Cancer Res Treat.
2024 Jul;56(3):945-955. 10.4143/crt.2023.1205.
CD19-Specific CAR-T Cell Treatment of 115 Children and Young Adults with Acute B Lymphoblastic Leukemia: Long-term Follow-up
- Affiliations
-
- 1Department of Pediatrics, Peking University People’s Hospital, Peking University, Beijing, China
- KMID: 2557681
- DOI: http://doi.org/10.4143/crt.2023.1205
Abstract
- Purpose
Chemotherapy has been the primary treatment for patients with B-cell acute lymphoblastic leukemia (B-ALL). However, there are still patients who are not sensitive to chemotherapy, including those with refractory/relapse (R/R) disease and those experiencing minimal residual disease (MRD) re-emergence. Chimeric antigen receptor-T lymphocytes (CAR-T) therapy may provide a new treatment option for these patients.
Materials and Methods
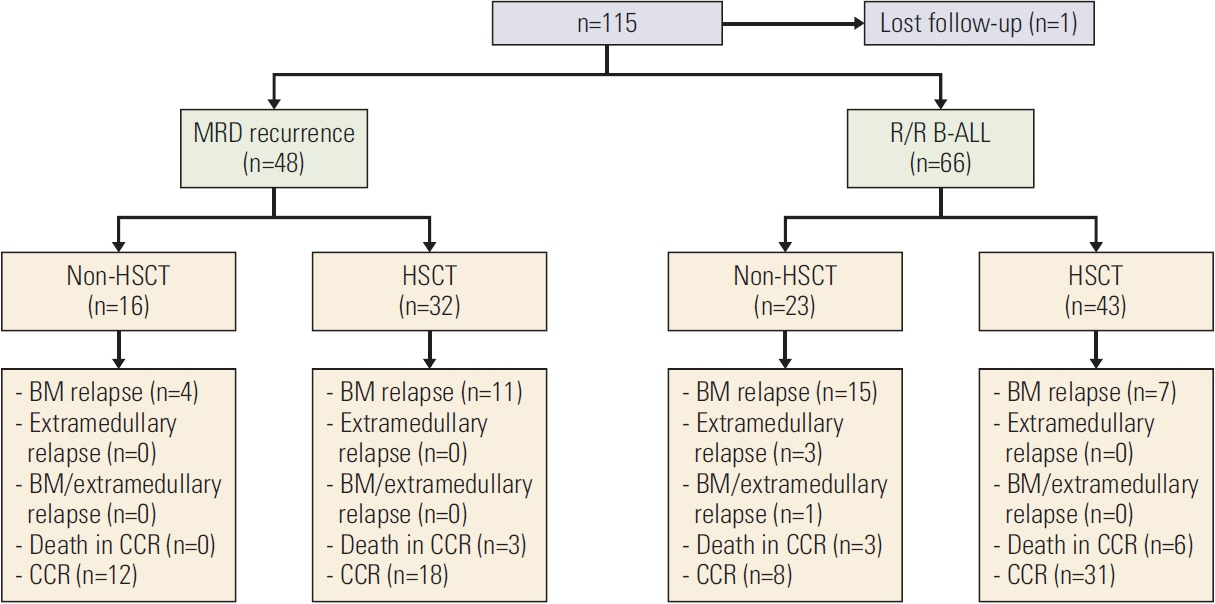
Our institution conducted a single-arm prospective clinical trial (ChiCTR-OPN-17013507) using CAR-T-19 to treat R/R B-ALL and MRD re-emergent patients. One hundred and fifteen patients, aged 1-25 years (median age, 8 years), were enrolled, including 67 R/R and 48 MRD re-emergent CD19-positive B-ALL patients.
Results
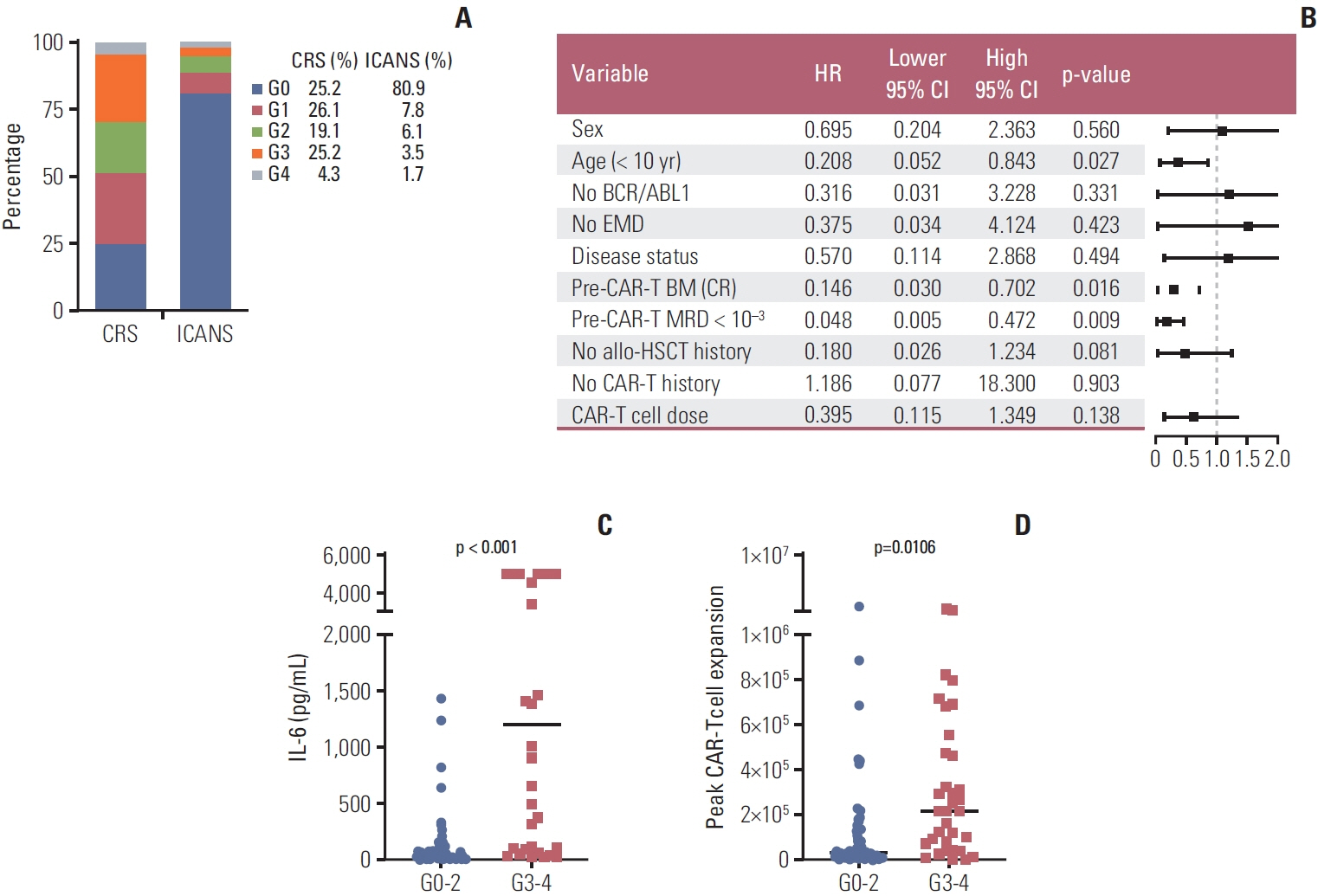
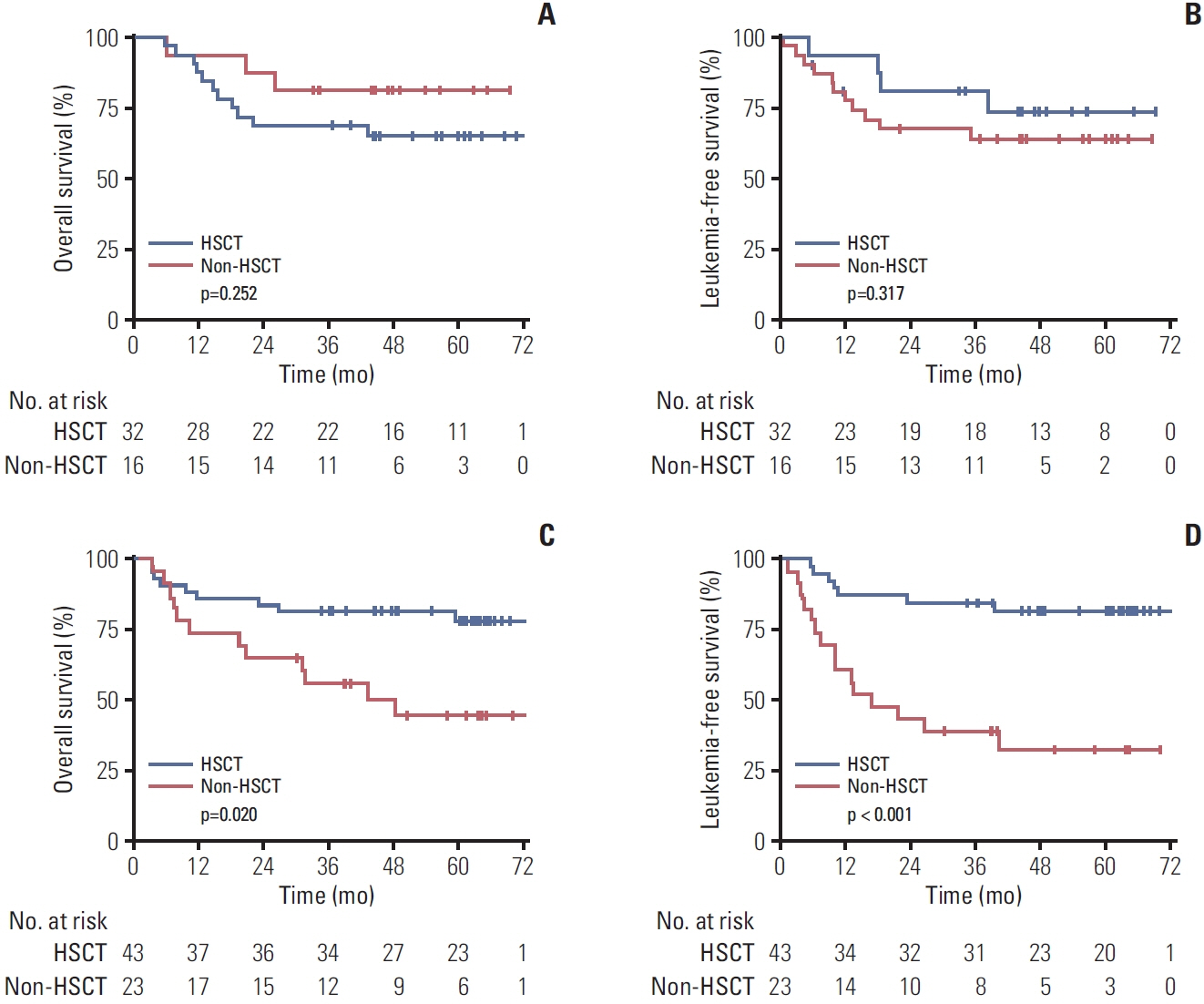
All patients achieved morphologic complete remission (CR), and within 1 month after infusion, 111 out of 115 (96.5%) patients achieved MRD-negative CR. With a median follow-up time of 48.4 months, the estimated 4-year leukemia-free survival (LFS) rate and overall survival (OS) rate were 68.7%±4.5% and 70.7%±4.3%, respectively. There were no significant differences in long-term efficacy observed among patients with different disease statuses before infusion (4-year OS: MRD re-emergence vs. R/R B-ALL, 70.6%±6.6% vs. 66.5%±6.1%, p=0.755; 4-year LFS: MRD re-emergence vs. R/R B-ALL, 67.3%±7.0% vs. 63.8%±6.2%, p=0.704). R/R B-ALL patients bridging to transplantation after CAR-T treatment had a superior OS and LFS compared to those who did not. However, for MRD re-emergent patients, there was no significant difference in OS and LFS, regardless of whether they underwent hematopoietic stem cell transplantation or not.
Conclusion
CD19 CAR-T therapy effectively and safely cures both R/R B-ALL and MRD re-emergent patients.
Keyword
Figure
Reference
-
References
1. Yu CH, Jou ST, Su YH, Coustan-Smith E, Wu G, Cheng CN, et al. Clinical impact of minimal residual disease and genetic subtypes on the prognosis of childhood acute lymphoblastic leukemia. Cancer. 2023; 129:790–802.
Article2. Cui L, Li ZG, Chai YH, Yu J, Gao J, Zhu XF, et al. Outcome of children with newly diagnosed acute lymphoblastic leukemia treated with CCLG-ALL 2008: The first nation-wide prospective multicenter study in China. Am J Hematol. 2018; 93:913–20.
Article3. Koh KN, Im HJ, Kim H, Kang HJ, Park KD, Shin HY, et al. Outcome of reinduction chemotherapy with a modified dose of idarubicin for children with marrow-relapsed acute lymphoblastic leukemia: results of the Childhood Acute Lymphoblastic Leukemia (CALL)-0603 Study. J Korean Med Sci. 2017; 32:642–9.
Article4. Wang Y, Xue YJ, Jia YP, Zuo YX, Lu AD, Zhang LP. Re-emergence of minimal residual disease detected by flow cytometry predicts an adverse outcome in pediatric acute lymphoblastic leukemia. Front Oncol. 2020; 10:596677.
Article5. Li Z, Yang K, Song Y, Zhao Y, Wu F, Wen X, et al. CAR-T therapy followed by allogeneic hematopoietic stem cell transplantation for refractory/relapsed acute B lymphocytic leukemia: Long-term follow-up results. Front Oncol. 2022; 12:1048296.
Article6. Park JH, Riviere I, Gonen M, Wang X, Senechal B, Curran KJ, et al. Long-term follow-up of CD19 CAR therapy in acute lymphoblastic leukemia. N Engl J Med. 2018; 378:449–59.
Article7. Zhang X, Yang J, Li J, Li W, Song D, Lu XA, et al. Factors associated with treatment response to CD19 CAR-T therapy among a large cohort of B cell acute lymphoblastic leukemia. Cancer Immunol Immunother. 2022; 71:689–703.
Article8. An F, Wang H, Liu Z, Wu F, Zhang J, Tao Q, et al. Influence of patient characteristics on chimeric antigen receptor T cell therapy in B-cell acute lymphoblastic leukemia. Nat Commun. 2020; 11:5928.
Article9. Hay KA, Gauthier J, Hirayama AV, Voutsinas JM, Wu Q, Li D, et al. Factors associated with durable EFS in adult B-cell ALL patients achieving MRD-negative CR after CD19 CAR T-cell therapy. Blood. 2019; 133:1652–63.
Article10. Hu GH, Zhao XY, Zuo YX, Chang YJ, Suo P, Wu J, et al. Unmanipulated haploidentical hematopoietic stem cell transplantation is an excellent option for children and young adult relapsed/refractory Philadelphia chromosome-negative B-cell acute lymphoblastic leukemia after CAR-T-cell therapy. Leukemia. 2021; 35:3092–100.
Article11. Hu GH, Cheng YF, Zuo YX, Chang YJ, Suo P, Wu J, et al. Chimeric antigens receptor T cell therapy improve the prognosis of pediatric acute lymphoblastic leukemia with persistent/recurrent minimal residual disease in first complete remission. Front Immunol. 2021; 12:731435.
Article12. Lee DW, Santomasso BD, Locke FL, Ghobadi A, Turtle CJ, Brudno JN, et al. ASTCT consensus grading for cytokine release syndrome and neurologic toxicity associated with immune effector cells. Biol Blood Marrow Transplant. 2019; 25:625–38.
Article13. Zhang X, Lu XA, Yang J, Zhang G, Li J, Song L, et al. Efficacy and safety of anti-CD19 CAR T-cell therapy in 110 patients with B-cell acute lymphoblastic leukemia with high-risk features. Blood Adv. 2020; 4:2325–38.
Article14. Shah NN, Lee DW, Yates B, Yuan CM, Shalabi H, Martin S, et al. Long-term follow-up of CD19-CAR T-cell therapy in children and young adults with B-ALL. J Clin Oncol. 2021; 39:1650–9.
Article15. Eldfors S, Kuusanmaki H, Kontro M, Majumder MM, Parsons A, Edgren H, et al. Idelalisib sensitivity and mechanisms of disease progression in relapsed TCF3-PBX1 acute lymphoblastic leukemia. Leukemia. 2017; 31:51–7.
Article16. Lenk L, Alsadeq A, Schewe DM. Involvement of the central nervous system in acute lymphoblastic leukemia: opinions on molecular mechanisms and clinical implications based on recent data. Cancer Metastasis Rev. 2020; 39:173–87.
Article17. Xu X, Sun Q, Liang X, Chen Z, Zhang X, Zhou X, et al. Mechanisms of relapse after CD19 CAR T-cell therapy for acute lymphoblastic leukemia and its prevention and treatment strategies. Front Immunol. 2019; 10:2664.
Article18. Zhang X, Li JJ, Lu PH. Advances in the development of chimeric antigen receptor-T-cell therapy in B-cell acute lymphoblastic leukemia. Chin Med J (Engl). 2020; 133:474–82.
Article19. Pui CH, Pei D, Coustan-Smith E, Jeha S, Cheng C, Bowman WP, et al. Clinical utility of sequential minimal residual disease measurements in the context of risk-based therapy in childhood acute lymphoblastic leukaemia: a prospective study. Lancet Oncol. 2015; 16:465–74.
Article20. Pemmaraju N, Kantarjian H, Jorgensen JL, Jabbour E, Jain N, Thomas D, et al. Significance of recurrence of minimal residual disease detected by multi-parameter flow cytometry in patients with acute lymphoblastic leukemia in morphological remission. Am J Hematol. 2017; 92:279–85.21. Winters A, Gore L. Moving immunotherapy into the front line in ALL. Hematology Am Soc Hematol Educ Program. 2019; 2019:209–17.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of adverse events in young adults and children with acute B-cell lymphoblastic leukemia receiving anti-CD19 chimeric antigen receptor (CAR) T-cell therapy
- Adolescents and young adults (AYA) with acute lymphoblastic leukemia
- Treatment of CD19-Positive Mixed Phenotype Acute Leukemia with Blinatumomab
- Precursor B-Cell Acute Lymphoblastic Leukemia in Two Patients with a History of Cytotoxic Therapy
- Optimal therapy for adolescents and young adults with acute lymphoblastic leukemia-current perspectives