J Korean Assoc Oral Maxillofac Surg.
2024 Jun;50(3):161-165. 10.5125/jkaoms.2024.50.3.161.
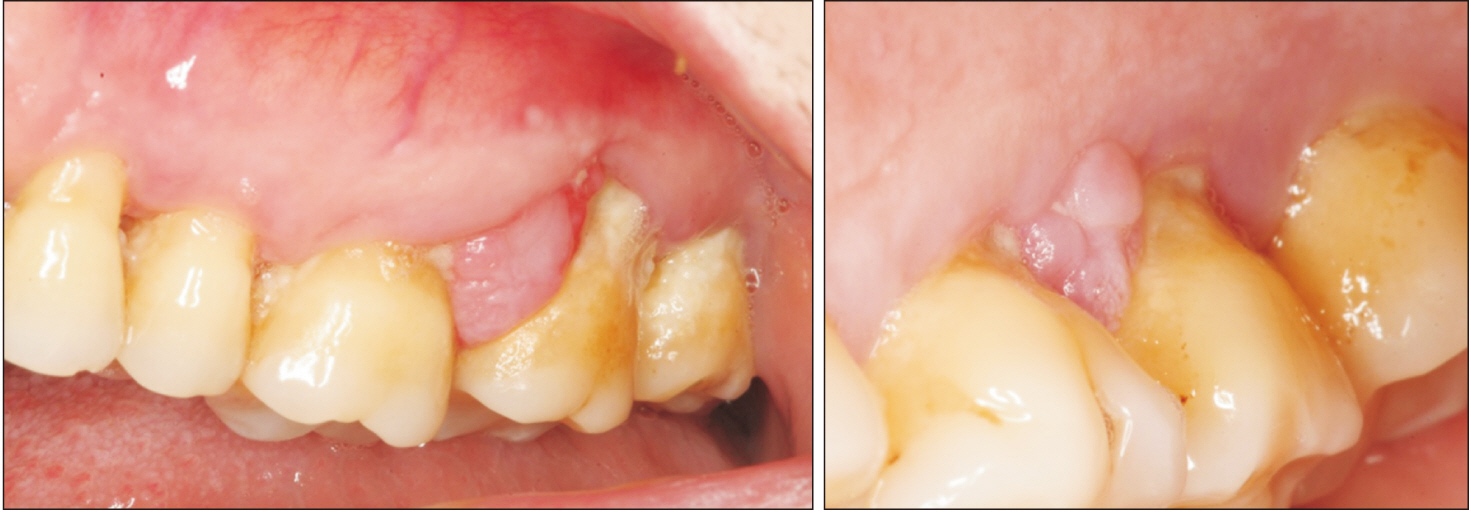
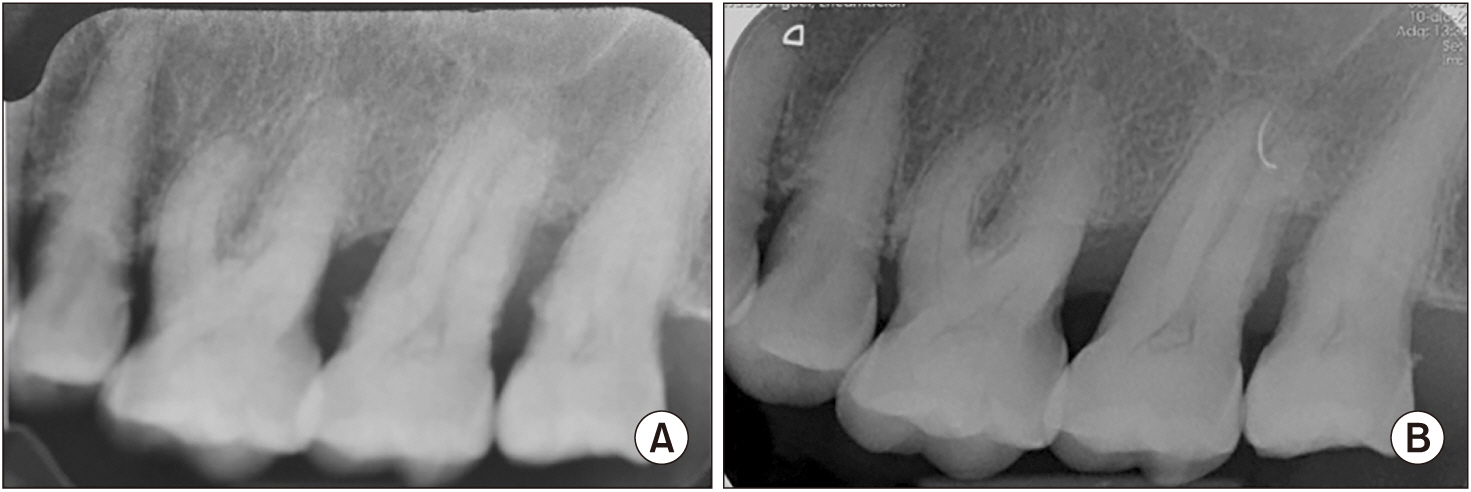
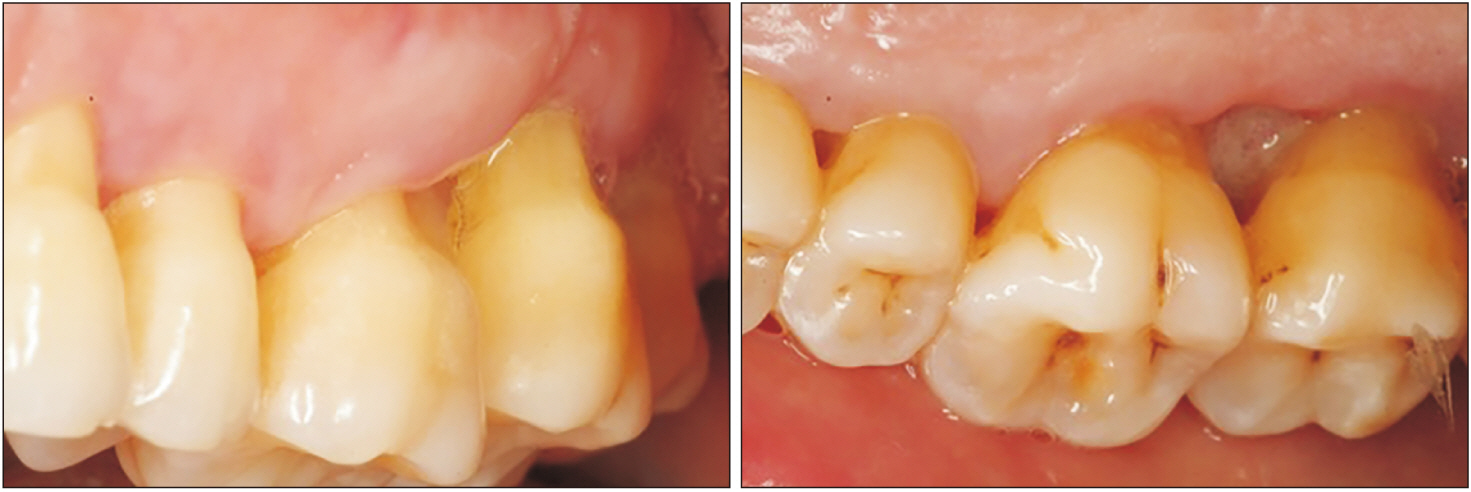
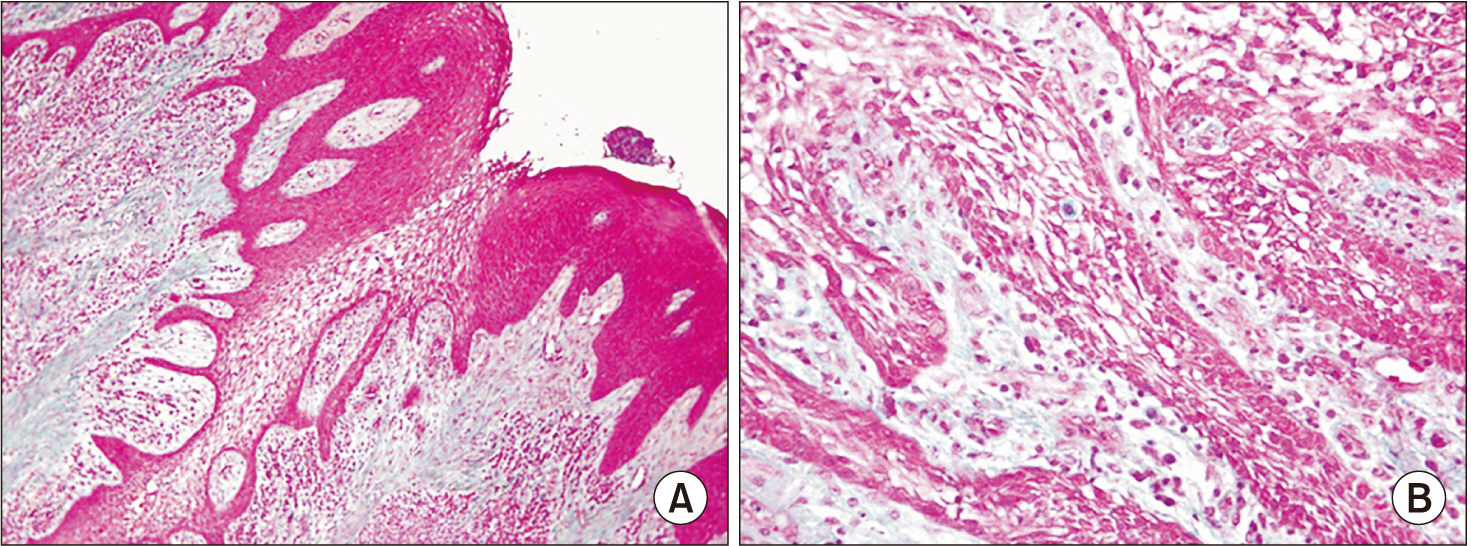
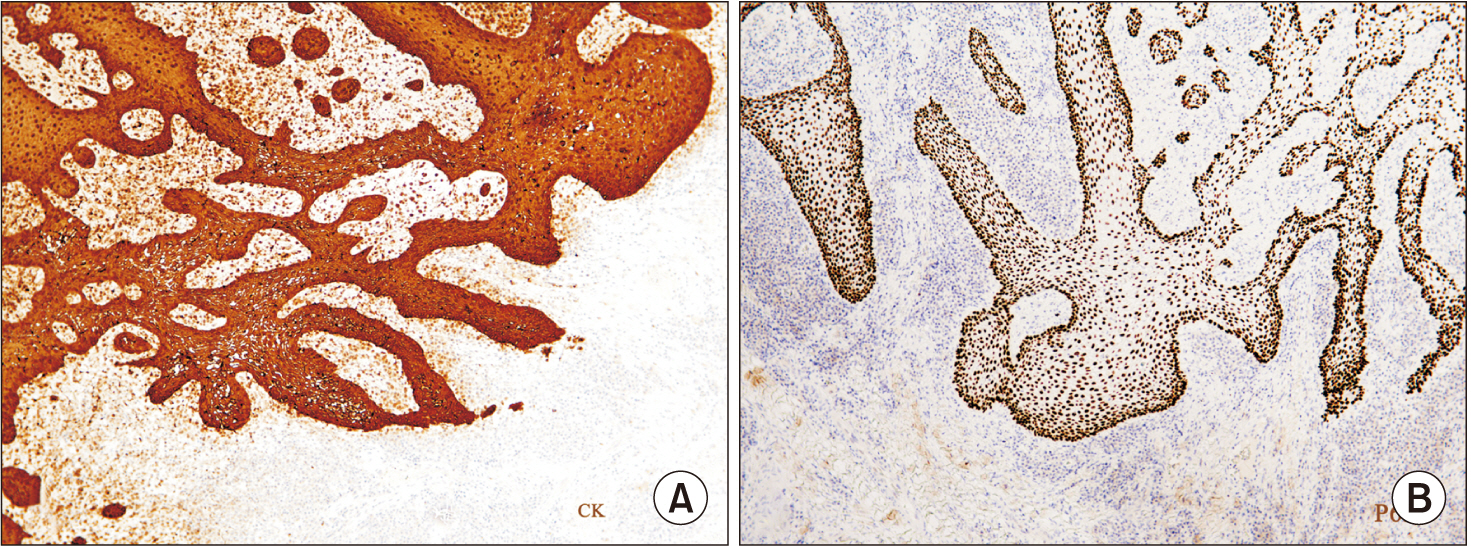
An unusual presentation of peripheral ameloblastoma in the maxilla
- Affiliations
-
- 1Department of Oral Surgery, Implantology and Periodontics, Faculty of Dentistry, Universidad Alfonso X el Sabio, Madrid, Spain
- 2Department of Dental Clinical Specialties, Faculty of Dentistry, Universidad Complutense de Madrid, Madrid, Spain
- 3Doctoral Programme in Surgery and Odontostomatology, University of Alcalá de Henares, Alcalá de Henares, Madrid, Spain
- 4Department of Surgery, Faculty of Medicine, Dental Clinic, University of Salamanca, Salamanca, Spain
- KMID: 2557633
- DOI: http://doi.org/10.5125/jkaoms.2024.50.3.161
Abstract
- Peripheral ameloblastoma (PA) is believed to be the rarest variant of ameloblastoma and only has been described in isolated case reports. PA is usually confined to the soft tissues surrounding the supporting tissues of the teeth. Although it manifests nonaggressive behavior and can be treated with complete removal by local surgical excision, long term follow up is mandatory to prevent future recurrence and possible malignant transformation.
Figure
Cited by 2 articles
-
Comment on “An unusual presentation of peripheral ameloblastoma in the maxilla”
Heitor Albergoni Silveira, Marcelo Borges Marques, Jorge Esquiche León
J Korean Assoc Oral Maxillofac Surg. 2024;50(5):303-304. doi: 10.5125/jkaoms.2024.50.5.303.Author’s reply to the letter to the editor of Journal of the Korean Association of Oral and Maxillofacial Surgeons
Rosa María Acevedo Ocaña
J Korean Assoc Oral Maxillofac Surg. 2024;50(5):305-306. doi: 10.5125/jkaoms.2024.50.5.305.
Reference
-
References
1. Philipsen HP, Reichart PA, Nikai H, Takata T, Kudo Y. 2001; Peripheral ameloblastoma: biological profile based on 160 cases from the literature. Oral Oncol. 37:17–27. https://doi.org/10.1016/s1368-8375(00)00064-6. DOI: 10.1016/S1368-8375(00)00064-6. PMID: 11120479.
Article2. Gardner DG. 1984; A pathologistʼs approach to the treatment of ameloblastoma. J Oral Maxillofac Surg. 42:161–6. https://doi.org/10.1016/s0278-2391(84)80026-9. DOI: 10.1016/S0278-2391(84)80026-9. PMID: 6583361.
Article3. Baden E, Doyle JL, Petriella V. 1993; Malignant transformation of peripheral ameloblastoma. Oral Surg Oral Med Oral Pathol. 75:214–9. https://doi.org/10.1016/0030-4220(93)90096-m. DOI: 10.1016/0030-4220(93)90096-M. PMID: 8426721.
Article4. Zhang X, Tian X, Hu Y, Zhang C, Wei C, Yang X. 2018; Oral peripheral ameloblastoma: a retrospective series study of 25 cases. Med Oral Patol Oral Cir Bucal. 23:e277–81. https://doi.org/10.4317/medoral.22225. DOI: 10.4317/medoral.22225. PMID: 29680843. PMCID: PMC5945233.
Article5. El-Mofty SK, Gerard NO, Farish SE, Rodu B. 1991; Peripheral ameloblastoma: a clinical and histologic study of 11 cases. J Oral Maxillofac Surg. 49:970–4. discussion 974–5. https://doi.org/10.1016/0278-2391(91)90061-p. DOI: 10.1016/0278-2391(91)90061-P. PMID: 1886025.
Article6. Kishino M, Murakami S, Yuki M, Iida S, Ogawa Y, Kogo M, et al. 2007; A immunohistochemical study of the peripheral ameloblastoma. Oral Dis. 13:575–80. https://doi.org/10.1111/j.1601-0825.2006.01340.x. DOI: 10.1111/j.1601-0825.2006.01340.x. PMID: 17944675.
Article7. Nonaka CF, de Oliveira PT, de Medeiros AM, de Souza LB, Freitas RA. 2013; Peripheral ameloblastoma in the maxillary gingiva: a case report. N Y State Dent J. 79:37–40.8. Ochsenius G, Ortega A, Godoy L, Peñafiel C, Escobar E. 2002; Odontogenic tumors in Chile: a study of 362 cases. J Oral Pathol Med. 31:415–20. https://doi.org/10.1034/j.1600-0714.2002.00073.x. DOI: 10.1034/j.1600-0714.2002.00073.x. PMID: 12165060.
Article9. Buchner A, Merrell PW, Carpenter WM. 2006; Relative frequency of peripheral odontogenic tumors: a study of 45 new cases and comparison with studies from the literature. J Oral Pathol Med. 35:385–91. https://doi.org/10.1111/j.1600-0714.2006.00437.x. DOI: 10.1111/j.1600-0714.2006.00437.x. PMID: 16827840.
Article10. Moskow BS, Baden E. 1982; The peripheral ameloblastoma of the gingiva. Case report and literature review. J Periodontol. 53:736–42. https://doi.org/10.1902/jop.1982.53.12.736. DOI: 10.1902/jop.1982.53.12.736. PMID: 6961202.
Article11. Mintz S, Anavi Y, Sabes WR. 1990; Peripheral ameloblastoma of the gingiva. A case report. J Periodontol. 61:649–52. https://doi.org/10.1902/jop.1990.61.10.649. DOI: 10.1902/jop.1990.61.10.649. PMID: 2231232.
Article12. Chae MP, Smoll NR, Hunter-Smith DJ, Rozen WM. 2015; Establishing the natural history and growth rate of ameloblastoma with implications for management: systematic review and meta-analysis. PLoS One. 10:e0117241. https://doi.org/10.1371/journal.pone.0117241. DOI: 10.1371/journal.pone.0117241. PMID: 25706407. PMCID: PMC4338260.
Article13. Bologna-Molina R, Mosqueda-Taylor A, Lopez-Corella E, Almeida OP, Carrasco-Daza D, Garcia-Vazquez F, et al. 2008; Syndecan-1 (CD138) and Ki-67 expression in different subtypes of ameloblastomas. Oral Oncol. 44:805–11. https://doi.org/10.1016/j.oraloncology.2007.10.007. DOI: 10.1016/j.oraloncology.2007.10.007. PMID: 18207448.
Article14. Reichart PA, Philipsen HP, Sonner S. 1995; Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 31B:86–99. https://doi.org/10.1016/0964-1955(94)00037-5. DOI: 10.1016/0964-1955(94)00037-5. PMID: 7633291.
Article15. Wettan HL, Patella PA, Freedman PD. 2001; Peripheral ameloblastoma: review of the literature and report of recurrence as severe dysplasia. J Oral Maxillofac Surg. 59:811–5. https://doi.org/10.1053/joms.2001.24302. DOI: 10.1053/joms.2001.24302. PMID: 11429748.
Article