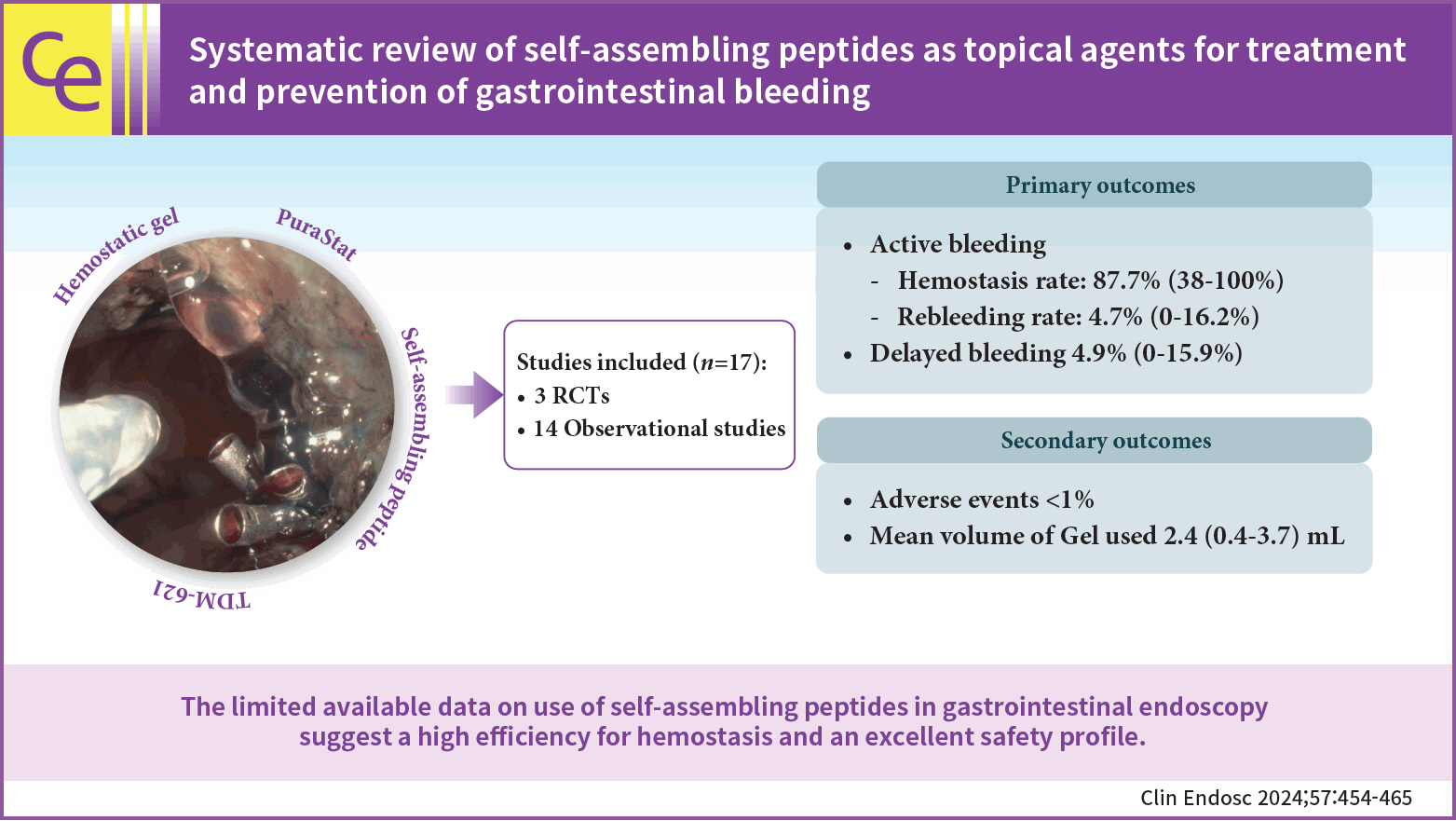
Systematic review of self-assembling peptides as topical agents for treatment and prevention of gastrointestinal bleeding
- Affiliations
-
- 1Gastroenterology Department, Colentina Clinical Hospital, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania
- KMID: 2558099
- DOI: http://doi.org/10.5946/ce.2023.168
Abstract
- Background/Aims
Gastrointestinal bleeding is a significant and potentially lethal event. We aimed to review the efficiency and safety of self-assembling peptides for the treatment and prevention of gastrointestinal tract bleeding.
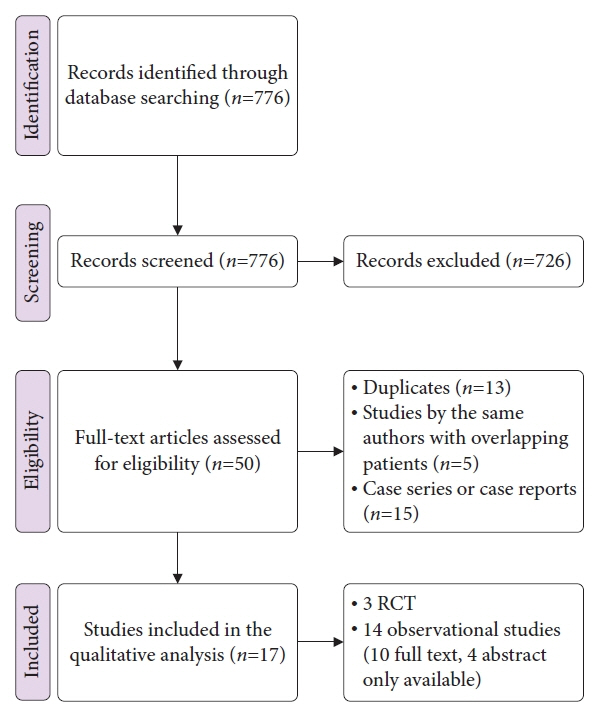
Methods
We conducted a systematic search for studies describing the endoscopic use of self-assembling peptides for treatment or prevention of bleeding in the gastrointestinal tract in a parallel, independent fashion. The primary outcomes were rates of successful initial hemostasis, delayed bleeding, and rebleeding. The secondary outcomes were adverse events and ease and volume of gel used.
Results
Seventeen studies were analyzed. Overall success rate of self-assembling peptides in gastrointestinal bleeding was 87.7% (38%–100%), regardless of etiology or associated treatments. Rebleeding rate ranged from 0% to 16.2%, with a mean of 4.7%, and overall delayed bleeding rate was 5% (range, 0%–15.9%). Only three adverse events were reported in a pooled number of 815 patients. The volume of gel used varied (0.43 to 3.7 mL) according to indication and type of bleeding.
Conclusions
The limited available data on the use of self-assembling peptides in gastrointestinal endoscopy suggest a high efficiency and good safety profile.
Keyword
Figure
Reference
-
1. Laursen SB, Stanley AJ, Laine L, et al. Rebleeding in peptic ulcer bleeding: a nationwide cohort study of 19,537 patients. Scand J Gastroenterol. 2022; 57:1423–1429.
Article2. Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) Guideline: Update 2021. Endoscopy. 2021; 53:300–332.
Article3. ASGE Technology Committee, Parsi MA, Schulman AR, et al. Devices for endoscopic hemostasis of nonvariceal GI bleeding (with videos). VideoGIE. 2019; 4:285–299.
Article4. Voiosu A. Commentary. Endoscopy. 2022; 54:1234–1235.
Article5. Nishiyama N, Kobara H, Kobayashi N, et al. Efficacy of endoscopic ligation with O-ring closure for prevention of bleeding after gastric endoscopic submucosal dissection under antithrombotic therapy: a prospective observational study. Endoscopy. 2022; 54:1078–1084.
Article6. Gangwani MK, Ahuja P, Aziz A, et al. Role of prophylactic hemoclip placement in prevention of delayed post-polypectomy bleeding for large colon polyps: a meta-analysis of randomized controlled trials. Ann Gastroenterol. 2021; 34:392–398.
Article7. Zhang S, Holmes T, Lockshin C, et al. Spontaneous assembly of a self-complementary oligopeptide to form a stable macroscopic membrane. Proc Natl Acad Sci U S A. 1993; 90:3334–3338.
Article8. Ellis-Behnke RG, Liang YX, Tay DK, et al. Nano hemostat solution: immediate hemostasis at the nanoscale. Nanomedicine. 2006; 2:207–215.9. Masuhara H, Fujii T, Watanabe Y, et al. Novel infectious agent-free hemostatic material (TDM-621) in cardiovascular surgery. Ann Thorac Cardiovasc Surg. 2012; 18:444–451.
Article10. Friedland Y, Bagot d’Arc MB, Ha J, et al. The use of self-assembling peptides (PuraStat™) in functional endoscopic sinus surgery for haemostasis and reducing adhesion formation: a case series of 94 patients. Surg Technol Int. 2022; 41:sti41/1594.11. Gangner Y, Bagot d’Arc M, Delin C. The use of self-assembling peptides (PuraStat) for hemostasis in cervical endocrine surgery: a real-life case series of 353 patients. Int J Surg Case Rep. 2022; 94:107072.
Article12. Nahm CB, Popescu I, Botea F, et al. A multi-center post-market clinical study to confirm safety and performance of PuraStat® in the management of bleeding during open liver resection. HPB (Oxford). 2022; 24:700–707.
Article13. U.S. Food and Drug Administration. K210098 [Internet]. U.S. Food and Drug Administration;2021. [cited 2022 Nov 15]. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf21/K210098.pdf.14. Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003; 73:712–716.
Article15. Clark HD, Wells GA, Huët C, et al. Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials. 1999; 20:448–452.16. Arndtz S, Subramaniam S, Hossain E, et al. Outcomes from the UK purastat® registry: multicentre observational study of purastat® use in gastrointestinal bleeding. Gut. 2021; 70:A45–A46.17. Branchi F, Klingenberg-Noftz R, Friedrich K, et al. PuraStat in gastrointestinal bleeding: results of a prospective multicentre observational pilot study. Surg Endosc. 2022; 36:2954–2961.
Article18. Subramaniam S, Kandiah K, Thayalasekaran S, et al. Haemostasis and prevention of bleeding related to ER: the role of a novel self-assembling peptide. United European Gastroenterol J. 2019; 7:155–162.
Article19. Uedo N, Uraoka T, Saito Y, et al. A new hemostatic peptide solution for reduction of electrocauterization during endoscopic submucosal dissection: a multicenter randomized controlled trial. Gastrointest Endosc. 2022; 95(6 Supplement):AB465.
Article20. de Nucci G, Reati R, Arena I, et al. Efficacy of a novel self-assembling peptide hemostatic gel as rescue therapy for refractory acute gastrointestinal bleeding. Endoscopy. 2020; 52:773–779.
Article21. Pioche M, Camus M, Rivory J, et al. A self-assembling matrix-forming gel can be easily and safely applied to prevent delayed bleeding after endoscopic resections. Endosc Int Open. 2016; 4:E415–E419.
Article22. Subramaniam S, Kandiah K, Chedgy F, et al. A novel self-assembling peptide for hemostasis during endoscopic submucosal dissection: a randomized controlled trial. Endoscopy. 2021; 53:27–35.
Article23. Uraoka T, Ochiai Y, Fujimoto A, et al. A novel fully synthetic and self-assembled peptide solution for endoscopic submucosal dissection-induced ulcer in the stomach. Gastrointest Endosc. 2016; 83:1259–1264.
Article24. Soons E, Turan A, van Geenen E, et al. Application of a novel self-assembling peptide to prevent hemorrhage after EMR, a feasibility and safety study. Surg Endosc. 2021; 35:3564–3571.
Article25. Choi JH, Cho IR, Lee SH, et al. Efficacy and safety of novel hemostatic gel in endoscopic sphincterotomy or endoscopic papillectomy: a multicenter, single-blinded, prospective, randomized controlled clinical trial. Gastrointest Endosc. 2022; 95:AB341–AB342.
Article26. Labianca O, Sica M, Zulli C, et al. Use of Purastat in management of gastro-intestinal bleeding: our experience. Endoscopy. 2021; 53:S97–S98.
Article27. White K, Henson CC. Endoscopically delivered Purastat for the treatment of severe haemorrhagic radiation proctopathy: a service evaluation of a new endoscopic treatment for a challenging condition. Frontline Gastroenterol. 2021; 12:608–613.
Article28. Woolley M, Subhaharan D, Bassan M, et al. Efficacy of a novel peptide haemostatic gel in prevention of bleeding post endoscopic resection of large duodenal adenomas. Endoscopy. 2022; 54(S 01):S282.
Article29. Yoshida M, Goto N, Kawaguchi M, et al. Initial clinical trial of a novel hemostat, TDM-621, in the endoscopic treatments of the gastric tumors. J Gastroenterol Hepatol. 2014; 29 Suppl 4:77–79.30. Soriani P, Mirante VG, Barbera C, et al. Novel endoscopic tool to prevent delayed bleeding after wide endoscopic resections in high risk patients: an initial single-centre experience. Dig Liver Dis. 2018; 50:e146.
Article31. Stammers M, Boger P, Patel P, et al. Comparison between 4% formalin instillation and purastat application for radiation proctopathy. Gut. 2021; 70(Suppl 1):A79.32. Ishida Y, Tsuchiya N, Koga T, et al. A novel self-assembling peptide hemostatic gel as an option for initial hemostasis in endoscopic sphincterotomy-related hemorrhage: a case series. Clin J Gastroenterol. 2022; 15:1210–1215.
Article33. Chung IK, Ham JS, Kim HS, et al. Comparison of the hemostatic efficacy of the endoscopic hemoclip method with hypertonic saline-epinephrine injection and a combination of the two for the management of bleeding peptic ulcers. Gastrointest Endosc. 1999; 49:13–18.
Article34. Chung IK, Kim EJ, Lee MS, et al. Bleeding Dieulafoy’s lesions and the choice of endoscopic method: comparing the hemostatic efficacy of mechanical and injection methods. Gastrointest Endosc. 2000; 52:721–724.35. Hamada S, Teramoto A, Zukeyama R, et al. Efficacy of combination therapy with epinephrine local injection and hemostatic clips on active diverticular bleeding. J Clin Med. 2022; 11:5195.
Article36. Sung JJ, Tsoi KK, Lai LH, et al. Endoscopic clipping versus injection and thermo-coagulation in the treatment of non-variceal upper gastrointestinal bleeding: a meta-analysis. Gut. 2007; 56:1364–1373.
Article37. Kataoka M, Kawai T, Hayama Y, et al. Comparison of hemostasis using bipolar hemostatic forceps with hemostasis by endoscopic hemoclipping for nonvariceal upper gastrointestinal bleeding in a prospective non-randomized trial. Surg Endosc. 2013; 27:3035–3038.
Article38. Yuan Y, Wang C, Hunt RH. Endoscopic clipping for acute nonvariceal upper-GI bleeding: a meta-analysis and critical appraisal of randomized controlled trials. Gastrointest Endosc. 2008; 68:339–351.
Article39. Rosenstock SJ, Møller MH, Larsson H, et al. Improving quality of care in peptic ulcer bleeding: nationwide cohort study of 13,498 consecutive patients in the Danish Clinical Register of Emergency Surgery. Am J Gastroenterol. 2013; 108:1449–1457.
Article40. McWhinney CD, Vemulapalli KC, El Rahyel A, et al. Adverse events and residual lesion rate after cold endoscopic mucosal resection of serrated lesions ≥10 mm. Gastrointest Endosc. 2021; 93:654–659.
Article41. Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017; 49:270–297.
Article42. Pimentel-Nunes P, Libânio D, Bastiaansen BA, et al. Endoscopic submucosal dissection for superficial gastrointestinal lesions: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2022. Endoscopy. 2022; 54:591–622.
Article43. Jung DH, Park JC. Strategies that reduce post-endoscopic submucosal dissection bleeding. Korean J Helicobacter Up Gastrointest Res. 2021; 21:194–202.
Article44. 3-D Matrix Medical Technology. PuraStat: the first haemostat approved to reduce delayed bleeding following ESD in the colon [Internet]. 3-D Matrix Medical Technology;2021. [cited 2022 Nov 15]. Available from: https://www.healthcare21.eu/product/purastat/?attachment_id=11084&download_file=t9f02uom9wa1h.45. Cryer BL, Wilcox CM, Henk HJ, et al. The economics of upper gastrointestinal bleeding in a US managed-care setting: a retrospective, claims-based analysis. J Med Econ. 2010; 13:70–77.
Article46. Bartell N, Bittner K, Kaul V, et al. Clinical efficacy of the over-the-scope clip device: a systematic review. World J Gastroenterol. 2020; 26:3495–3516.
Article47. Zhong C, Tan S, Ren Y, et al. Clinical outcomes of over-the-scope-clip system for the treatment of acute upper non-variceal gastrointestinal bleeding: a systematic review and meta-analysis. BMC Gastroenterol. 2019; 19:225.
Article48. Chandrasekar VT, Desai M, Aziz M, et al. Efficacy and safety of over-the-scope clips for gastrointestinal bleeding: a systematic review and meta-analysis. Endoscopy. 2019; 51:941–949.
Article49. Mutneja H, Bhurwal A, Go A, et al. Efficacy of hemospray in upper gastrointestinal bleeding: a systematic review and meta-analysis. J Gastrointestin Liver Dis. 2020; 29:69–76.
Article50. Facciorusso A, Bertini M, Bertoni M, et al. Effectiveness of hemostatic powders in lower gastrointestinal bleeding: a systematic review and meta-analysis. Endosc Int Open. 2021; 9:E1283–E1290.
Article51. Misumi Y, Nonaka K. Prevention and management of complications and education in endoscopic submucosal dissection. J Clin Med. 2021; 10:2511.
Article52. Bishay K, Meng ZW, Frehlich L, et al. Prophylactic clipping to prevent delayed colonic post-polypectomy bleeding: meta-analysis of randomized and observational studies. Surg Endosc. 2022; 36:1251–1262.
Article53. Lau LH, Guo CL, Lee JK, et al. Effectiveness of prophylactic clipping in preventing postpolypectomy bleeding in oral anticoagulant users: a propensity-score analysis. Gastrointest Endosc. 2022; 96:530–542.
Article54. Ayoub F, Westerveld DR, Forde JJ, et al. Effect of prophylactic clip placement following endoscopic mucosal resection of large colorectal lesions on delayed polypectomy bleeding: a meta-analysis. World J Gastroenterol. 2019; 25:2251–2263.
Article55. Forbes N, Gupta S, Frehlich L, et al. Clip closure to prevent adverse events after EMR of proximal large nonpedunculated colorectal polyps: meta-analysis of individual patient data from randomized controlled trials. Gastrointest Endosc. 2022; 96:721–731.
Article56. Yang TC, Wu YH, Lee PC, et al. Prophylactic clipping after endoscopic mucosal resection of large nonpedunculated colorectal lesions: a meta-analysis. J Gastroenterol Hepatol. 2021; 36:1778–1787.
Article57. Nishizawa T, Suzuki H, Goto O, et al. Effect of prophylactic clipping in colorectal endoscopic resection: a meta-analysis of randomized controlled studies. United European Gastroenterol J. 2017; 5:859–867.
Article58. Chen B, Du L, Luo L, et al. Prophylactic clips to reduce delayed polypectomy bleeding after resection of large colorectal polyps: a systematic review and meta-analysis of randomized trials. Gastrointest Endosc. 2021; 93:807–815.
Article59. Qiu J, Xu J, Zhang Y, et al. Over-the-scope clip applications as first-line therapy in the treatment of upper non-variceal gastrointestinal bleeding, perforations, and fistulas. Front Med (Lausanne). 2022; 9:753956.
Article60. Nakahara K, Sekine A, Tateishi K. Self-assembling peptide gel application to achieve endoscopic hemostasis for fistula bleeding after lumen apposing metal stent removal. Dig Endosc. 2023; 35:e48–e49.
Article61. Soriani P, Biancheri P, Deiana S, et al. Off-label PuraStat use for the treatment of acute intrahepatic biliary duct bleeding. Endosc Int Open. 2021; 9:E1926–E1927.
Article62. Kubo K. Delayed bleeding following percutaneous endoscopic gastrostomy successfully treated with PuraStat®. Intern Med. 2023; 62:487–488.
Article63. Karna R, Deliwala S, Ramgopal B, et al. Efficacy of topical hemostatic agents in malignancy-related GI bleeding: a systematic review and meta-analysis. Gastrointest Endosc. 2023; 97:202–208.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcomes and complications of embolization for gastrointestinal bleeding
- Strategies that Reduce Post-endoscopic Submucosal Dissection Bleeding
- Potential Strategies in the Prevention of Nonsteroidal Anti-inflammatory Drugs-Associated Adverse Effects in the Lower Gastrointestinal Tract
- Topical Treatment of Onychomycosis
- Recent Trends in Cyclic Peptides as Therapeutic Agents and Biochemical Tools