J Korean Med Sci.
2024 Jul;39(25):e196. 10.3346/jkms.2024.39.e196.
Beyond Legal Boundaries: Public and Clinician Perspectives on Treatment Withdrawal in Infants With Poor Neurological Prognosis
- Affiliations
-
- 1Department of Pediatrics, Severance Children’s Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Integrative Care Hub, Seoul National University Hospital, Seoul, Korea
- 3Department of Pediatrics, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 4Center for Palliative Care and Clinical Ethics, Seoul National University Hospital, Seoul, Korea
- 5Department of Psychiatry, Chungnam National University Hospital, Daejeon, Korea
- 6Department of Psychiatry, Chungnam National University College of Medicine, Daejeon, Korea
- 7Department of Psychiatry, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2557771
- DOI: http://doi.org/10.3346/jkms.2024.39.e196
Abstract
- Background
Despite medical advancements in neonatal survival rates, many children have poor neurological outcomes. Because the law in Korea restricts the withdrawal of lifesustaining treatment to only cases of imminent death, treatment discontinuation may not be an option, even in patients with poor neurological prognosis. This study investigated the opinions of the general population and clinicians regarding life-sustaining treatment withdrawal in such cases using hypothetical scenarios.
Methods
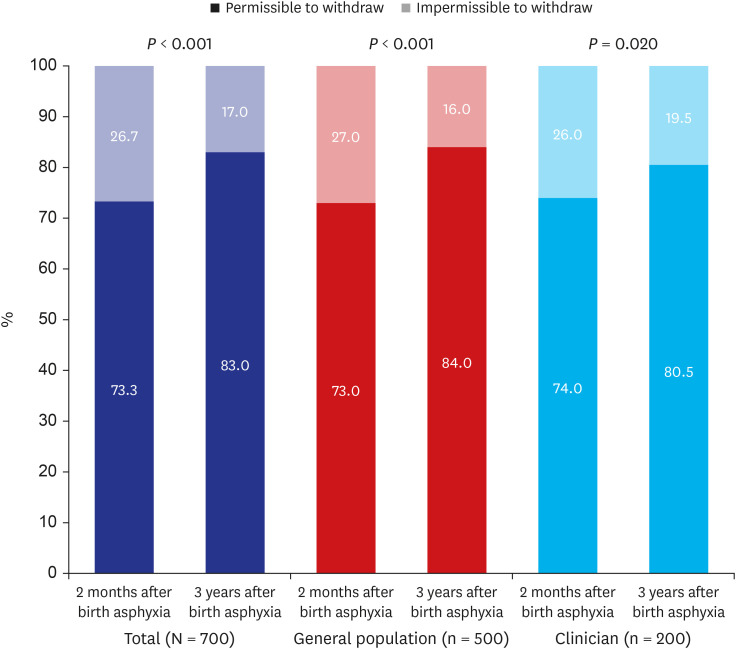
We conducted a cross-sectional study on the general population and clinicians using a web-based questionnaire. The sample of the general population from an online panel comprised 500 individuals aged 20–69 years selected by quota sampling. The clinician sample comprised 200 clinicians from a tertiary university hospital. We created hypothetical vignettes and questionnaire items to assess attitudes regarding mechanical ventilation withdrawal for an infant at risk of poor neurological prognosis due to birth asphyxia at 2 months and 3 years after the incidence.
Results
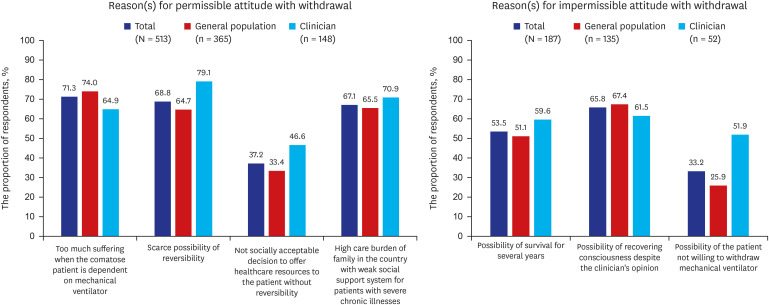
Overall, 73% of the general population and 74% of clinicians had positive attitudes toward mechanical ventilator withdrawal at 2 months after birth asphyxia. The proportion of positive attitudes toward mechanical ventilator withdrawal was increased in the general population (84%, P < 0.001) and clinicians (80.5%, P = 0.02) at 3 years after birth asphyxia. Religion, spirituality, the presence of a person with a disability in the household, and household income were associated with the attitudes of the general population. In the multivariable logistic regression analysis of the general population, respondents living with a person with a disability or having a disability were more likely to find the withdrawal of the ventilator at 2 months and 3 years after birth asphyxia not permissible. Regarding religion, respondents who identified as Christians were more likely to find the ventilator withdrawal at 2 months after birth asphyxia unacceptable.
Conclusion
The general population and clinicians shared the perspective that the decision to withdraw life-sustaining treatment in infants with a poor neurological prognosis should be considered before the end of life. A societal discussion about making decisions centered around the best interest of pediatric patients is warranted.
Keyword
Figure
Reference
-
1. Lee JH, Noh OK, Chang YS. Korean Neonatal Network. Neonatal outcomes of very low birth weight infants in Korean neonatal network from 2013 to 2016. J Korean Med Sci. 2019; 34(5):e40. PMID: 30718992.2. Kim CH, Song IG, Kim MS, Lee JY, Lim NG, Shin HY. Healthcare utilization among children and young people with life-limiting conditions: exploring palliative care needs using National Health Insurance claims data. Sci Rep. 2020; 10(1):2692. PMID: 32060337.3. Kim MS, Lim NG, Kim HJ, Kim C, Lee JY. Pediatric deaths attributed to complex chronic conditions over 10 years in Korea: evidence for the need to provide pediatric palliative care. J Korean Med Sci. 2018; 33(1):e1. PMID: 29215810.4. Yoo SH, Kim Y, Choi W, Shin J, Kim MS, Park HY, et al. Ethical issues referred to clinical ethics support at a university hospital in Korea: three-year experience after enforcement of Life-Sustaining Treatment Decisions Act. J Korean Med Sci. 2023; 38(24):e182. PMID: 37337807.5. Heo DS. Life-sustaining medical treatment for terminal patients in Korea. J Korean Med Sci. 2013; 28(1):1–3. PMID: 23341705.6. Kim Y, Lim CM, Shim TS, Hong SB, Huh JW, Oh D, et al. The influence of new legislation on the withdrawal of life-sustaining treatment on the perceptions and experiences of residents in a tertiary hospital in Korea. Korean J Med Ethics. 2020; 23(4):279–299.7. Lee HY, Kim HJ, Kwon JH, Baek SK, Won YW, Kim YJ, et al. The situation of life-sustaining treatment one year after enforcement of the Act on Decisions on Life-Sustaining Treatment for patients at the end-of-life in Korea: data of National Agency for Management of Life-Sustaining Treatment. Cancer Res Treat. 2021; 53(4):897–907. PMID: 34082496.8. Diekema DS, Mercurio MR, Adam MB. Clinical Ethics in Pediatrics: A Case-Based Textbook. Cambridge, UK: Cambridge University Press;2011.9. American Academy of Pediatrics Committee on Fetus and Newborn. Bell EF. Noninitiation or withdrawal of intensive care for high-risk newborns. Pediatrics. 2007; 119(2):401–403. PMID: 17272630.10. Korea Ministry of Government Legislation. Act on Decisions on Life-Sustaining Treatment for Patients in Hospice and Palliative Care or at the End of Life. Sejong, Korea: Korean Law Information Center;2016.11. Choi YH, Kim MS, Kim CH, Song IG, Park JD, In Suh D, et al. Looking into the life of technology-dependent children and their caregivers in Korea: lifting the burden of too many responsibilities. BMC Pediatr. 2020; 20(1):486. PMID: 33081719.12. Korean National Index. Trend of median income in Korea. Accessed February 8, 2023. https://www.index.go.kr/unity/potal/main/EachDtlPageDetail.do?idx_cd=2762 .13. Macauley RC. Ethics in Palliative Care: A Complete Guide. Oxford, UK: Oxford University Press;2018. p. 306–310.14. Lin M, Deming R, Wolfe J, Cummings C. Infant mode of death in the neonatal intensive care unit: a systematic scoping review. J Perinatol. 2022; 42(5):551–568. PMID: 35058594.15. Weiner J, Sharma J, Lantos J, Kilbride H. How infants die in the neonatal intensive care unit: trends from 1999 through 2008. Arch Pediatr Adolesc Med. 2011; 165(7):630–634. PMID: 21727274.16. Verhagen AA, Janvier A, Leuthner SR, Andrews B, Lagatta J, Bos AF, et al. Categorizing neonatal deaths: a cross-cultural study in the United States, Canada, and The Netherlands. J Pediatr. 2010; 156(1):33–37. PMID: 19772968.17. Lemmon ME, Boss RD, Bonifacio SL, Foster-Barber A, Barkovich AJ, Glass HC. Characterization of death in neonatal encephalopathy in the hypothermia era. J Child Neurol. 2017; 32(4):360–365. PMID: 28193115.18. Natarajan G, Mathur A, Zaniletti I, DiGeronimo R, Lee KS, Rao R, et al. Withdrawal of life-support in neonatal hypoxic-ischemic encephalopathy. Pediatr Neurol. 2019; 91:20–26. PMID: 30559002.19. Al Amrani F, Racine E, Shevell M, Wintermark P. Death after birth asphyxia in the cooling era. J Pediatr. 2020; 226:289–293. PMID: 32682749.20. Kim MJ, Lee JH, Lee HD. Recent changes in end-of-life decisions for newborns in a Korean hospital. Am J Hosp Palliat Care. 2018; 35(4):574–578. PMID: 28905637.21. Park GY, Kim SS. Deaths in the neonatal intensive care unit between 2002 and 2014. Neonatal Med. 2016; 23(1):8–15.22. Wilkinson DJ. A life worth giving? The threshold for permissible withdrawal of life support from disabled newborn infants. Am J Bioeth. 2011; 11(2):20–32.23. Chiang FM, Hsieh JG, Fan SY, Wang YW, Wang SC. Does the experience of caring for a severely disabled relative impact advance care planning? A qualitative study of caregivers of disabled patients. Int J Environ Res Public Health. 2020; 17(5):1594. PMID: 32121624.24. Tanaka M, Kodama S, Lee I, Huxtable R, Chung Y. Forgoing life-sustaining treatment - a comparative analysis of regulations in Japan, Korea, Taiwan, and England. BMC Med Ethics. 2020; 21(1):99. PMID: 33066771.25. Liao YS, Tsai WC, Chiu LT, Kung PT. Effects of the time of hospice and palliative care enrollment before death on morphine, length of stay, and healthcare expense in patients with cancer in Taiwan. Healthcare (Basel). 2023; 11(21):2867. PMID: 37958010.26. Scott-Joynt M. Withdrawal of life-sustaining treatment for newborn infants from a Christian perspective. Early Hum Dev. 2012; 88(2):89–90. PMID: 22257827.27. Chung GS, Yoon JD, Rasinski KA, Curlin FA. US physicians’ opinions about distinctions between withdrawing and withholding life-sustaining treatment. J Relig Health. 2016; 55(5):1596–1606. PMID: 26725047.28. Sprung CL, Maia P, Bulow HH, Ricou B, Armaganidis A, Baras M, et al. The importance of religious affiliation and culture on end-of-life decisions in European intensive care units. Intensive Care Med. 2007; 33(10):1732–1739. PMID: 17541550.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Public and Clinician Perspectives on Ventilator Withdrawal in Vegetative State Following Severe Acute Brain Injury: A Vignette Survey
- A Tale of Two Fields: Mathematical and Statistical Modeling of Infectious Diseases
- A Period of Storm and Stress
- Sound in the Air
- Can Stigma Still Distort the Spectrum of a Disease?