Ann Clin Microbiol.
2024 Jun;27(2):69-79. 10.5145/ACM.2024.27.2.4.
Molecular diagnosis of parasitic diseases in Korea
- Affiliations
-
- 1Department of Parasitology and Institute of Medical Education, College of Medicine, Hallym University, Chuncheon, Korea
- KMID: 2557879
- DOI: http://doi.org/10.5145/ACM.2024.27.2.4
Abstract
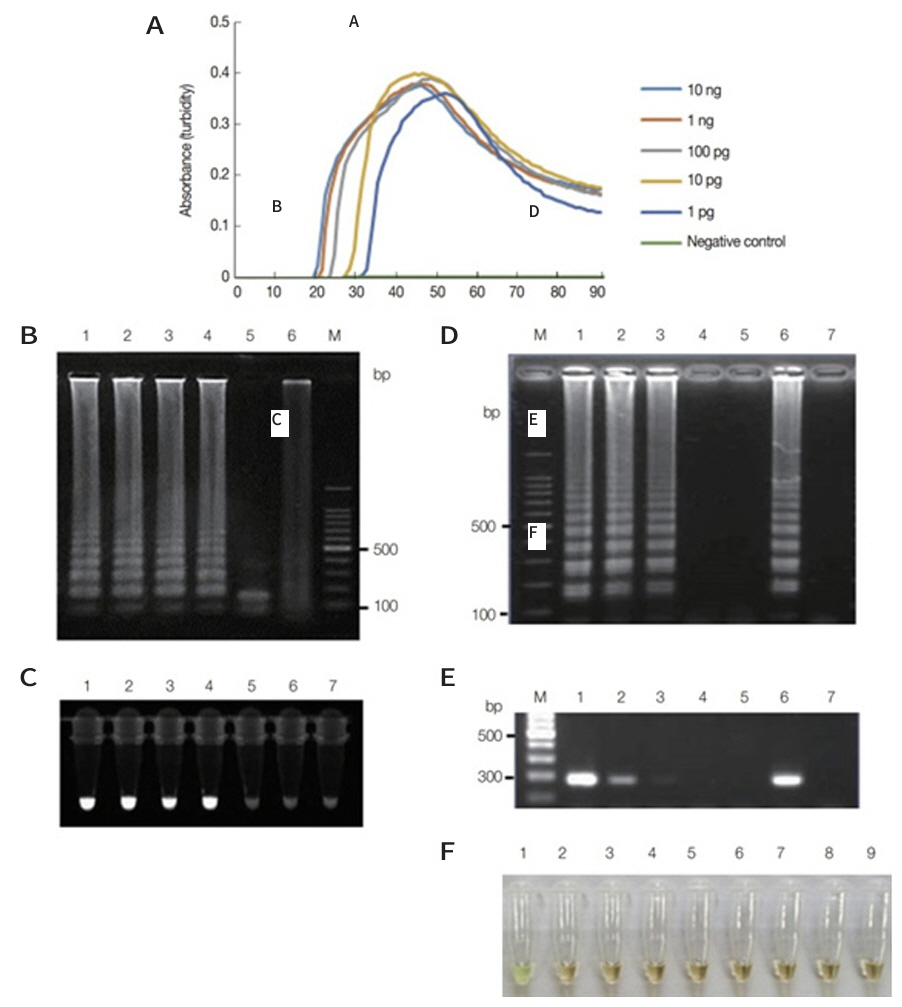
- The aim of this review is to provide practical guidance for the molecular diagnosis of parasitic diseases in Korea in 2024. Specifically, the prevalence of parasitic diseases, commercially available molecular diagnostic kits, and reference laboratories for molecular diagnosis are presented. It is based on the literature and the medical diagnosis device database of the Korea Disease Control and Prevention Agency. In Korea, molecular diagnostic kits are available for intestinal protozoa (Giardia lamblia, Entamoeba histolytica, Cryptosporidium hominis, and Cryptosporidium parvum), Trichomonas vaginalis, and malarial parasites. Molecular diagnosis of other parasites is also possible; however, there is no commercially available kit. Therefore, parasite samples or derivatives for molecular diagnosis should be sent to specific laboratories, the parasitology departments of medical schools, or the Division of Vectors and Parasitic Diseases, Bureau of Infectious Disease Diagnosis Control at the Korea Disease Control and Prevention Agency. In commercial diagnostic kits, multiplex real-time polymerase chain reaction (PCR) is used to rapidly and easily detect the amplified parasitic DNA. The loop-mediated isothermal amplification (LAMP) was developed to diagnose T. vaginalis and Acanthamoeba infections. Its merits are that it does not require a PCR machine and has a short test time of approximately 60 min. Although LAMP is not commercially available, it may be widely used to screen for parasitic diseases. Commercial molecular diagnostic kits for parasitic diseases are limited to the clinical setting in Korea. Available kits are used to diagnose certain intestinal protozoa, T. vaginalis, and to differentiate Plasmodium species using multiplex PCR.
Keyword
Figure
Reference
-
1. Huh S. Status of common parasitic diseases in Korea in 2019. J Korean Med Assoc 2019;62:437-56. .2. Korea Disease Control and Prevention Agency. Sentinel surveillance parasitic infections. https://dportal.kdca.go.kr/pot/is/st/prsts.do [Online] (last visited on 2 April 2024). .3. Korea Disease Control and Prevention Agency. Guidelines for the management of parasite diseases in 2024. https://www.kdca.go.kr/board/board.es?mid=a20507020000&bid=0019&act=view&list_ no=724832 [Online] (last visited on 2 April 2024). .4. Korea Disease Control and Prevention Agency. Malaria statistics. https://dportal.kdca.go.kr/ pot/is/summary.do [Online] (last visited on 2 April 2024). .5. Korea Disease Control and Prevention Agency. Sentinel surveillance intestinal protozoan infections. https://dportal.kdca.go.kr/pot/is/st/gstrnftn.do [Online] (last visited on 2 April 2024). .6. Kim YH, Ahn HJ, Kim D, Nam HW. Spatiotemporal clusters and trend of Trichomonas vaginalis infection in Korea. Korean J Parasitol 2022;60:97-107. .7. Sung GH, Park IJ, Koo HS, Park EH, Lee MO. Molecular detection and genotype analysis of Kudoa septempunctata from food poisoning outbreaks in Korea. Parasites Hosts Dis 2023;61:15-23. .8. Lee E, Park SY, Lee E, Kim TH. Previous long-term care facility admission as a risk factor for scabies in a medical facility. J Korean Med Sci 2021;36:e337. .9. Kim DH, Yun SY, Park YC, Kang SA, Yu HS. Prevalence of scabies in long-term care hospitals in South Korea. PLoS Negl Trop Dis 2020;14:e0008554. .10. Kim H and Lee YW. Current status of scabies in Korea. J Korean Med Assoc 2023;66:696-9. .11. Korea Disease Control and Prevention Agency. Sentinel surveillance of imported parasitic diseases. https://dportal.kdca.go.kr/pot/is/st/gstrnftn.do [Online] (last visited on 2 April 2024). .12. Lee SU, Huh S, Sohn WM, Chai JY. Sequence comparisons of 28S ribosomal DNA and mitochondrial cytochrome c oxidase subunit I of Metagonimus yokogawai, M. takahashii and M. miyatai. Korean J Parasitol 2004;42:129-35 .13. Won EJ, Shin JH, Lee YJ, Kim MJ, Kang SJ, Jung SI, et al. Four taeniasis saginata cases diagnosed at a university hospital in Korea. Korean J Parasitol 2019;57:313-8. .14. Go YB, Lee EH, Cho J, Choi S, Chai JY. Diphyllobothrium nihonkaiense infections in a family. Korean J Parasitol 2015;53:109-12. .15. Song H, Jung BK, Cho J, Chang T, Huh S, Chai JY. Molecular identification of Anisakis larvae extracted by gastrointestinal endoscopy from health check-up patients in Korea. Korean J Parasitol 2019;57:207-211 .16. Madison-Antenucci S, Relich RF, Doyle L, Espina N, Fuller D, Karchmer T, et al. Multicenter evaluation of BD Max Enteric Parasite Real-Time PCR Assay for detection of Giardia duodenalis, Cryptosporidium hominis, Cryptosporidium parvum, and Entamoeba histolytica. J Clin Microbiol 2016;54:2681-8. .17. Yoo J, Park J, Lee HK, Yu JK, Lee GD, Park KG, et al. Comparative evaluation of SeegeneAllplex Gastrointestinal, Luminex xTAG Gastrointestinal Pathogen Panel, and BD MAX Enteric Assays for detection of gastrointestinal pathogens in clinical stool specimens. Arch Pathol Lab Med 2019;143:999-1005. .18. Park HJ, Kim YT, Moon JY, Jin CE, Ko KH, Lee SH, et al. Trend analysis of the profiles of 12 sexually transmitted disease pathogens in the Republic of Korea in 2019. Inquiry 2021;58:469580211065684. .19. Vieira-Baptista P, Silva AR, Costa M, Aguiar T, Saldanha C, Sousa C. Clinical validation of a new molecular test (SeegeneAllplex™ Vaginitis) for the diagnosis of vaginitis: a crosssectional study. BJOG 2021;128:1344-52. .20. Freitas MD, Cardoso FG, Rigo GV, de Melo Machado H, Bazzo ML, Tasca T. Detection of Trichomonas vaginalis by Allplex™ STI Essential Assay (Seegene) in clinical samples from the Brazilian public health system users. Eur J Clin Microbiol Infect Dis 2024;43:167-70. .21. Goo YK, Shin WS, Yang HW, Joo SY, Song SM, Ryu JS, et al. Loop-mediated isothermal amplification targeting actin DNA of Trichomonas vaginalis. Korean J Parasitol 2016;54:329-34. .22. Van Gerwen OT, Camino AF, Sharma J, Kissinger PJ, Muzny CA. Epidemiology, natural history, diagnosis, and treatment of Trichomonas vaginalis in men. Clin Infect Dis 2021;73:1119-24. .23. Hong KW, Jeong JH, Byun JH, Hong SH, Ju JW, Bae IG. Fatal primary amebic meningoencephalitis due to Naegleria fowleri: the first imported case in Korea. Yonsei Med J 2023;64:641-5. .24. Yang HW, Lee YR, Inoue N, Jha BK, Danne DB, Kim HK, et al. Loop-mediated isothermal amplification targeting 18S ribosomal DNA for rapid detection of Acanthamoeba. Korean J Parasitol 2013;51:269-77. .25. Choi W, Kang HG, Choi EY, Kim SS, Kim CY, Koh HJ, et al. Clinical utility of aqueous humor polymerase chain reaction and serologic testing for suspected infectious uveitis: a single-center retrospective study in South Korea. BMC Ophthalmol 2020;20:242. .26. Lee SE, Hong SH, Lee SH, Jeong YI, Lim SJ, Kwon OW, et al. Detection of ocular Toxoplasma gondii infection in chronic irregular recurrent uveitis by PCR. Korean J Parasitol 2012;50:229-31. .27. Korea Disease Control and Prevention Agency. Integrated guidelines for diagnostic tests of notifiable infectious disease in Korea. https://www.kdca.go.kr/board/board.es?mid=a20507020000&bid=0019&ac t=view&list_no=722174 [Online] (last visited on 8 May 2024). .28. Kim H and Lee YW. Current status of scabies in Korea. J Korean Med Assoc 2023;66:696-9. .29. Yu DS and Lee YB. Guideline for the diagnosis and treatment of scabies. J Korean Med Assoc 2023;66:705-11. .30. Bae M, Kim JY, Jung J, Cha HH, Jeon NY, Lee HJ, et al. Diagnostic value of the molecular detection of Sarcoptes scabiei from a skin scraping in patients with suspected scabies. PLoS Negl Trop Dis 2020;14:e0008229. .