J Korean Assoc Oral Maxillofac Surg.
2024 Jun;50(3):166-169. 10.5125/jkaoms.2024.50.3.166.
Customized spacers in provisional treatment of temporomandibular joint ankylosis: a case report
- Affiliations
-
- 1Oral and Maxillofacial Surgery Residency Program, Hospital Governador Celso Ramos, Florianópolis, Brazil
- 2LabMAIS (Additive Manufacturing and Health Innovation Laboratory), IFSC (Federal Institute of Santa Catarina), Florianópolis, Brazil
- KMID: 2557634
- DOI: http://doi.org/10.5125/jkaoms.2024.50.3.166
Abstract
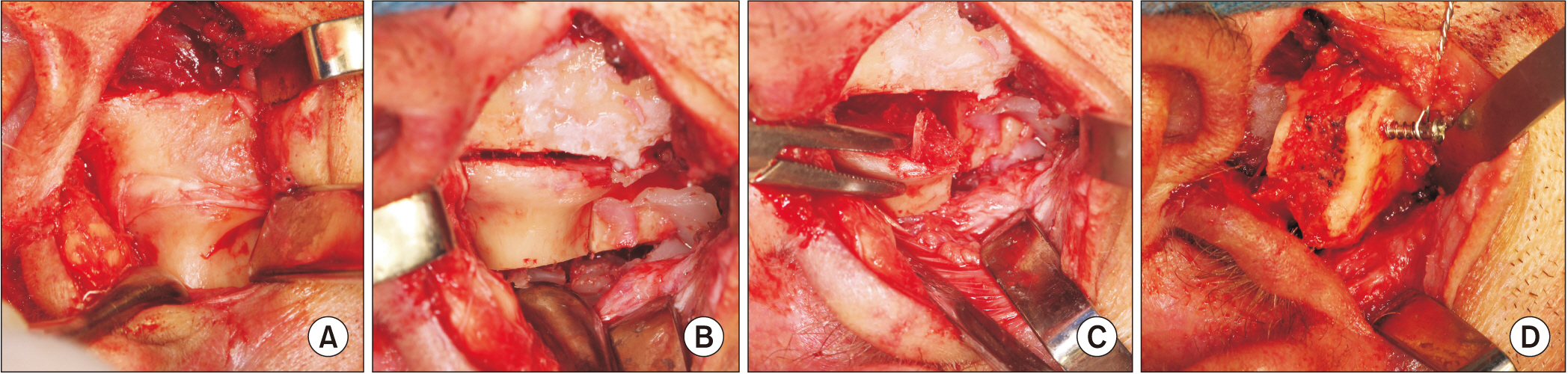
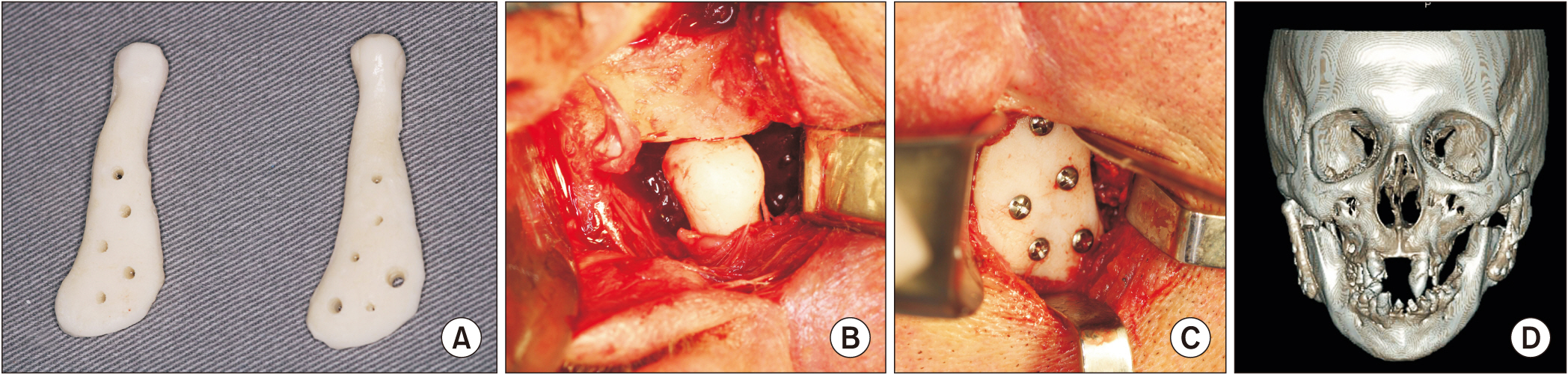
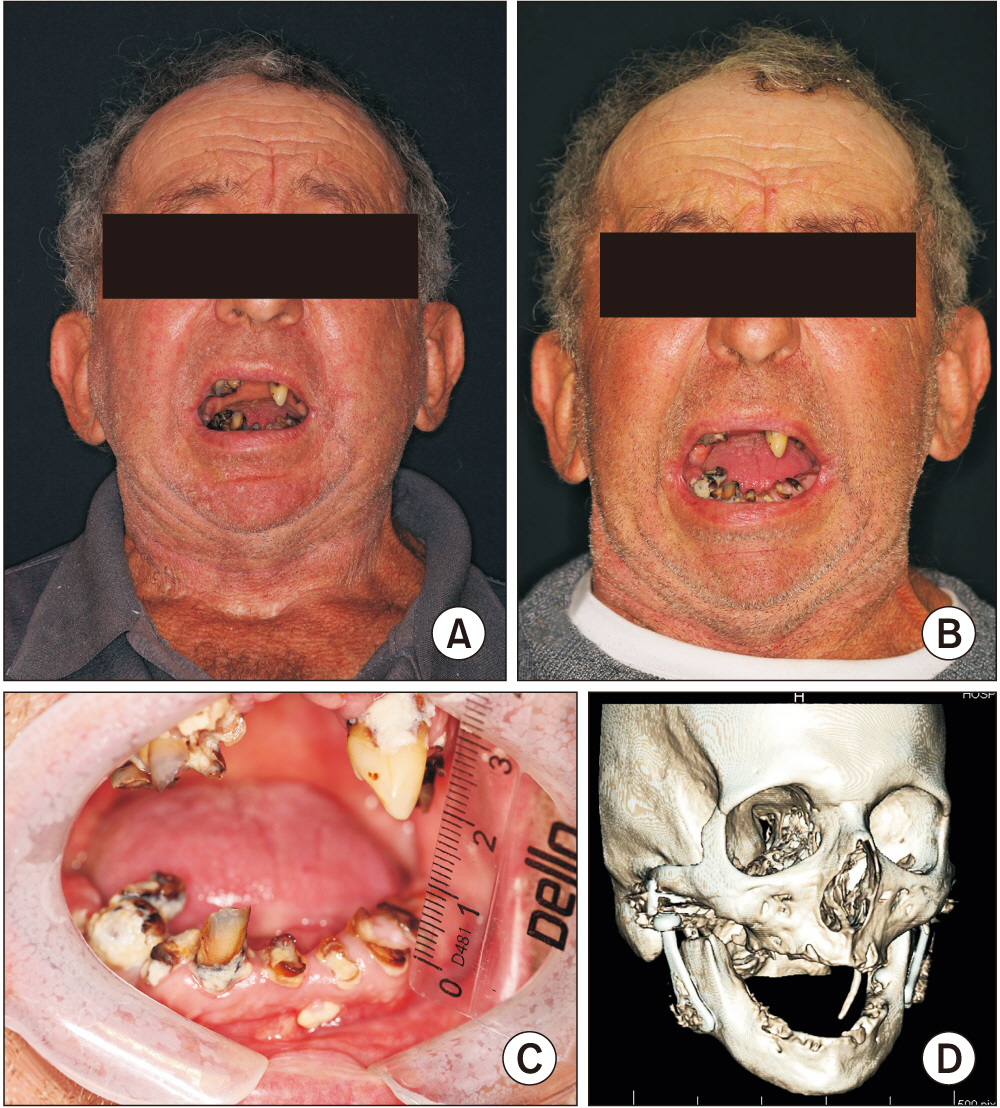
- Ankylosis of the temporomandibular joint (TMJ) is a condition in which the mandibular condyle fuses with the mandibular fossa through fibrous or bone tissue. It is a debilitating pathology that interferes with chewing, speaking, and oral hygiene. Currently, alloplastic reconstruction is considered the gold standard for treating severely compromised TMJs, such as in ankylosis. The article describes a patient with a history of facial trauma, with bilateral ankylosis of the TMJs, inability to open his mouth, and poor dental condition. Due to a long period of immobilization of approximately 40 years, the initial treatment plan was to remove the ankylosis bilaterally and install customized PMMA (polymethylmethacrylate) spacers. The patient gained mouth opening and improved chewing quality with one year of customized spacer use prior to definitive alloplastic replacement with stock-type TMJ prostheses. Customized joint spacers are a provisional treatment option when definitive alloplastic reconstruction is not indicated. Spacers provide the patient with progressive jaw function and mobility gains.
Figure
Reference
-
References
1. Wolford L, Movahed R, Teschke M, Fimmers R, Havard D, Schneiderman E. 2016; Temporomandibular joint ankylosis can be successfully treated with TMJ concepts patient-fitted total joint prosthesis and autogenous fat grafts. J Oral Maxillofac Surg. 74:1215–27. https://doi.org/10.1016/j.joms.2016.01.017. DOI: 10.1016/j.joms.2016.01.017. PMID: 26878364.
Article2. Lotesto A, Miloro M, Mercuri LG, Sukotjo C. 2017; Status of alloplastic total temporomandibular joint replacement procedures performed by members of the American Society of Temporomandibular Joint Surgeons. Int J Oral Maxillofac Surg. 46:93–6. https://doi.org/10.1016/j.ijom.2016.08.002. DOI: 10.1016/j.ijom.2016.08.002. PMID: 27567049.
Article3. Green JM 3rd, Lawson ST, Liacouras PC, Wise EM, Gentile MA, Grant GT. 2016; Custom anatomical 3D spacer for temporomandibular joint resection and reconstruction. Craniomaxillofac Trauma Reconstr. 9:82–7. https://doi.org/10.1055/s-0035-1546814. DOI: 10.1055/s-0035-1546814. PMID: 26889353. PMCID: PMC4755798.
Article4. Teschke M, Christensen A, Far F, Reich RH, Naujokat H. 2021; Digitally designed, personalized bone cement spacer for staged TMJ and mandibular reconstruction - introduction of a new technique. J Craniomaxillofac Surg. 49:935–42. https://doi.org/10.1016/j.jcms.2021.05.002. DOI: 10.1016/j.jcms.2021.05.002. PMID: 34238634.
Article5. Puricelli E. 2022; Puricelli biconvex arthroplasty as an alternative for temporomandibular joint reconstruction: description of the technique and long-term case report. Head Face Med. 18:27. https://doi.org/10.1186/s13005-022-00331-4. DOI: 10.1186/s13005-022-00331-4. PMID: 35906643. PMCID: PMC9335964.
Article6. Sinn DP, Tandon R, Tiwana PS. 2021; Can alloplastic total temporomandibular joint reconstruction be used in the growing patient? A preliminary report. J Oral Maxillofac Surg. 79:2267.e1–16. https://doi.org/10.1016/j.joms.2021.06.022. DOI: 10.1016/j.joms.2021.06.022. PMID: 34339614.
Article7. Kong L, Mei J, Ge W, Jin X, Chen X, Zhang X, et al. 2021; Application of 3D printing-assisted articulating spacer in two-stage revision surgery for periprosthetic infection after total knee arthroplasty: a retrospective observational study. Biomed Res Int. 2021:3948638. https://doi.org/10.1155/2021/3948638. DOI: 10.1155/2021/3948638. PMID: 33628779. PMCID: PMC7884112.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Temporomandibular Joint Disorder by Alloplastic Total Temporomandibular Joint Replacement
- Difficult airway management in a case with lingual tonsil hypertrophy and temporo-mandibular joint partial ankylosis
- Temporomandibular joint re-ankylosis: a case report and literature review
- Airway Management for General Anesthesia in a Patient with Severe Trismus due to Temporomandibular Joint Ankylosis : A case report
- Temporomandibular joint bony ankylosis following postoperative radiotherapy for maxillary cancer