J Korean Med Sci.
2024 Jul;39(27):e204. 10.3346/jkms.2024.39.e204.
The Current Incidence and Future Projection of Acetabular Fractures in Korea
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Radiology, We Comfortable Clinic, Seoul, Korea
- 3Department of Orthopaedic Surgery, Chamjoeun Hospital, Gwangju, Korea
- 4Department of Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 5Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2557781
- DOI: http://doi.org/10.3346/jkms.2024.39.e204
Abstract
- Background
As one of the most challenging fractures to orthopedic surgeons, acetabular fractures show a wide range of incidence among countries and regions with even more variance in the treatment modalities. In this study, we aimed to investigate the epidemiology of acetabular fractures, and to compare the rate of subsequent total hip arthroplasty (THA) between nonoperative and operative treatments in South Korea using a medical claims database.
Methods
This was a retrospective study using the Korean Health Insurance Review and Assessment database. Patients admitted for acetabular fractures from January 2007 to December 2018 were identified using International Classification of Diseases-10 codes. Kaplan-Meier survival analysis was used to compare the cumulative incidence of THA between two groups. We also evaluated the survivorship of operative group according to the type of institutions.
Results
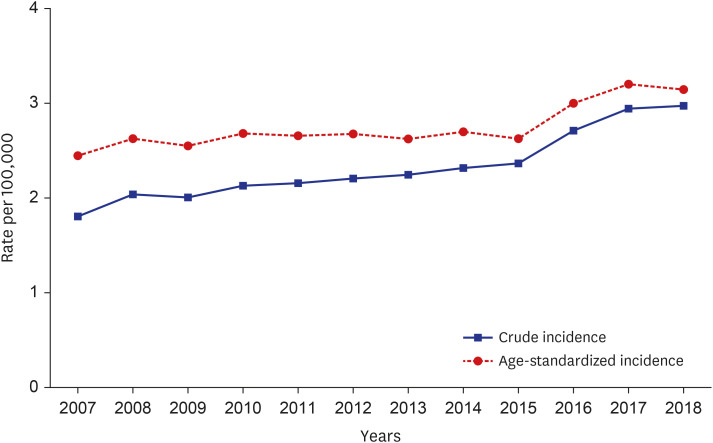
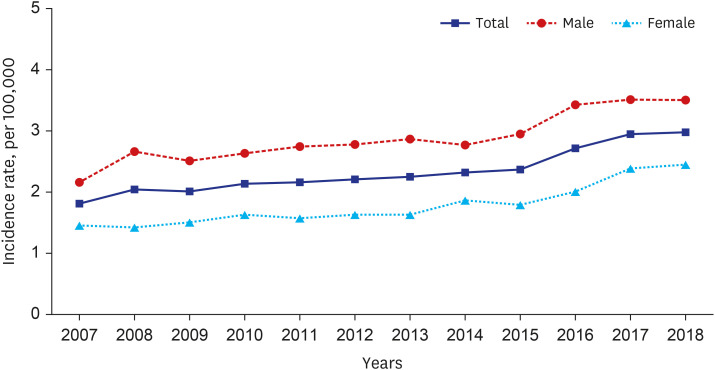
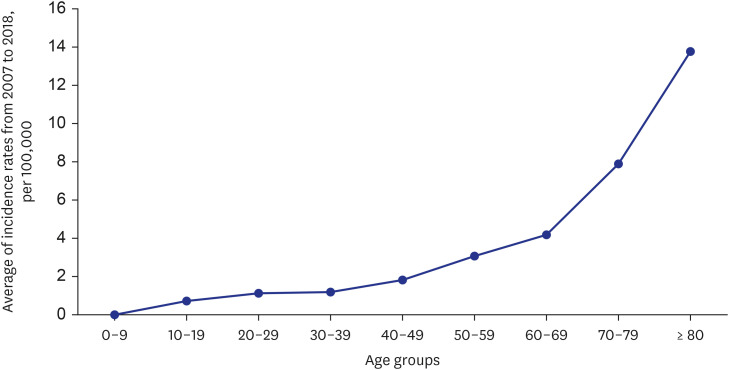
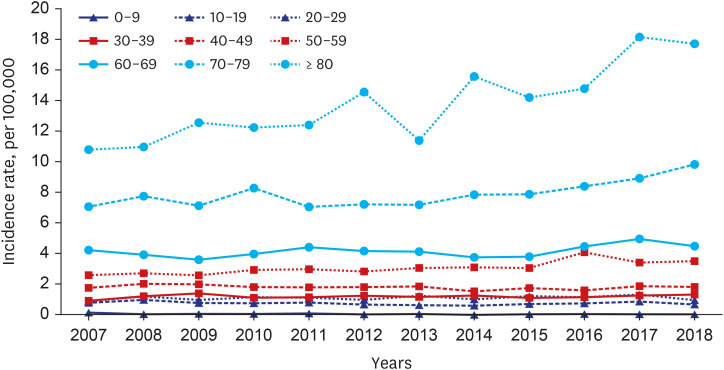
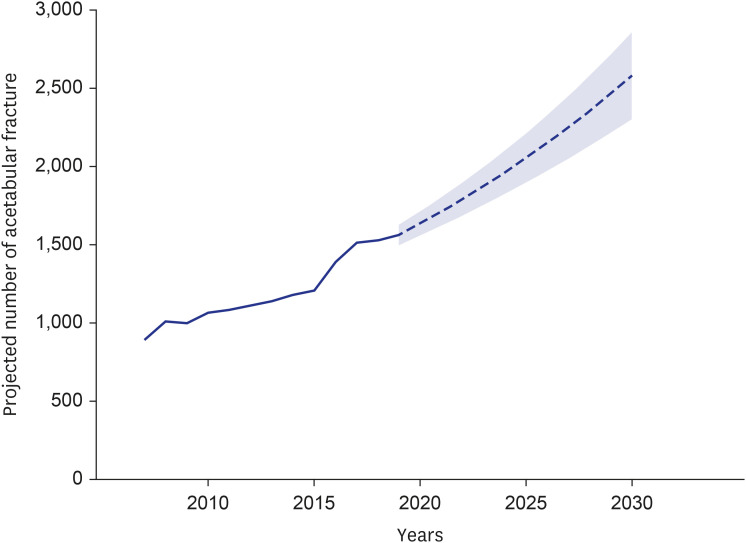
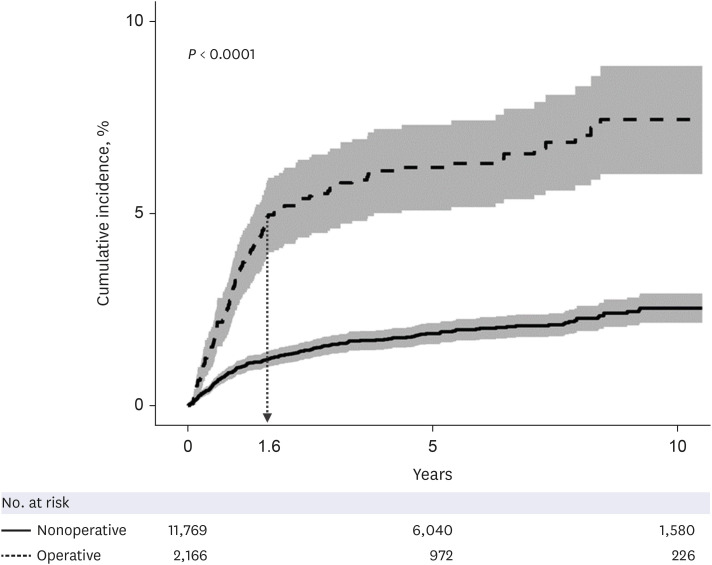
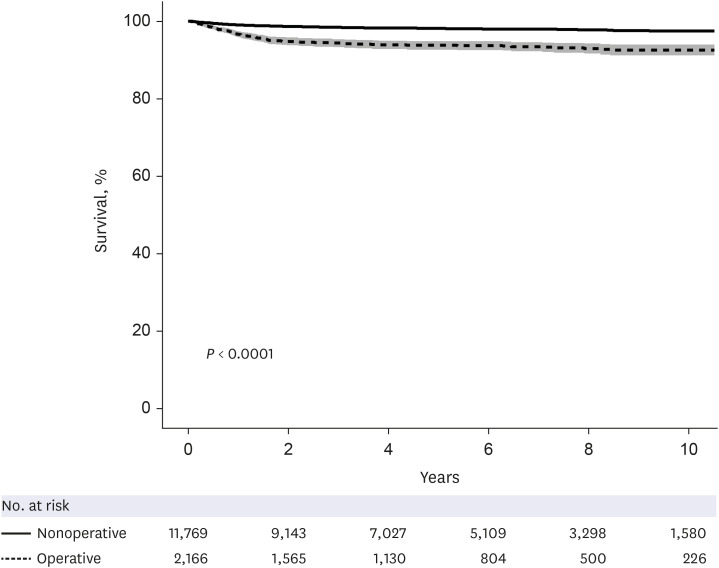
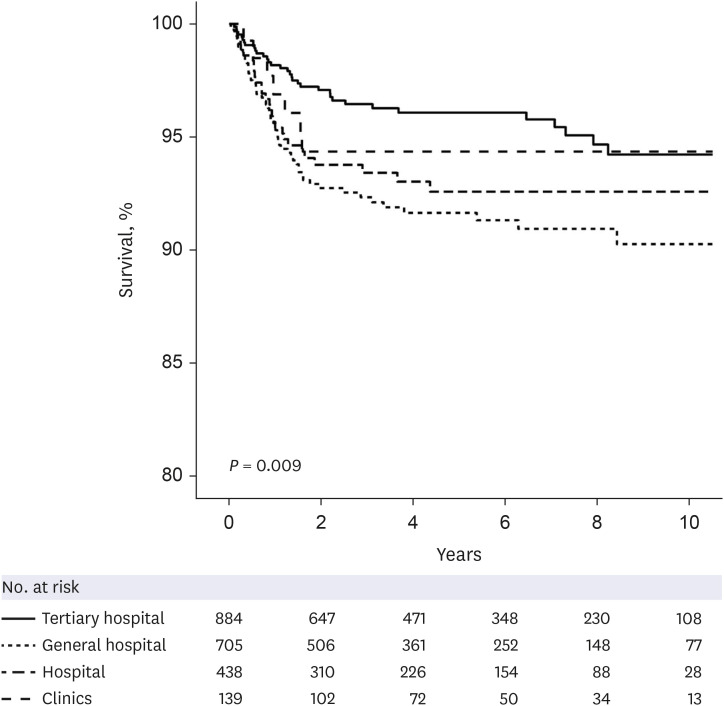
The incidence rate of acetabular fractures increased by 28% between 2007 and 2018. Acetabular fractures were more common in men (62%) than women (38%), and most common in the patients older than 80 years. The number of acetabular fractures was estimated to increase 1.7-fold in 2030 compared to 2018. Operative treatment accounted for 16% of cases, and nonoperative treatment for 84%. The incidence of subsequent THA was higher in the operative treatment group than in the nonoperative group (P < 0.001). The higher rate in the operative treatment group is probably related with the severity of the fracture type. The rate of subsequent THA was higher in patients who initially treated in general hospitals compared with those who were initially treated in tertiary hospitals.
Conclusion
The incidence of acetabular fractures is increasing in South Korea, in line with global trends. Most acetabular fractures are treated conservatively, and those who receive surgery are more likely to require a subsequent THA. Patients who were operated in general hospitals had highest possibility of subsequent THA after acetabular fractures.
Figure
Reference
-
1. Dalal SA, Burgess AR, Siegel JH, Young JW, Brumback RJ, Poka A, et al. Pelvic fracture in multiple trauma: classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma. 1989; 29(7):981–1000. PMID: 2746708.2. Giannoudis PV, Pohlemann T, Bircher M. Pelvic and acetabular surgery within Europe: the need for the co-ordination of treatment concepts. Injury. 2007; 38(4):410–415. PMID: 17397845.3. Briffa N, Pearce R, Hill AM, Bircher M. Outcomes of acetabular fracture fixation with ten years’ follow-up. J Bone Joint Surg Br. 2011; 93-B(2):229–236.4. Gary JL, Lefaivre KA, Gerold F, Hay MT, Reinert CM, Starr AJ. Survivorship of the native hip joint after percutaneous repair of acetabular fractures in the elderly. Injury. 2011; 42(10):1144–1151. PMID: 20850738.5. Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005; 87-B(1):2–9.6. Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010; 92-B(2):250–257.7. Laird A, Keating JF. Acetabular fractures: a 16-year prospective epidemiological study. J Bone Joint Surg Br. 2005; 87-B(7):969–973.8. Olson SA, Matta JM. The computerized tomography subchondral arc: a new method of assessing acetabular articular continuity after fracture (a preliminary report). J Orthop Trauma. 1993; 7(5):402–413. PMID: 8229376.9. Matta JM, Anderson LM, Epstein HC, Hendricks P. Fractures of the acetabulum. A retrospective analysis. Clin Orthop Relat Res. 1986; (205):230–240.10. Spencer RF. Acetabular fractures in older patients. J Bone Joint Surg Br. 1989; 71-B(5):774–776.11. Sen RK, Veerappa LA. Long-term outcome of conservatively managed displaced acetabular fractures. J Trauma. 2009; 67(1):155–159. PMID: 19590327.12. Jauregui JJ, Weir TB, Chen JF, Johnson AJ, Sardesai NR, Maheshwari AV, et al. Acute total hip arthroplasty for older patients with acetabular fractures: a meta-analysis. J Clin Orthop Trauma. 2020; 11(6):976–982. PMID: 33191999.13. Rickman M, Young J, Trompeter A, Pearce R, Hamilton M. Managing acetabular fractures in the elderly with fixation and primary arthroplasty: aiming for early weightbearing. Clin Orthop Relat Res. 2014; 472(11):3375–3382. PMID: 24452793.14. Ahmed M, Abuodeh Y, Alhammoud A, Salameh M, Hasan K, Ahmed G. Epidemiology of acetabular fractures in Qatar. Int Orthop. 2018; 42(9):2211–2217. PMID: 29430606.15. Hsieh SL, Lin TL, Lo YS, Chen CY, Chang HW, Chen HT, et al. Trends and treatments of pelvic and acetabular fractures in Taiwan: facing an aging society. Arch Osteoporos. 2023; 18(1):66. PMID: 37162585.16. Lundin N, Huttunen TT, Berg HE, Marcano A, Felländer-Tsai L, Enocson A. Increasing incidence of pelvic and acetabular fractures. A nationwide study of 87,308 fractures over a 16-year period in Sweden. Injury. 2021; 52(6):1410–1417. PMID: 33771345.17. Melhem E, Riouallon G, Habboubi K, Gabbas M, Jouffroy P. Epidemiology of pelvic and acetabular fractures in France. Orthop Traumatol Surg Res. 2020; 106(5):831–839. PMID: 32019733.18. Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD. Acetabular fractures in patients aged > 55 years: a systematic review of the literature. Bone Joint J. 2014; 96-B(2):157–163. PMID: 24493178.19. Shaker F, Esmaeili S, Nakhjiri MT, Azarboo A, Shafiei SH. The outcome of conversion total hip arthroplasty following acetabular fractures: a systematic review and meta-analysis of comparative studies. J Orthop Surg. 2024; 19(1):83.20. Dias MV, Goldsztajn F, Guimarães JM, Grizendi JA, Correia M, Rocha TH. Epidemiology of acetabulum fractures treated at the Instituto Nacional De Traumatologia E Ortopedia (INTO). Rev Bras Ortop. 2010; 45(5):474–477. PMID: 27022597.21. Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011; 173(6):676–682. PMID: 21330339.22. Park JW, Won SH, Moon SY, Lee YK, Ha YC, Koo KH. Burden and future projection of revision total hip arthroplasty in South Korea. BMC Musculoskelet Disord. 2021; 22(1):375. PMID: 33888097.23. Best MJ, Buller LT, Quinnan SM. Analysis of Incidence and outcome predictors for patients admitted to US hospitals with acetabular fractures from 1990 to 2010. Am J Orthop (Belle Mead NJ). 2018; 47(9):24. Rinne PP, Laitinen MK, Huttunen T, Kannus P, Mattila VM. The incidence and trauma mechanisms of acetabular fractures: a nationwide study in Finland between 1997 and 2014. Injury. 2017; 48(10):2157–2161. PMID: 28807429.25. Alvarez-Nebreda ML, Weaver MJ, Uribe-Leitz T, Heng M, McTague MF, Harris MB. Epidemiology of pelvic and acetabular fractures in the USA from 2007 to 2014. Osteoporos Int. 2023; 34(3):527–537. PMID: 36577845.26. Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M. Epidemiology of osteoporotic pelvic fractures in elderly people in Finland: sharp increase in 1970-1997 and alarming projections for the new millennium. Osteoporos Int. 2000; 11(5):443–448. PMID: 10912847.27. Guerado E, Cano JR, Cruz E. Occult acetabular fracture in elderly patients. Open Orthop J. 2012; 6(1):582–586. PMID: 23284595.28. Kakar R, Sharma H, Allcock P, Sharma P. Occult acetabular fractures in elderly patients: a report of three cases. J Orthop Surg (Hong Kong). 2007; 15(2):242–244. PMID: 17709871.29. Lee MJ, Ho SW, Kwek EB. Occult acetabular fractures in the elderly: a report of three cases and review of literature. Ann Acad Med Singapore. 2017; 46(10):404–409. PMID: 29177370.30. Cawthon PM. Gender differences in osteoporosis and fractures. Clin Orthop Relat Res. 2011; 469(7):1900–1905. PMID: 21264553.31. Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010; 152(6):380–390. PMID: 20231569.32. Hawkes WG, Wehren L, Orwig D, Hebel JR, Magaziner J. Gender differences in functioning after hip fracture. J Gerontol A Biol Sci Med Sci. 2006; 61(5):495–499. PMID: 16720747.33. Tornetta P 3rd. Displaced acetabular fractures: indications for operative and nonoperative management. J Am Acad Orthop Surg. 2001; 9(1):18–28. PMID: 11174160.34. Walley KC, Appleton PT, Rodriguez EK. Comparison of outcomes of operative versus non-operative treatment of acetabular fractures in the elderly and severely comorbid patient. Eur J Orthop Surg Traumatol. 2017; 27(5):689–694. PMID: 28389758.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- New Radiologic Projection for Acetabular Rim
- Anterior Approach for the Acetabular Fractures
- Total Hip Arthroplasty after Acetabular Fracture: Acute Phase and Delayed Phase
- Clinical Characteristics of Acetabular Fractures in Motor Vehicle Accident According to Tile's Classification
- Radiographic findings of acetabular fractures